Research Article - Biomedical Research (2017) Volume 28, Issue 8
Comparison of transcolostomy single-incision laparoscopic and open procedures in secondary operations for hirschsprung's disease
Junmei Yan1,2, Sanliang Li3, Yan Chang2, Jian Wang1 and Aiwu Li1*
1Department of Pediatric Surgery, Qilu Hospital of Shandong University, Jinan, PR China
2Department of Pediatric Surgery, Yidu Center Hospital of Weifang, Weifang, PR China
3Department of Anesthesia, Yidu Center Hospital of Weifang, Weifang, PR China
- *Corresponding Author:
- Aiwu Li
Department of Pediatric Surgery
Qilu Hospital of Shandong University, PR China
Accepted on December 29, 2016
Abstract
The aim of this study was to report our experience with the Soave pull-through procedure combined with a single-incision laparoscopic approach to treat Hirschsprung's disease after one-stage colostomy, in comparison with an open approach. A total of 37 children diagnosed with Hirschsprung's Disease after one-stage colostomy were evaluated in this study from June 2008 to May 2014. Nineteen patients treated with the Soave pull-through combined with an open approach from June 2008 to May 2011 were in Group 1, and 18 patients treated with a single-incision (abdominal wall colostomal) laparoscopic Soave pull-through approach from June 2011 to June 2014 were in Group 2. The preoperative data, operative details, and follow-up outcomes were compared in the two groups to determine the advantages of the single-incision laparoscopic approach. Statistical comparison was made with unpaired t-tests, χ2 tests and Fisher’s exact test, with P value less than 0.05 considered significant. The two groups had similar preoperative patient data to ensure comparability. The operative time in Group 2 was similar to that in Group 1, and all Group 2 cases underwent a single-incision laparoscopic approach. The postoperative time to feeding and the hospital stay after surgery were shorter in Group 2, which showed less blood loss, fewer complications, and less incidental injury. All patients were followed up for 6-12 months, and outcomes were better in Group 2. Compared to open surgery, the laparoscopic singleincision abdominal wall colostomal approach had many benefits and was effective in treatment of Hirschsprung's disease after one-stage colostomy.
Keywords
Laparoscopic, Single-incision, Colostomy, Pull-through, Comparison.
Introduction
Hirschsprung's disease (HSCR) is characterized by the absence of autonomic ganglion cells in the terminal bowel, and is a relatively common cause of intestinal obstruction in newborns [1]. The incidence of HSCR is estimated to be 1 in 5,000 live births [2]. Enterocolitis is the most common cause of significant morbidity and death in HSCR [3-5]. When a neonate with HSCR has a colon perforation or enterocolitis, initial life-saving intestinal fistula surgery must be performed [6]. A second stage radical operation must contend with abdominal cavity adhesions, and a pull-through laparotomy is commonly performed [7,8].
The surgical technique for HSCR has been modified several times in the last twenty years. From a total transanal, endorectal pull-through (TERPT) to a laparoscopy-assisted approach, the need to reduce surgical trauma has been a concern [9-11]. Single-incision laparoscopic surgery (SILS) has gained acceptance as a method to reduce visible abdominal scars [2,12-14]. In this article, we introduce abdominal wall colostomal SILS and provide a comprehensive and detailed comparison with the open procedure to evaluate the advantages of this minimally invasive laparoscopic surgery.
Materials and Methods
Patient data
From June 2008 to May 2011, 19 children with HSCR, with a mean age of 5.8 months (range 3.1 to 7.3 months), were treated following colostomy with an open-assisted Soave pull-through approach; 14 were boys (73.7%) and 5 were girls (26.3%). All cases were diagnosed by pathological examination after the one-stage colostomy at a mean age of 20.8 days (range 9 to 27 days); 11 long-type cases (lesion involving descending or transverse colon) were treated with transverse colostomy (57.9%), and 8 common-type cases (lesion involving sigmoid colon) were treated with sigmoidostomy (42.1%), based on Chinese guidelines. These patients were in Group 1. This study was conducted in accordance with the declaration of Helsinki.
This study was conducted with approval from the Ethics Committee of Shandong University. Written informed consent was obtained from all participants’ guardians.
From June 2011 to May 2014, 18 children with HSCR, with a mean age of 6.2 months (range 3.6 to 8.1 months), were treated following colostomy with a SILS-assisted Soave pull-through approach; 13 were boys (72.2%) and 5 were girls (27.8%). The mean age at one-stage colostomy was 21.9 days (range 8 to 29 days); 11 long-type cases were treated with transverse colostomy (61.1%), and 7 common-type cases were treated with sigmoidostomy (38.9%). These patients were in Group 2. The detailed data of all patients including nutritional status and body mass index (BMI) are shown in Table 1; there were no statistical differences between the two groups.
| Index | Open Group | Laparoscopy Group | P value |
|---|---|---|---|
| Cases | 19 | 18 | - |
| Age (month) | 5.8 ± 2.15 | 6.2 ± 2.07 | 0.7158 |
| Sex (male/female) | 14/5 | 13/5 | - |
| Disease Type (long type/common type) | 11/8 | 11/7 | - |
| Colostomy site (transverse colon/sigmoid ) | 11/8 | 11/7 | - |
| Colostomy age (days) | 20.8 ± 5.5 | 21.9 ± 3.2 | 0.7673 |
| Nutritional status | |||
| Serum total protein(g/L) | 68.1 ± 6.21 | 71.2 ± 4.09 | 0.9583 |
| Serum albumin(g/L) | 46.2 ± 6.63 | 49.5 ± 5.59 | 0.9442 |
| Hemoglobin(g/L) | 125.1 ± 11.17 | 128.9 ± 9.19 | 0.8662 |
| Blood urea nitrogen (BUN)(mmol/L) | 3.44 ± 1.12 | 3.11 ± 1.07 | 0.1831 |
| Length (cm) | 64.8 ± 3.94 | 66.5 ± 4.18 | 0.8944 |
| Weight (KG) | 7.6 ± 2.01 | 8.1 ± 2.45 | 0.7496 |
| Basal metabolic index (BMI) | 8.5% ± 0.04 | 8.9% ± 0.05 | 0.6054 |
Table 1. The comparison of preoperative data between Laparoscopy and Open group (mean ± SD).
Surgical techniques
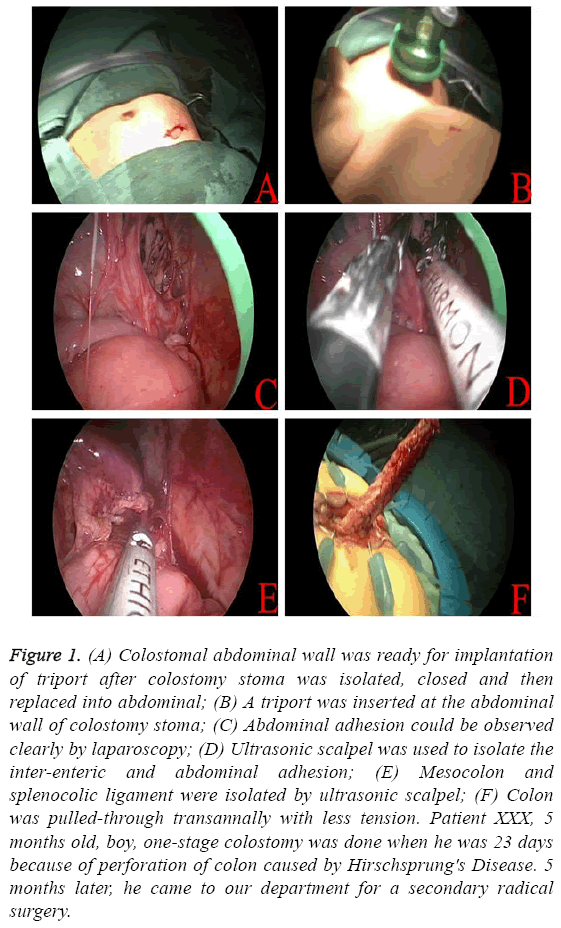
Adequate bowel preparation was necessary and operative position was as for abdominal-perineal resection. The abdominal operation was performed first, and the colostoma was isolated, closed, and then replaced in the abdomen, using a 2 cm, fusiform incision around the colostoma. Then, a modification of a transanal Soave pull-through procedure for HSCR was performed as previously described [10], unless there was a problem with the transanal pull-through because of difficult mesocolon ligation. Then, laparoscopy was used to assist the procedure on the isolated colon instead of traditional open surgery. A TriPort was inserted at the abdominal wall colostoma (Figures 1A and 1B), through which 5-mm laparoscopic instruments were inserted into the abdominal cavity, and carbon dioxide was insufflated at a pressure of 8-10 mmHg. An ultrasonic scalpel was used to isolate the interenteric and abdominal adhesions (Figures 1C and 1D), mesocolon, and splenocolic ligament (Figure 1E), to enable tensionless, transanal colon pull-through (Figure 1F). The modified Soave pull-through procedure could then be completed.
Figure 1: (A) Colostomal abdominal wall was ready for implantation of triport after colostomy stoma was isolated, closed and then replaced into abdominal; (B) A triport was inserted at the abdominal wall of colostomy stoma; (C) Abdominal adhesion could be observed clearly by laparoscopy; (D) Ultrasonic scalpel was used to isolate the inter-enteric and abdominal adhesion; (E) Mesocolon and splenocolic ligament were isolated by ultrasonic scalpel; (F) Colon was pulled-through transannally with less tension. Patient XXX, 5 months old, boy, one-stage colostomy was done when he was 23 days because of perforation of colon caused by Hirschsprung's Disease. 5 months later, he came to our department for a secondary radical surgery.
Statistical analysis
Statistical comparisons were made using unpaired t-tests, χ2 tests, and Fisher’s exact test, with P value less than 0.05 considered significant.
Results
All cases were successfully completed, and there were no deaths. No case was converted to open surgery in Group 2. The comparison of operative and hospital data for Group 1 and Group 2 is shown in Table 2. The operative times (170.2 ± 17.8 vs. 175.5 ± 20.7, P=0.7957) and postoperative defecation frequency (7.8 ± 2.2 vs. 8.1 ± 1.9, P=0.6697) were similar between the two groups, but Group 2 had less blood loss (12.5 ± 6.2 vs. 47.3 ± 7.1, P<0.001), less incidental injury (0 vs. 2/19, 10.5%), fewer hospitalization days (6.2 ± 1.5 vs. 13.1 ± 1.8, P<0.001), and earlier postoperative return to feeding (3.1 ± 1.8 vs. 6.2 ± 2.1, P<0.001). Among postoperative complications, no anastomotic leakage or intra-abdominal infection occurred in the two groups; however, the rate of abdominal wound infections and postoperative intestinal obstruction and enterocolitis were lower in Group 2 than in Group 1 (0 vs. 2/19, 10.5%; 0 vs. 2/19, 10.5%; 0 vs. 1/19, 5.26%).
| Index | Open Group | Laparoscopy Group | P value |
|---|---|---|---|
| Cases | 19 | 18 | - |
| Procedure time(min) | 170.2 ± 17.8 | 175.5 ± 20.7 | 0.7957 |
| Blood loss(ml) | 47.3 ± 7.1 | 12.5 ± 6.2 | <0.0001 |
| Side-injury | 2/19, 10.5% | 0 | |
| Postoperative food taken(d) | 6.2 ± 2.1 | 3.1 ± 1.8 | <0.0001 |
| Hospitalization days(d) | 13.1 ± 1.8 | 6.2 ± 1.5 | <0.0001 |
| Defection frequency | 7.8 ± 2.2 | 8.1 ± 1.9 | 0.6697 |
| Postoperative complications | |||
| Abdominal wound infection | 2/19, 10.5% | 0 | - |
| Anastomotic leakage | 0 | 0 | - |
| Postoperative intestinal obstruction | 2/19, 10.5% | 0 | - |
| Abdominal infection | 0 | 0 | - |
| Posteoperative enterocolitis | 1/19, 5.26% | 0 | - |
Table 2. The comparison of operative and hospitalized data between Laparoscopy and Open group (mean ± SD).
The results of follow-up in the outpatient clinic for 6-12 months are shown in Table 3. Although there were no differences in the rate of prolapse and diarrhea between the two groups (0 vs. 0; 1/18, 5.56% vs. 1/19, 5.26%), the rates of recurrence, intestinal obstruction, retraction, constipation, and diaper rash were all lower in Group 2 than in Group 1.
| Index | Open Group | Laparoscopy Group | P value |
|---|---|---|---|
| Cases | 19 | 18 | - |
| Recurrence | 1/19, 5.26% | 0 | <0.05 |
| Intestinal obstruction | 2/19, 10.5% | 0 | <0.05 |
| Retraction | 2/19, 10.5% | 0 | <0.05 |
| Prolapse | 0 | 0 | >0.05 |
| Constipation | 1/19, 5.26% | 0 | <0.05 |
| Diarrhea | 1/19, 5.26% | 1/18, 5.56% | >0.05 |
| Diaper rash | 2/19, 10.5% | 1/18, 5.56% | <0.05 |
| Anal stenosis | 2/19, 10.5% | 0 | <0.05 |
Table 3. The comparison of followed-up data (6-12months) between Laparoscopy and Open group.
Discussion
TERPT for HSCR has been popular, and includes the standard Swenson, Duhamel, and Soave procedures, as well as various modified procedures [15-17]. The most common type of HSCR has been treated by primary radical repair; for most long-type and some common-type HSCR cases in newborns with enterocolitis or colonic perforation, one-stage life-saving colostomy was necessary, followed by two-stage radical repair 3-6 months after colostomy, once nutritional status was improved. Since laparoscopic surgical treatment for HSCR was first described by Georgeson [19,20], the primary laparoscopic-assisted, endorectal colon pull-through has been the standard treatment for HSCR [20,21]. The desire to reduce scarring and pain and decrease recovery time and the time to return to routine activity has gained increasing attention, and has led to more single-incision laparoscopic procedures (SILS) [22,23].
Just as trans-colostomy SILS combined with Soave TERPT was used to treat HSCR patients after one-stage colostomy in this article, scarring can be reduced and abdominal wound infection can be prevented by placing a TriPort in the abdominal wall colostoma instead of performing open surgery with associated significant trauma. In addition to the cosmetic benefit, laparoscopy offers excellent intraoperative visualization of small structures and great surgical accuracy [24,25]; incidental injury due to lysis of adhesions, intestinal loop perforation, or splenic injury can be effectively avoided, which can reduce intraoperative blood loss and the rate of postoperative intestinal obstruction caused by recurrent adhesions [21,26]. As a result, postoperative feeding resumed earlier and hospitalization days were reduced.
We also found that the rate of postoperative enterocolitis, recurrence, anal stenosis, constipation, and retraction were lower in the laparoscopic group, mainly because of the prevention of strong tension between the anal stoma and left colon. Because laparoscopy is a deep and accurate procedure, the colon can be isolated sufficiently and the mesenteric vasculature can be selectivity spared; adequate blood supply can thus be achieved [27,28]. Laparoscopy has generally not been suitable in the presence of abdominal adhesions. However, with open implantation of a TriPort, perforations can be avoided, adhesions can be effectively isolated, and incidental injury due to adhesion lysis, as well as adhesion recurrence, can also be effectively avoided. In our experience, SILS combined with Soave TERPT to treat HSCR patients after one-stage colostomy is safe and effective. Although significant experience is required, this procedure offers significant advantages. With the development of laparoscopic techniques, this procedure should be widely implemented, and more experience will thereby be obtained.
References
- Kusafuka T, Wang Y, Puri P. Novel mutations of the endothelin-B receptor gene in isolated patients with Hirschsprung's disease. Hum Mol Genet 1996; 5: 347-349.
- Granstrom AL, Husberg B, Nordenskjold A, Svensson PJ, Wester T. Laparoscopic-assisted pull-through for Hirschsprung's disease, a prospective repeated evaluation of functional outcome. J Pediatr Surg 2013; 48: 2536-2539.
- Bagwell CE, Langham MR Jr, Mahaffey SM, Talbert JL, Shandling B. Pseudomembranous colitis following resection for Hirschsprung's disease. J Pediatr Surg 1992; 27: 1261-1264.
- Kim AC, Langer JC, Pastor AC, Zhang L, Sloots CE, Hamilton NA, Neal MD, Craig BT, Tkach EK, Hackam DJ, Bax NM, Dillon PA, Chamberlain JN, Teitelbaum DH. Endorectal pull-through for Hirschsprung's disease-a multicenter, long-term comparison of results: transanal vs. transabdominal approach. J Pediatr Surg 2010; 45: 1213-1220.
- Miyano G, Ochi T, Lane GJ, Okazaki T, Yamataka A. Factors affected by surgical technique when treating total colonic aganglionosis: laparoscopy-assisted versus open surgery. Pediatr Surg Int 2013; 29: 349-352.
- Frykman PK, Short SS. Hirschsprung-associated enterocolitis: prevention and therapy. Semin Pediatr Surg 2012; 21: 328-335.
- Aslanabadi S, Ghalehgolab-Behbahan A, Zarrintan S, Jamshidi M, Seyyedhejazi M. Transanal one-stage endorectal pull-through for Hirschsprung's disease: a comparison with the staged procedures. Pediatr Surg Int 2008; 24: 925-929.
- Oancea M, Vatra L, Kadar A, Cop?escu C. Laparoscopic approach for rectosigmoidian resection in children. J Chirurgia 2014; 109: 117-122.
- Tang ST, Yang Y, Li SW, Cao GQ, Yang L, Huang X, Shuai L, Wang GB. Single-incision laparoscopic versus conventional laparoscopic endorectal pull-through for Hirschsprung's Disease: A comparison of short-term surgical results. J Pediatr Surg 2013; 48: 1919-1923.
- Tang ST, Yang Y, Wang GB, Tong QS, Mao YZ, Wang Y, Li SW, Ruan QL. Laparoscopic extensive colectomy with transanal Soave pull-through for intestinal neuronal dysplasia in 17 children. World J of Pediatr 2010; 6: 50-54.
- Langer JC, Minkes RK, Mazziotti MV, Skinner MA, Winthrop AL. Transanal one-stage Soave procedure for infants with Hirschsprung’s disease. J Pediatr Surg 1999; 34: 148-151.
- Rothenberg SS, Shipman K, Yoder S. Experience with modified single-port laparoscopic procedures in children. J Laparoendosc Adv Surg Tech A 2009; 19: 695-698.
- Muensterer OJ, Adibe OO, Harmon CM, Chong A, Hansen EN, Bartle D, Georgeson KE. Single-incision laparoscopic pyloromyotomy: initial experience. Surg Endosc 2010; 24: 1589-1593.
- Georgeson KE, Robertson DJ. Laparoscopic-assisted approaches for the definitive surgery for Hirschsprung’s disease. J Seminars in Pediatr Surg 2004; 13: 256-262.
- Li AW, Zhang WT, Li FH, Cui XH, Duan XS. A new modification of transanal Soave pull-through procedure for Hirschsprung’s disease. Chin Med J (Engl) 2006; 119: 37-42.
- Shen C, Song Z, Zheng S, Xiao X. A comparison of the effectiveness of the Soave and Martin procedures for the treatment of total colonic aganglionosis. J Pediatr Surg 2009; 44: 2355-2358.
- De la Torre-Mondragón L, Ortega-Salgado JA. Transanal endorectal pull-through for Hirschsprung's disease. J Pediatr Surg 1998; 33: 1283-1286.
- Wang L, He Q, Jiang J, Li N. Long-term outcomes and quality of life after subtotal colectomy combined with modified Duhamel procedure for adult Hirschsprung’s disease. Pediatr Surg Int 2014; 30: 55-61.
- Georgeson KE, Fuenfer MM, Hardin WD. Primary laparoscopic pull-through for Hirschsprung’s disease in infants and children. J Pediatr Surg 1995; 30: 1017-1022.
- Wang L, He Q, Jiang J, Li N. Long-term outcomes and quality of life after subtotal colectomy combined with modified Duhamel procedure for adult Hirschsprung's disease. J Pediatr Surg Int 2014; 30: 55-61.
- Ruggeri G, Randi B, Gargano T, Libri M, Maffi M, Lima M. Technical Modification of the Georgeson Procedure for Hirschsprung’s Disease. J Endoscopic, Minimally Invasive Surgery in Newborn, Children and Adolescent 2014; 2: 2.
- Vestweber B, Galetin T, Lammerting K, Paul C, Giehl J, Straub E, Kaldowski B, Alfes A, Vestweber KH. Single-incision laparoscopic surgery: outcomes from 224 colonic resections performed at a single center using SILS (TM). J Surgical Endoscopy 2012; 27: 434-442.
- Chow A, Aziz O, Purkayastha S, Darzi A, Paraskeva P. Single incision laparoscopic surgery for acute appendicitis: feasibility in pediatric patients. Diagn Ther Endosc 2010; 2010: 294958.
- Zhu T, Feng J, Zhang W, Wei M, Yu D, Zhang X, Yu K, Kuang H. Subtotal colectomy with a single-incision laparoscopic surgery technique in children with long-segment Hirschsprung disease and allied disorders. Pediatr Surg Int 2013; 29: 197-201.
- Wang J, Zhang W, Sun D, Zhang Q, Liu H, Xi D, Li A. Laparoscopic treatment for choledochal cysts with stenosis of the common hepatic duct. J Am Coll Surgeons 2012; 214: e47-52.
- Zhao B, Liu T, Li Q. Comparison of the efficacy and safety of laparoscopic-assisted operations and open operations for Hirschsprung's disease: evidence from a meta-analysis. Int J Clin Exp Med 2015; 8: 12963-12969.
- van de Ven TJ, Sloots CE, Wijnen MH, Rassouli R, van Rooij I, Wijnen RM, de Blaauw I. Transanal endorectal pull-through for classic segment Hirschsprung's disease: with or without laparoscopic mobilization of the rectosigmoid? J Pediatr Surg 2013; 48: 1914-1918.
- Travassos DV, Bax NM, van der Zee DC. Duhamel procedure: a comparative retrospective study between an open and a laparoscopic technique. Surg Endosc 2007; 21: 2163-2165.