Review Article - Current Pediatric Research (2025) Volume 29, Issue 2
Diagnostic stewardship and reasoning for the management of neonatal sepsis.
Daniel Geleta1*, Gemeda Abebe1, Netsanet Workneh2, Getenet Beyene1
1Department of Health Sciences, Jimma University, Jimma, Ethiopia
2Department of Pediatrics and Child Health, Jimma University, Jimma, Ethiopia
- Corresponding Author:
- Daniel Geleta
Department of Health Sciences, Jimma University, Jimma, Ethiopia,
Email: daniel@ju.edu.et
Received: 26-Jul-2024, Manuscript No. AAJCP-24-143274; Editor assigned: 29-Jul-2024, AAJCP-24-143274 (PQ); Reviewed: 12-Aug-2024, QC No. AAJCP-24-143274; Revised: 09-Feb-2025, Manuscript No. AAJCP-24-143274 (R); Published: 16-Feb-2025, DOI: 10.35841/0971-9032.29.02.1-6
Abstract
The healthcare system faces numerous challenges and contradictions when it comes to preventable or treatable sepsis in newborns. Diagnostic errors, testing methods and clinical management approaches significantly contribute to the high morbidity and mortality rates associated with neonatal sepsis. These issues persistently trouble healthcare providers, prompting recent efforts to introduce diagnostic stewardship and reasoning as effective strategies to enhance neonatal outcomes. Diagnostic stewardship is a new concept aimed at streamlining the healthcare system and optimizing diagnostic pathways for neonatal sepsis diagnosis. It focuses on determining the reasons, timing and necessity of diagnostic tests and procedures. Consequently, diagnostic stewardship plays a critical role in ensuring accurate diagnoses for newborns when needed. Practical application of this concept has shown positive results when combined with computerized clinical decision support tools, direct feedback and real-time evaluations. Evidence consistently demonstrates the significant impact of diagnostic stewardship in saving lives, reducing medical expenses and improving survival rates for newborns. The implementation of diagnostic stewardship strategies has resulted in tangible benefits for healthcare outcomes, despite facing notable challenges that hinder its integration into clinical practice. Overcoming these obstacles is essential for realizing the full potential of diagnostic stewardship in enhancing healthcare outcomes. In conclusion, while diagnostic stewardship and reasoning offer promising improvements in diagnosing neonatal sepsis, their successful integration into healthcare systems requires substantial effort and thorough implementation research. By adopting these approaches and facilitating their implementation, healthcare systems can improve newborn health, lower costs and ultimately save more newborn lives.
Keywords
Diagnostic pathway, Diagnostic stewardship, Diagnostic reasoning; Diagnostic test, Neonatal care, Neonatal sepsis, Right test, Treatment outcome.
Introduction
Overview of neonatal health and neonatal sepsis
The survival of newborns is influenced by several factors, including the location of birth, the paradoxes within healthcare systems and the 60-30-10 dimension of healthcare facilities. Access to and affordability of high-quality healthcare services play a critical role in determining neonatal morbidity and mortality rates. Unfortunately, these tragedies are more common in hospital settings and are particularly pronounced in developing countries, primarily due to the prevalence of infectious diseases, including neonatal sepsis [1].
Despite ongoing efforts to address adverse neonatal conditions in healthcare facilities, the published literature reports a staggering number of annual neonatal mortalities, with approximately 2.5 million deaths occurring within the first 28 days of life. These deaths now account for 47% of all deaths in children under the age of five [2]. These numbers serve as a quantification of the burden of these conditions on the population and act as a reflection of the socioeconomic and health status of the community population. What is especially disheartening is that a significant portion, approximately 78%, of these neonatal mortalities results from causes that are preventable or treatable. However, amidst these preventable causes, neonatal sepsis-related mortality often goes unnoticed or becomes normalized in some developing countries.
Literature Review
In this document, the term "neonatal sepsis" refers to a clinical syndrome that is difficult to define and unsurprisingly, difficult to diagnose [3]. It is, however, known to be commonly caused by bacteria, viruses or fungi, usually before neonates celebrate their 28th birthday and remains a nuisance to clinicians. The condition makes the neonatal period the most perilous time for child survival and has remained a major global public health challenge for a variety of reasons [4]. The reasons include the ambiguous definition and diagnosis of the condition, neonate exposure to multiple iatrogenic risks, the inextricable link with maternal perinatal care and well-being, the lack of point-ofcare diagnostic tests, disparities in health care quality, institutional culture and climate, heterogeneity of the neonatal population and the coincidence of the sepsis with other neonatal conditions.
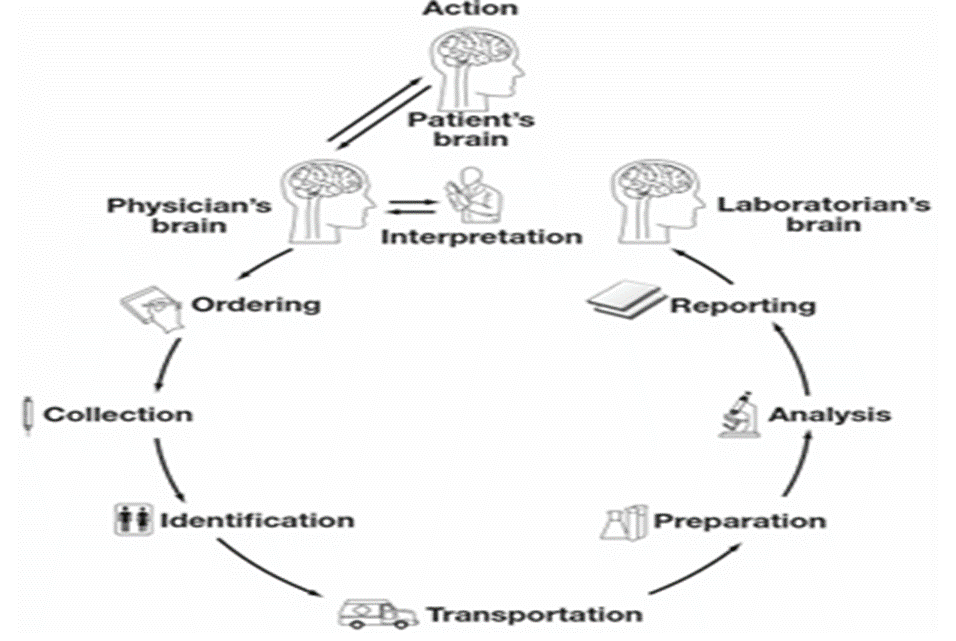
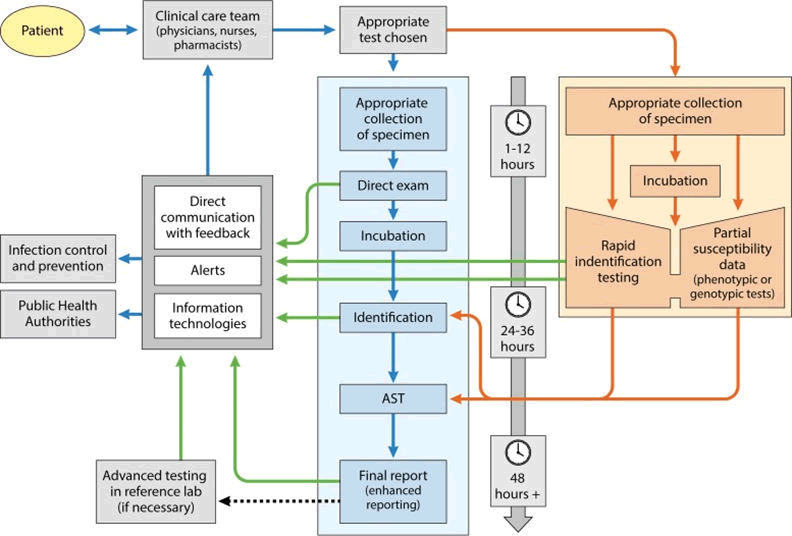
Currently, laboratory diagnostic tests help streamline neonatal care by strengthening the “brain-to-brain turnaround time loop” (Figure 1) and providing data on three basic concepts: Whether the neonate is infected, what type of infection it is, and what will help treat it [5]. Laboratory diagnostic testing has subsequently evolved into an important component of neonatal sepsis management as well as a rapidly advancing and widely recognized medical activity. Diagnostic testing acknowledged an important factor in hospital settings, accounting for 3%-15% of total health-care expenditures and influencing 70%-80% of clinical decisions. In neonatal sepsis, the approach delineates reasonable diagnostic modalities and the proper management, aiming improved neonatal outcomes by changing the dimensions of the modern health-care system [6].
Figure 1. The brain-to-brain turnaround time loop and its nine steps.
However, in a number of settings, laboratory diagnostics operates as an insular department, focusing almost entirely on its own silo. This trend resulted in diagnostic tests to exhibit errors in the pre and post-analytical phases of the overall testing process rather than the analytical phase. The exhibition then made Geisinger laboratory aware of the need to enhance diagnostic capabilities and fueled efforts to provide patients with high-quality care. The initiative resulted in the development of the diagnostic stewardship approach, which has recently gained popularity and is dedicated to balancing technical capability with the ability to apply it effectively and economically to neonatal sepsis. The current authors were also inspired to contribute to the initiative and prepared this paper. The paper provides a concise review of diagnostic stewardship and explains why diagnostic tests for suspected neonatal sepsis should be chosen with care.
Discussion
Overview of diagnostic stewardship in the management of neonatal sepsis
Healthcare systems are replacing fee-for-service models with value-based care, which emphasizes ordering tests and procedures that can lead to shorter hospital stays and better neonatal sepsis outcomes. The new model outlines critical components, such as clinical microbiology laboratories, to improve the overall brain-to-brain loop of diagnosis and treatment. The system intends to support the component with a diagnostic stewardship approach that ensures the "right test, for the right neonate, at the right time" [7]. Recent publications describe the diagnostic stewardship as a systemically integrated strategy for the effective use of microbiology laboratories for the delivery of safer, more effective and efficient patient care. The term refers to a novel concept and a growing field that focuses on coordinated interventions, with a particular emphasis on the integration of microbiological and molecular diagnostics at an earlier stage in neonatal care [8]. It has recently been recognized by journal publications as promoting prudent microbiology testing practices to support neonatal treatment decisions and is cited as the fit-for-purpose use of laboratory testing or more simply, keeping antibiotics safe by supervising the use of diagnostic tests.
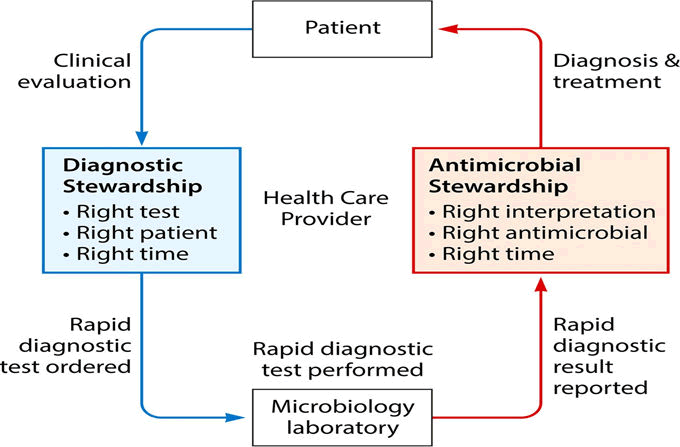
The concept of diagnostic stewardship encompasses all stages of the diagnostic process and ultimately aims to optimize patient care by improving the entire diagnostic process or component depicted in Figure 2.
Figure 2. Situation, component and interaction of diagnostic stewardship in clinical setting.
The approach purported to improve microbiology diagnostic test practices, reduce avoidable testing, improve the validity of test results and reduce antibiotic use. The approach strives to select the right test for the right patient and generate accurate, clinically relevant results at the right time and hence maximize value and reduce waste in the healthcare system [9]. The most important details are the appropriateness of the test (the right test), the impact of the test on newborn clinical treatment (the right neonate) and the prompt availability of the test result for the best possible patient care. Diagnostic stewardship encompasses all aspects of ordering, performing and reporting diagnostic tests during the preanalytical, analytical and postanalytical phases. It essentially supports to protect antibiotic resistance, provide top-notch clinical treatment, maximize antibiotic use and enhance newborn outcomes.
Basics and benefits of diagnostic stewardship in the management of neonatal sepsis
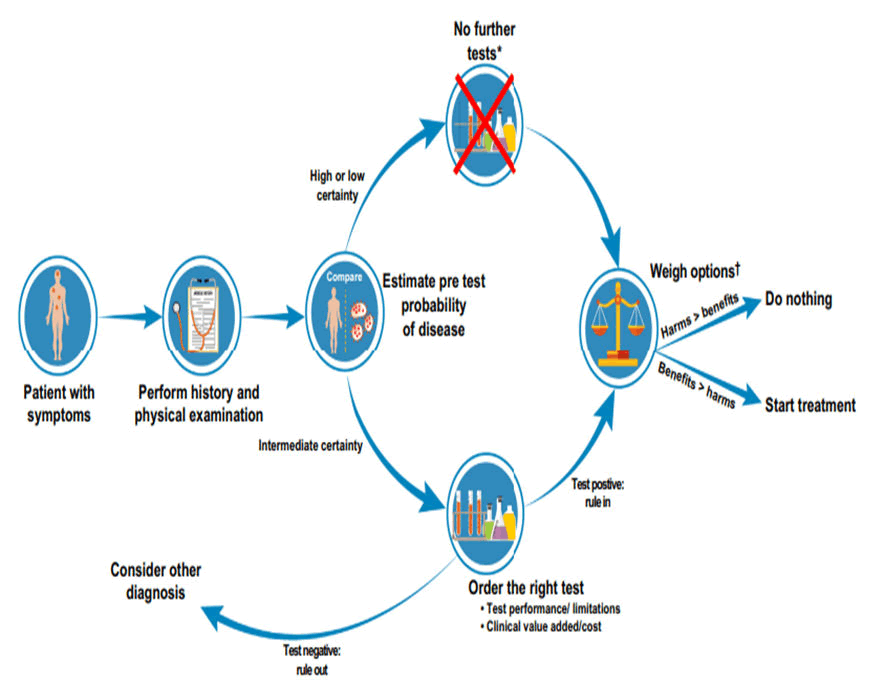
Improve accuracy of diagnoses: In fact, a good prescription starts with a precise diagnosis, and the precise diagnosis is ensured by true diagnostic test accuracy (sensitivity and specificity). On the other hand, diagnostic excellence has recently been accredited by the true north of diagnostic stewardship. A rapid microbiology laboratory response is a distinguishing feature in hospital settings, where it influences nearly 70% of clinical decisions and disease progression. This massive laboratory reliance results in diagnostic errors (missed, delayed and incorrect diagnoses) that occur nearly twice as frequently as other types of clinical errors. To reduce diagnostic error, diagnostic stewardship functions in the improvement of processes and diagnostic test essentials such as performance (depending on accuracy), deployability (performance and ease of use) and use-case (who is tested and why) (Figure 3) [10]. More recently, the diagnostic stewardship expanded to include components critical to excellent care delivery, such as diagnostic inelegancy, readiness, intervention and impact. It imposes microbial diagnostics to provide clinicians with refined information more quickly than ever before based on the concepts of supportive, actionable, quick turnaround time, population health prioritization and precision medicine.
Figure 3. A conceptual model for the ideal journey of diagnostic process.
The approach, particularly in clinical settings, focuses on an earlier stage of the neonatal case management process though the diagnostic intervention occurs at any phase. It encourages appropriate and timely diagnostic testing, including specimen collection, pathogen identification and accurate and timely results reporting. In general, diagnostic stewardship regulates the practices and procedures that guide specimen selection, collection and the completion of clinical, demographic and epidemiological data that must accompany each specimen. It targets strategies for better specimen storage and transportation, discusses how laboratories receive, register and process specimens, including how appropriate tests are selected and performed and then moves on to how results are reported and interpreted before being used to guide patient management. Based on the observations, diagnostic stewardship assists in determining the types of samples and diagnostic procedures required, as well as the patient groups that benefit from the specific testing. For example, if a neonate's diagnostic testing revealed viral etiology while on empirically indicated broad spectrum antibiotics, the result may allow antimicrobials to be discontinued sooner.
Reduce cost of care and risk of over-testing: According to neonatal sepsis guidelines, clinicians treat when infection is highly unlikely. The addition of rapid diagnostics is a muchneeded addition to overcome the standard's opinion. However, the cost of ordering these panels remains and testing guidelines have not caught up with new diagnostic technologies in determining who needs such tests. Accordingly, diagnostic stewardship was implemented, ensuring that lower-cost but potentially clinically useful laboratory testing remained in use. The diagnostic stewardship entails modifying the ordering process by nudging the ordering menu institution by institution. The diagnostic stewardship involves modifying the process of ordering diagnostic tests by nudging the ordering menu institution by institution. It encourages the use-case to define the feasibility and clinical significance of each use-case for neonates. The approach was studied in some countries with experience on diagnostic stewardship and found promising financial benefits of diagnostic stewardship initiatives. It entails making an effort to use diagnostic tests efficiently while eliminating unnecessary, ineffective, or even harmful testing. It also implies reducing the use of unnecessary tests, resulting in cost savings. It advocates the abolition of some high-cost tests with dubious clinical values and the exclusion of unnecessary tests. The diagnostic stewardship program for children reduced unnecessary tests and cost expenditure, reducing the test frequency for the identification of infectious agents and shortening antimicrobial utilization.
Improve neonatal treatment outcomes: Diagnostic stewardship emphasizes streamlining the diagnosis process and reducing the time to optimal therapy as quickly as possible, potentially leading to more optimal treatment outcomes. The initiative improves patient safety by promoting accurate diagnosis and supplementing antimicrobial stewardship. It extends antimicrobial stewardship and is well-known for combating antibiotic resistance by optimizing antimicrobial selection and reducing antibiotic overuse. It ensures that the appropriate test is performed on the appropriate patient in order to use the appropriate drug at the appropriate time, dose and duration, all while minimizing neonatal harm.
Furthermore, in several countries, the diagnostic stewardship program contributes to the development of antibiotic use guidelines by ensuring the accuracy and credibility of data generated by microbiology labs and it is used as a team sport to improve intervention implementation and effect measurement.
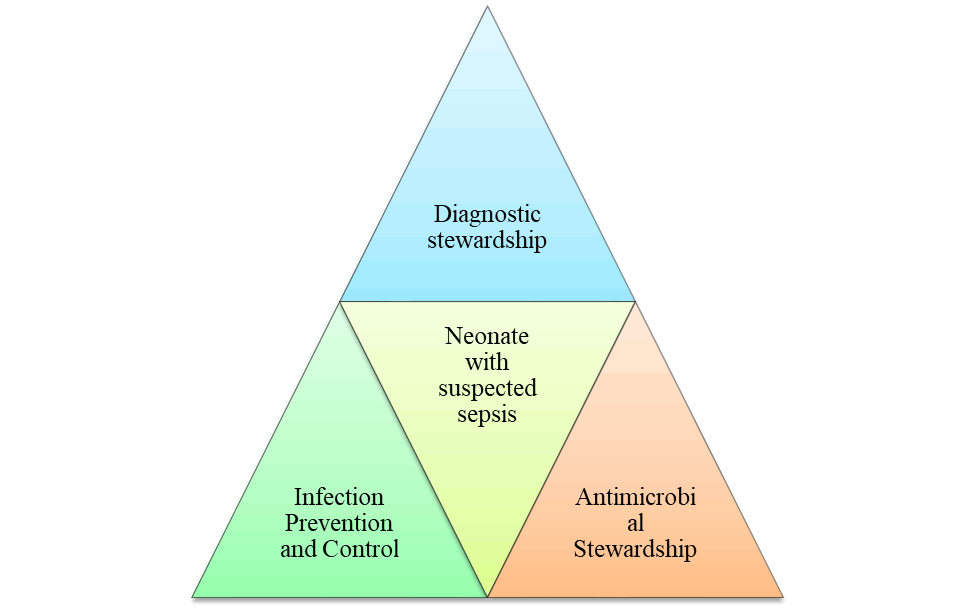
In addition, it collaborated with programs like antimicrobial stewardship, infection prevention and control (Figure 4) and the microbiology laboratories. It then enhanced the use of antibiotics and restricted the emergence and spread of antibiotic resistance, thereby lessening the need for needless treatment.
Figure 4. The interlace of diagnostic stewardship, antimicrobial stewardship and infection prevention and control programs to influence neonatal treatment outcomes.
Applications of diagnostic stewardship in the management of neonatal sepsis
The first step in the application of diagnostic stewardship is to develop the theoretical framework (Figure 5) on how the outcomes of diagnostic tests impact patient treatment and outcome. In the second step, define the roles and responsibilities of those involved in diagnostic stewardship, particularly for the clinician and microbiologist. Hereto, the clinician should always be briefed on three interconnected points: The signs and symptoms of the infectious process, the availability of the optimal diagnostic test to evaluate the infection and the method of collecting the diagnostic specimen to optimize the result. Clinical microbiologists promote appropriate diagnostic methods and support method selection while mentoring workflow pathways to improve result communication, as given in Figure 5. In the pathway under Figure 5, blue, orange and green arrows, respectively, represent the conventional microbiology pathway, the rapid diagnostic pathway and opportunities for the diagnostic stewardship teams to improve communication of results.
Figure 5. Workflow pathways in conventional microbiology and rapid diagnostic test in clinical setting
In the complex pathway, the microbiologist must collaborate with a diverse range of health professionals and lead multidisciplinary committees to design diagnostic algorithms, improve the laboratory computer system, train staff and strengthen the role of other clinical microbiologists in managing infectious diseases. The microbiologist is also accountable for recognizing the significance of diagnostic stewardship in areas such as decision support, readiness, intervention, speed, accessibility, impact and safety. The microbiologist must also show that the new tests support the minimum standards for antimicrobial stewardship programs, offer actionable test results in both inpatient and outpatient settings, have a quick turnaround, reduce the spread of infection during onsite testing and exhibit good precision medicine.
In practice, diagnostic stewardship has shown the highest success rate in the presence of computerized clinical decision support interventions, face-to-face feedback and real-time evaluations. The diagnostic stewardship team, therefore, is necessary to evaluate the technologies available, better integrate the selected technologies into the healthcare system and develop innovative and appropriate uses. It also needs diagnostic stewardship policies aimed at choosing the right diagnostic test for a specific patient at the optimal time for maximum clinical efficacy and cost-effectiveness.
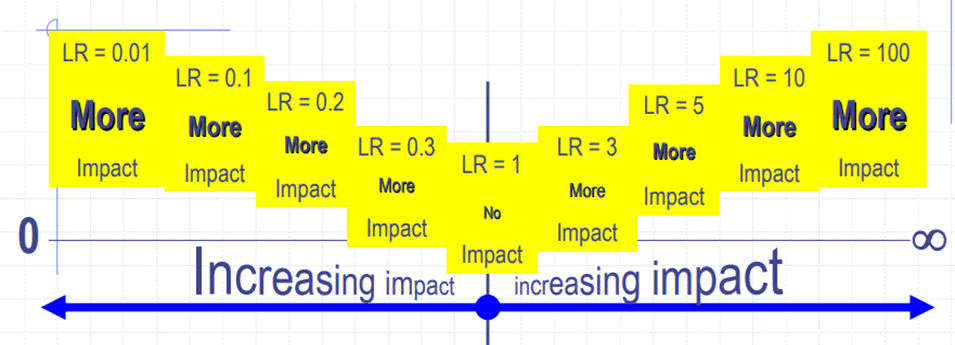
The maximizing process for enhancing diagnostic tests and diagnosis involves education, order sets, order search menus, reflex orders, hard and soft orders, electronic reference, feedback and benchmarking, decision algorithms and predictive analytics. To better use diagnostic stewardship in accordance with evidence-based medicine, the team must consider sensitivity, specificity, likelihood ratio and infection prevalence. The selection of a test or method must be based on the strength of the available scientific evidence.
Diagnostic reasoning for the management of neonatal sepsis
Diagnostic approaches for neonatal sepsis include various techniques such as conventional microbiologic techniques, biomarkers, gene expression profiling and molecular analysis. These approaches can provide valuable information for the diagnosis of neonatal sepsis. However, it is important to note that the availability and utilization of these diagnostic approaches may vary depending on factors such as socioeconomic status, technological advancement, human skill and institutional culture. In some healthcare settings, these advanced diagnostic techniques may not be readily accessible or routinely used. In such cases, certain commonly used biomarkers can still support the clinical judgment or gestalt in diagnosing neonatal sepsis. White Blood Cell count (WBC), CReactive Protein (CRP) and Procalcitonin (PCT) levels are among the biomarkers that are frequently utilized in the diagnosis of neonatal sepsis. An elevated WBC count, increased CRP levels and elevated PCT levels can indicate the presence of infection or inflammation in the newborn. These biomarkers, along with clinical assessment, can aid healthcare providers in making decisions regarding the diagnosis and management of neonatal sepsis, especially in settings where more advanced diagnostic techniques may not be available.
To narrow the variation, Raymond Bartlett's 1974 called for the development of more practical, economical and clinically meaningful diagnostic approaches using clinical information to arrive at a diagnosis. The clinically meaningful diagnostic method, also known as diagnostic reasoning, is the act of reasoning logically about neonatal sepsis, for example, in order to reach a conclusion. It is the most crucial of a doctor's talents, an assessment of a clinician's ability and the key component of a professional self-image. Diagnostic reasoning involves differential diagnosis and is essential to establish a diagnosis and improve the prognosis of newborn sepsis. The concept heightened the need for accurate and sensitive diagnostics to confirm the diagnosis of neonatal sepsis.
The diagnostic reasoning enables a cautious selection of diagnostic tests, using criteria such as ASSURED (Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipmentfree and Deliverable to end-users). In a more advanced laboratory setting, scholars sought for more effective predictive values and outlined a series of diagnostic selection steps before recommendation for neonatal sepsis. Further, they evaluate the effectiveness of the selected diagnostic tests at four levels: Analytical, diagnostic, operational and medical decisionmaking. Despite their high predictive value, none of the diagnostic tests is perfect and until now, a single score has not been proven to be comprehensive. Therefore, the best clinical evidence continues to be supported by several diagnostic tests, diagnostic stewardship and diagnostic reasoning.
The fundamental principles of diagnostic reasoning require a clinician to consider the diagnostic test setting (institutional culture and climate), test accuracy (sensitivity, specificity, predictive values and likelihood ratios), as well as Bayes' Theorem and Fagan nomograms. The clinician must also define the odds of infection, the pre-test probability or disease prevalence, the pre-test odds and the post-test probability to estimate the likelihood ratio or use a Fagan nomogram. Practically, high likelihood ratio positive values aid in ruling in sepsis and low likelihood ratio negative values aid in ruling out sepsis, while values close to 1 indicate poor accuracy (Figure 6).
Figure 6. Application and interpretation of the likelihood ratio.
Based on the above information, the test likelihood of the neonatal sepsis varies by setting and context. For example, to put the discussion into context at Jimma medical center, first, the prevalence of neonatal sepsis in Jimma medical center's neonatal intensive care unit is 64.1%. According to the systematic review and meta-analysis study, if the neonate has given a C-reactive protein test, the sensitivity (0.69) and specificity (0.77) were comparable to those at Jimma medical center in a developing country. If the test is performed without a thorough history and physical examination, the neonate will have a pretest probability consistent with the center's prevalence of neonatal sepsis (64.1%). The pretest odd is converted to odd and measures (0.69/1-0.69=2.3), implying that the neonate has 2.3 odds of developing sepsis prior to the test. The neonate's test-positive likelihood ratio will be 3.83 (0.656/1-0.78) and its negative likelihood ratio will be 0.44 (1-. 656/.78). Finally, converting the pretest odds to posttest odds (2.3*3.83=8.83) and the odds to probability (8.83/1+8.83=89.8%) yields an 89.8% chance that the neonate has sepsis. Based on the data, if you think the neonate may have sepsis, it might be reasonable to check for a C-reactive protein level. Yet it's important to keep an eye on the process of the test to increase your test likelihood ratio.
Current statuses and practical implications of diagnostic stewardship
The concept of diagnostic stewardship is becoming increasingly popular in hospitals, but there are no published papers for countries other than Nigeria. The application of diagnostic stewardship is premeditated to reduce testing in patients with low pretest probability, ensure correct specimen collection technique and warn clinical teams of potential spurious results. The concept was then recognized as having the potential to significantly improve the quality and value of health care.
Woods-Hill and his US colleagues' study report concluded that multidisciplinary diagnostic stewardship can optimize diagnostic test practice and broad-spectrum antibiotic use in pediatric critical care centers. Another study has found that a program can significantly lower rates of antibiotic utilization, reduce unnecessary antibiotic use, provide faster time-topositive tests, shorten empiric therapy and reduce intravenous antimicrobial duration. These studies simultaneously discovered no differences in the time to effective antimicrobials, hospital admissions, antimicrobial starts or length of stay, total hospital cost or microbiologic testing costs. However, the summa of the diagnostic stewardship couldn’t be indicated because of the limited number of published papers.
Challenges of diagnostic stewardship and diagnostic reasoning
Diagnostic stewardship in neonatal care requires collaboration among clinical laboratories, pharmacists and infectious disease clinicians to ensure that appropriate tests are ordered and the information is effectively translated into appropriate management in real time. However, there are challenges and barriers that need to be addressed for successful implementation. These include the lack of standardized order menus, inadequate integration with electronic health records, insufficient education on test performance parameters and overall cost and resistance to change. Another challenge in diagnosing neonatal sepsis is the absence of a clear gold standard or cutoff point for interpreting certain diagnostic test results. This can lead to overlapping values, making it difficult to differentiate between neonates with and without sepsis.
Conclusion
Diagnostic stewardship and diagnostic reasoning are emerging concepts that have the potential to improve neonatal care, particularly in managing sepsis. These concepts emphasize the judicious use of diagnostic tests to ensure accurate and timely diagnoses while minimizing unnecessary testing. They have been applied in broader healthcare settings and have shown promise in improving patient outcomes and reducing costs. Diagnostic reasoning is the cognitive process used by healthcare providers to arrive at a diagnosis based on clinical information, patient history, physical examination findings and available diagnostic tests. It involves critical thinking, pattern recognition and the synthesis of information to make accurate diagnostic decisions. Effective diagnostic reasoning is crucial for the timely and appropriate management of conditions like neonatal sepsis. To further support the implementation of these concepts in neonatal care, robust research and academic studies are necessary. Conducting rigorous analysis, clinical trials and observational studies specific to neonatal populations would provide valuable evidence to guide the implementation and evaluate the impact of these concepts on neonatal outcomes, cost-effectiveness and overall quality of care. The scarcity of published papers may present a challenge, but further research is needed to establish diagnostic stewardship and reasoning as important components of neonatal care.
Author Contributions
The review was conceptualized by DG and designed by DG, GA, BA, NW and GB, who worked with together for literature search and manuscript creation. The results were interpreted by DG, GA, NW, BA and GB, who also wrote, edited and reviewed the manuscript for intellectual content. The final version was approved by all authors and assigned DG to manage the publication process.
Ethical Statement
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgment
Declared none.
Funding Information
The review has not granted fund.
References
- Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: The 60-30-10 challenge. BMC Med 2020; 18:102.
[Crossref] [Google Scholar] [PubMed]
- Rosa-Mangeret F, Benski AC, Golaz A, et al. 2.5 million annual deaths-Are neonates in low-and middle-income countries too small to be seen? A bottom-up overview on neonatal morbi-mortality. Trop Med Infect Dis 2022; 7(5):64.
[Crossref] [Google Scholar] [PubMed]
- Helguera-Repetto AC, Soto-Ramírez MD, Villavicencio-Carrisoza O, et al. Neonatal sepsis diagnosis decision-making based on artificial neural networks. Front Pediatr 2020; 8:525.
[Crossref] [Google Scholar] [PubMed]
- Qazi SA, Stoll BJ. Neonatal sepsis: A major global public health challenge. Pediatr Infect Dis J 2009; 28(1 Suppl):S1-2.
[Crossref] [Google Scholar] [PubMed]
- Peters RP, van Agtmael MA, Danner SA, et al. New developments in the diagnosis of bloodstream infections. Lancet Infect Dis 2004; 4(12):751-760.
[Crossref] [Google Scholar] [PubMed]
- Madden GR, Weinstein RA, Sifri CD. Diagnostic stewardship for healthcare-associated infections: Opportunities and challenges to safely reduce test use. Infect Control Hosp Epidemiol 2018; 39(2):214-218.
[Crossref] [Google Scholar] [PubMed]
- Zacharioudakis IM, Zervou FN. Diagnostic stewardship in infectious diseases: Steps towards intentional diagnostic testing. Future Microbiol 2022; 17(11):813-817.
[Crossref] [Google Scholar] [PubMed]
- Morado F, Wong DW. Applying diagnostic stewardship to proactively optimize the management of urinary tract infections. Antibiotics 2022; 11(3):308.
[Crossref] [Google Scholar] [PubMed]
- Sullivan KV. Diagnostic stewardship in clinical microbiology, essential partner to antimicrobial stewardship. Clin Chem 2022; 68(1):75-82.
[Crossref] [Google Scholar] [PubMed]
- Morjaria S, Chapin KC. Who to test, when and for what: Why diagnostic stewardship in infectious diseases matters. J Mol Diagn 2020; 22(9):1109-1113.
[Crossref] [Google Scholar] [PubMed]