Research Paper - Ophthalmology Case Reports (2021) Volume 5, Issue 6
Correlation between water drinking test and modified phasing among medically treated primary open angle glaucoma patients in Enugu, Nigeria
Gloria C. Eze1*, Nkiru Kizor-Akaraiwe1, Ifeoma R. Ezegwui2
1Ophthalmology Department, Enugu State University of Science and Technology Teaching Hospital Parklane, Enugu, Nigeria.
2Ophthalmology Department, University of Nigeria Teaching Hospital Ituku-Ozalla, Enugu, Nigeria.
- Corresponding Author:
- Gloria C. Eze
Ophthalmology Department
Enugu State University of Science and Technology
Teaching Hospital Parklane, Enugu; P.O.Box 2051 Enugu, Nigeria
Tel: +234-8034335432
Email: chizglo1@gmail.com
Accepted date: September 20 2021
Citation: Eze GC, Akaraiwe NK, Ezegwui IR. Correlation between water drinking test and modified phasing among medically treated primary open angle glaucoma patients in Enugu, Nigeria. Ophthalmol Case Rep. 2021;5(6):1-5.
Abstract
Aim: To determine the correlation between the mean intraocular pressure peaks and fluctuations in water drinking test and modified phasing among primary open angle glaucoma patients on medical treatment at the eye clinic of Enugu State University of Science and Technology Teaching Hospital Parklane (ESUTTHP), Enugu. Study design: This was a cross sectional study done at the eye clinic of Enugu State University of Science and Technology Teaching Hospital Parklane, Enugu, Nigeria between August and October 2017. Methodology: One hundred and thirty primary open angle glaucoma patients (56 males, 74 females; age range 42-83 years) on medical treatment were selected by simple random sampling. Modified phasing was performed on them over 8 hours (from 8:00am to 4:00pm) with intraocular pressure measured at 2 hourly intervals. Water drinking test was done on another day over 2 hours (between 8:00am and 11:00am) after intake of 1 liter of water with intraocular pressure measured every 15 minutes. Data analysis was done using statistical package for social sciences version 20 for windows (USA). Pearson’s correlation was used to find the correlation between mean intraocular pressure peaks and fluctuations in water drinking test and modified phasing. Results: The mean intraocular pressure peaks during water drinking test and modified phasing were 22.9 ± 5.7 and 18.0 ± 4.4 mmHg, respectively. The mean intraocular pressure fluctuations during water drinking test and modified phasing were 7.9 ± 3.9 and 5.6 ± 2.4 mmHg, respectively. There was significant correlation between the mean peak intraocular pressure during water drinking test and modified phasing (r=0.589, p ≤ 0.05) as well as between the intraocular pressure fluctuation during water drinking test and modified phasing (r=0.186, p ≤ 0.05). Conclusion: Water drinking test could be done as a quick clinic procedure for black primary open angle glaucoma patients on medical treatment to detect their intraocular pressure peaks and fluctuations so as to manage appropriately. Keywords: Primary open angle glaucoma, Intraocular pressure, Water drinking test, Modified phasing. Abbreviations: POAG: Primary Open Angle Glaucoma, WDT: Water Drinking Test, IOP: Intraocular Pressure, ESUTTHP: Enugu State University of Science and Technology Teaching Hospital Parklane
Keywords
Primary open angle glaucoma, Intraocular pressure, Water drinking test, Modified phasing.
Abbreviations
POAG: Primary Open Angle Glaucoma, WDT: Water Drinking Test, IOP: Intraocular Pressure, ESUTTHP: Enugu State University of Science and Technology Teaching Hospital Parklane
Introduction
Primary open angle glaucoma (POAG) is more prevalent [1] as well as more aggressive in blacks [2] especially in West Africa and South-East Nigeria consequently leading to blindness [3-5]. Intraocular Pressure (IOP) is the main modifiable risk factor in glaucoma that is addressed in its management [6]. High IOP peaks and fluctuations have been identified as the risk factors for glaucoma progression [7,8]. Intraocular pressure peak and fluctuation can be detected through phasing. However, phasing is time consuming and may require hospital admission. Consent for phasing therefore is a challenge as it significantly disrupts patient’s busy schedule apart from the demand on the clinician’s time. As a result, clinicians take only one IOP measurement during follow-up visits. This single IOP value may not reflect the patient’s IOP peak or fluctuation. The modified phasing which is carried out during clinic hours of 8:00 am-4:00 pm has been found to correlate with the 24-hour full phasing [9]. However, many clinicians and patients still find the 8-hour modified phasing challenging.
Water Dinking Test (WDT) is a stress test that can be used to evaluate the outflow facility [10]. It is fast, requires no hospitalization and done as an office procedure over one or two hours. WDT has been neglected over the years because of its poor diagnostic value for glaucoma [11,12]. However recently, it was found to be useful in monitoring glaucoma treatment and predicting diurnal IOP peaks as well as fluctuations among Caucasians and Asians [11-15]. There is paucity of studies on correlation between water drinking test and modified phasing among glaucoma patients in the Nigerian population. Therefore, this study aims to determine the correlation between water drinking test and modified phasing among primary open angle glaucoma patients on medical treatment at the eye clinic of ESUTTHP Enugu. This may give evidence for a quick clinic test for assessing IOP peak and fluctuation for better management of glaucoma patients in Nigeria.
Material and Methods
The study was a hospital based cross sectional study on POAG patients on medical treatment attending the eye clinic of a tertiary hospital between August and October 2017. The study adhered to the tenets of the Helsinki declaration. Ethical approval was obtained from the Enugu State University of Science and Technology Teaching hospital Health Research and Ethics Committee before commencement of the study. A written informed consent was obtained from each patient before being included in the study.
One hundred and thirty already diagnosed POAG patients on medical treatment were selected by simple random sampling using a table of random numbers. Both eyes of each patient (total of 260 eyes) were examined which included visual acuity assessment, gonioscopy, anterior and posterior segments examination. Consenting POAG patients 40 years and above on medical treatment were included in the study while those with angle closure or secondary glaucoma, history of previous glaucoma surgeries or laser treatment, ocular conditions requiring steroid therapy, underlying medical conditions like severe hypertension (blood pressure ≥ 180/110 mmHg), renal or heart failure were excluded. A structured intervieweradministered proforma questionnaire was used to obtain information on their biodata, clinical history as well as record the examination findings.
Modified phasing and WDT were carried out on both eyes of the study participants on two different days with intraocular pressure measured using Perkins applanation tonometer. Modified phasing was done over 8 hours (from 8:00am to 4:00pm) with intraocular pressure measured at 2 hourly intervals. WDT was done over 2 hours (between 8:00 am and 11:00 am) after intake of 1 liter of water (at room temperature) within 5 minutes with intraocular pressure measured every 15 minutes. A baseline IOP was measured before intake of the 1 liter of water. Out of the 130 POAG patients studied, 129 (258 eyes) did WDT while 124 (248 eyes) did modified phasing.
Data analysis was done using Statistical Package for Social Sciences (SPSS) version 20 for windows (SPSS Inc., Chicago, III, USA). The mean IOP peak and fluctuation during WDT and modified phasing were determined. Peak IOP was defined as the maximum IOP measured during the WDT or modified phasing. IOP fluctuation was defined as the difference between peak IOP and baseline IOP in WDT or the difference between peak IOP and the lowest IOP during modified phasing. Pearson’s correlation was used to find the correlation between mean IOP peaks and fluctuations in WDT and modified phasing. A p value of ≤ 0.05 was used to define statistical significance corresponding to a 95% confidence interval.
Results
A total of 260 eyes of 130 POAG patients on medical treatment were examined comprising 56 males (43.1%) and 74 females (56.9%). Their age ranged between 42 and 83 years with mean age of 62.25 ± 9.002 years.
The mean peak IOP and mean IOP fluctuation during WDT were 22.9 ± 5.7 mmHg and 7.9 ± 3.9 mmHg respectively. The mean peak IOP and mean IOP fluctuation during Phasing were 18.0 ± 4.4 mmHg and 5.6 ± 2.4 mmHg respectively (Table 1).
| Minimum | Maximum | Mean | Standard Deviation | |
|---|---|---|---|---|
| Water drinking test Peak IOP | 10.2 | 38.1 | 22.9 | 5.7 |
| Water drinking test IOP fluctuation | 1.0 | 20.5 | 7.9 | 3.9 |
| Modified Phasing Peak IOP | 7.7 | 31.0 | 18.0 | 4.4 |
| Modified Phasing IOP fluctuation | 1.0 | 14.5 | 5.6 | 2.4 |
Table 1: Mean IOP peak and fluctuation during Water Drinking Test, mean IOP peak and fluctuation during modified phasing.
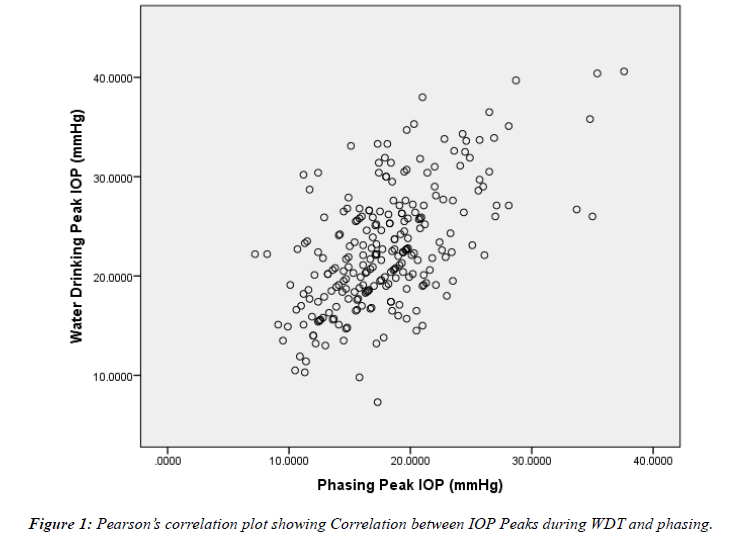
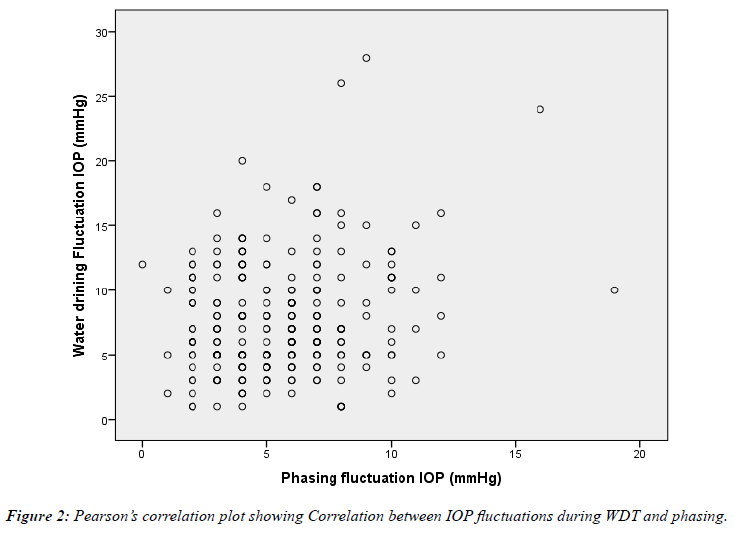
On comparing the IOP peak during WDT with IOP peak during phasing, there was significant correlation between them (r=0.589, p ≤ 0.05). There was also significant correlation between IOP fluctuation during WDT and IOP fluctuation during phasing (r=0.186, p ≤ 0.05; Table 2, Figures 1 and 2).
| Phasing | Peak IOP | Phasing IOP | fluctuation | ||
|---|---|---|---|---|---|
| Water drinking test |
Pearson Correlation | 0.589* | |||
| peak IOP | coefficient (r) | ||||
| P-value | 0.001 | ||||
| Water drinking test | Pearson Correlation | ||||
| IOP fluctuation | coefficient | 0.186* | |||
| P-value | 0.003 | ||||
| *Correlation is significant at p ≤ 0.05 | |||||
Table 2: Correlation between mean IOP peak and fluctuation during WDT and phasing.
High peak IOP values and IOP fluctuation have been found to play significant role in glaucoma progression despite acceptable IOP values during clinic visits [6,7] The mean peak IOP of 22.9 ± 5.7mmHg in WDT among the patients studied was similar to the study in USA by Moraes, et al. [16] in which the mean peak IOP was 20.0 ± 2.9 mmHg. However, Susanna, et al. [10] in Brazil found a lower mean peak IOP of 16.5 ± 3.8 mmHg while Yassein, et al [17] in Egypt found a higher mean peak IOP of 26.57 mmHg. These variations could be due to differences in the duration of WDT. In the present study WDT was done over 2 hours with few patients having peak IOP after one hour whereas Susanna, et al. [10] did WDT over one hour and may have missed out some IOP peaks that may have occurred after one hour thereby resulting in lower mean peak IOP.
The mean peak IOP of 18.0 ± 4.4 mmHg during modified phasing was higher than that reported by Moodie, et al [9] who observed a slightly lower mean peak IOP (16.96 ± 3.51 mmHg) during daytime phasing. In contrast, Caiado, et al. [13] in Brazil found a slightly higher mean peak IOP (20.0 ± 3.3 mmHg) in daytime phasing among POAG patients on medical treatment while the mean peak IOP (25.71 ± 7.20 mmHg) in the medical group found by Yassein, et al. [17] in Egypt was even much higher than that found in the present study. The disparity could be due to the differences in the duration of phasing as well as interval of IOP measurements in the different studies.
The mean peak IOP during WDT was higher than the mean peak IOP during phasing. However, there was a significant correlation between the peak IOP during WDT and the peak IOP during phasing (r=0.589, p ≤ 0.05). This is similar to the findings of previous studies in USA by Moraes, et al. [14], Australia by Kumar, et al. [18], China by Lizuozuo [19], USA by Moraes, et al. [16] which suggests that WDT may be done in place of phasing to detect IOP peaks of glaucoma patients on medical treatment.
The mean IOP fluctuation in WDT was 7.9 ± 3.9 mmHg. Smaller proportion of the patients had IOP fluctuation ≤ 6 mmHg while greater proportion had IOP fluctuation > 6mmHg. This shows that greater proportion of these POAG patients might be at risk of glaucomatous progression. Guedes, et al. [20] in USA also found a high mean IOP fluctuation of 8.4 mmHg which is comparable to that in the present study. In contrast, some previous studies by Susanna, et al. in Brazil [21], Medeiros, et al. in Brazil [22] and Ozyol, et al in Turkey [23] found lower mean IOP fluctuations which were within the normal range (≤ 6 mmHg).
The mean IOP fluctuation of 5.6 ± 2.4mmHg during modified phasing in this study was within the normal range (2 mmHg-6 mmHg) unlike during WDT where greater proportion of patients had IOP fluctuation ≤ 6mmHg. Jonas, et al. [24] in USA found a mean IOP fluctuation of 5.74 ± 3.44 mmHg though he did a 24-hour phasing. However, Yassein, et al. [17], Moodie, et al. [9] and Caiado, et al. [13] found lower mean IOP fluctuations of 4.85 mmHg, 4.99 ± 2.54 and 3.3 ± 1.0 mmHg respectively during daytime phasing. These differences might be a reflection of the level of IOP control achieved in the different study groups.
Though the mean IOP fluctuation during WDT was higher than the mean IOP fluctuation during phasing, there was significant correlation between the IOP fluctuations during WDT and phasing (r=0.186, p ≤ 0.05). This is similar to the study by Moraes, et al. [16] in USA (r=0.780, p<0.0001). In contrast, Kumar, et al. [18] found that there was no significant correlation between IOP fluctuation during WDT and that during daytime phasing. This difference could be due to the small sample size which included glaucoma patients, ocular hypertensives and glaucoma suspects.
Conclusion
There was a significant correlation between the IOP peaks and fluctuations obtained during WDT and modified phasing in this study. Therefore, WDT may be done as a quick clinic procedure for POAG patients on medical treatment so as to detect their IOP peaks and fluctuations and manage appropriately.
Acknowledgement
We sincerely appreciate all the study participants who voluntarily agreed to participate in this study and the Head, Ophthalmology department, ESUT Teaching hospital Parklane, Enugu for allowing us to conduct this research work in her department.
Disclosures
No monetary grants or sponsoring organizations.
References
- Leske MC, Connell AM, Schachat AP, et al. The Barbados Eye Study. Prevalence of open angle glaucoma. Arch Ophthalmol. 1994;112:821-9.
- Racette L, Wilson MR, Zangwill LM, et al. Primary open-angle glaucoma in blacks: a review. Surv Ophthalmol. 2003;48:295-313.
- Rabiu M, Abdull MM, Kyari F, et al. The Nigeria national blindness and visual impairment survey 2005-2007. Investig Ophthalmol Vis Sci. 2009;50:4114-20.
- Azuamah Y, Amadi A, Esenwah E, et al. Major Causes of Low Vision and Blindness in Southeast Nigeria. Int J Heal Sci Res. 2013;3:48-52.
- Egbert PR. Glaucoma in West Africa: a neglected problem. Br J Ophthalmol. 2002;86:131-2.
- Varma R, Hwang L-J, Grunden JW, et al. Inter-visit intraocular pressure range: an alternative parameter for assessing intraocular pressure control in clinical trials. Am J Ophthalmol. 2008;145:336-42.
- Leske CM, Heijl A, Hussein M, et al. Factors for Glaucoma Progression and the Effect of Treatment-The Early Manifest Glaucoma Trial. Arch Ophthalmol. 2003;121:48-56.
- De Moraes CG V, Juthani VJ, et al. Risk Factors for Visual Field Progression in Treated Glaucoma. Arch Ophthalmol. 2011;129:563-7.
- Moodie J, Wilde C, Rotchford AP, et al. 24-Hour versus daytime intraocular pressure phasing in the management of patients with treated glaucoma. Br J Ophthalmol. 2010;94:999-1002.
- Susanna Jr R, Hatanaka M, Vessani RM, et al. Correlation of Asymmetric Glaucomatous Visual Field Damage and Water-Drinking Test Response. Investig Ophthalmol Vis Sci. 2006;47:641-4.
- Clement C, Bhartiya S. IOP assessment with the water drinking test [Internet]. Glaucoma Now. 2013 [cited 2015 Dec 5]. p. 10-1.
- Roth JA. Inadequate diagnostic value of the water-drinking test. Br J Ophthalmol. 1974;58:55-61.
- Caiado RR, Badaró E, Kasahara N. Intraocular pressure fluctuation in healthy and glaucomatous eyes: a comparative analysis between diurnal curves in supine and sitting positions and the water drinking test. Arq Bras Oftalmol. 2014;77:288-92.
- Vasconcelos-Moraes CG, Susanna Jr R. Correlation between the water drinking test and modified diurnal tension curve in untreated glaucomatous eyes. Clinics. 2008;63:433-6.
- Sakata R, Aihara M, Murata H, et al. Intraocular pressure change over a habitual 24-hour period after changing posture or drinking water and related factors in normal tension glaucoma. Investig Ophthalmol Vis Sci. 2013;54:5313.
- De Moraes CG V, Furlanetto LR, Reis ASC, et al. Agreement between stress intraocular pressure and long-term intraocular pressure measurements in primary open angle glaucoma. Clin Exp Ophthalmol. 2009;37:270-4.
- Yassein HA, Hamdi MM, Abdelshafik MA, et al. The Value of Water Drinking Test as a Clue for Short Term Intraocular Pressure Fluctuation. Clin Exp Ophthalmol. 2016;7:536.
- Kumar RS, De Guzman MHP. Does peak intraocular pressure measured by water drinking test reflect peak circadian levels? A pilot study. Clin Exp Ophthalmol. 2008;36:312-5.
- LiZuoZuo. Clinical study of water drinking test and twenty-four-hour monitoring of intraocular pressure in patients with Primary Open Angle Glaucoma. Zhengzhou University; 2012.
- Guedes RA, Guedes VM, et al. Use of water drinking test after non-penetrating deep sclerectomy. French J Ophthalmol. J Fr Ophthalmol; 2005;28:1076-80.
- Susanna Jr R, Vessani RM, Sakata L, et al. The relation between intraocular pressure peak in the water drinking test and visual field progression in glaucoma. Br J Ophthalmol. 2005;89:1298-301.
- Medeiros FA, Pinheiro A, Moura FC, et al. Intraocular Pressure Fluctuations in Medical versus Surgically Treated Glaucomatous Patients. J Ocul Pharmacol Ther. 2002;18:489-98.
- Özyol P, Özyol E, Baldemir E. Intraocular pressure dynamics with prostaglandin analogs: a clinical application of water-drinking test. Clin Ophthalmol. 2016;10:1351-6.