Research Article - Biomedical Research (2017) Volume 28, Issue 4
Comparison of preoperative and postoperative approaches to ultrasoundguided transversus abdominis plane block for postoperative analgesia in total abdominal hysterectomy
Dirican B, Erdogan M*, Ucar M, Uzgul U, Gulhas N, Kayhan G and Durmus MDepartment of Anaesthesiology and Reanimation, Inonu University, Turkey
- *Corresponding Author:
- Erdogan M
Department of Anaesthesiology and Reanimation
Inonu University, Turkey
Accepted date: September 16, 2016
Abstract
Background: Transversus Abdominis Plane (TAP) block produces more effective postoperative analgesia and significantly reduces consumption of postoperative opioids after various abdominal surgeries. It can be performed either preoperatively or postoperatively. Furthermore studies investigating the ideal period for TAP block administration are few. The objective of our study was to investigate, which period is more effective for administration of TAP block on postoperative analgesia in patients undergoing total abdominal hysterectomy.
Methods: This prospective randomized controlled double-blind study was conducted with 60 patients between the ages of 18-65 and ASA class I-II who were scheduled to undergo total abdominal hysterectomy. Patients who received a TAP block with ultrasound guidance prior to the surgical procedure were referred to as Group 1, the TAP block procedure after surgery made up Group 2. The rest and movement period Visual Analog Score (VAS), sedation score, nausea, vomiting and the need for additional analgesics were recorded at 2, 4, 6, 12 and 24 hours postoperatively.
Results: When Group 1 was compared with Group 2, the rest period pain scores were significantly lower in Group 2 at 2 and 4 hours (p<0.05). In Group 2, the 24-hour morphine consumption was significantly lower than that of Group 1 (p<0.05).
Conclusion: Post-operative administration of an US guided TAP block in total hysterectomy patients significantly decreased pain scores in early periods and also reduced 24 hour morphine consumption when compared with preoperative administration of the block.
Keywords
Transversus abdominis plane block, Ultrasound machines, Analgesia, Postoperative, Abdominal surgery
Introduction
Transversus Abdominis Plane (TAP) block is a useful strategy to reduce opioid consumption and support the management of postoperative pain [1,2]. Ultrasound (US) provides better localization and successful procedures. There are growing interest in the use of US with TAP block [2,3]. It has been reported that TAP block is safe and successful as an adjunct to analgesia outcome after various abdominal surgery [4-6]. TAP block characteristics can be associated with type of surgery, volume of local anaesthetic solution and timing of injection. Although optimal time for administration of the TAP block has been recommended preoperative period the in few publication, it can be performed either preoperatively or postoperatively [2,5]. Furthermore studies investigating the ideal period for TAP block administration are few. The objective of our study was to investigate, which period is more effective for administration of the TAP block using US guide on postoperative analgesia in patients undergoing total abdominal hysterectomy.
Materials and Methods
This prospective randomized double-blind study was conducted on 60 patients between the ages of 18-65 with ASA classes I-II who were scheduled to undergo total abdominal hysterectomy via a Pfannenstiel incision. The study was carried out between February 2013 and December 2013 at Turgut Ozal Medicine Center, Malatya, Turkey. This study was conducted after obtaining written consent from all patients and approval from the Inonu University Faculty of Medicine Ethics Committee, Malatya, Turkey. Patients were excluded if they had a history of allergy to the drugs used in the study protocol or had coagulation pathology, opioid tolerance, diabetes mellitus or hypertension. Patients were divided into two groups by using computer generated randomization. Patients who received an US guided TAP block prior to the surgical procedure (starting with the skin incision) following the induction of standard general anaesthesia allocated in Group 1, the patients who underwent the TAP block procedure after surgery (following skin suture and closure) allocated in Group 2. All patients received information about the Visual Analogue Scale (VAS) and the PCA (Patient Controlled Analgesia) device, which was implanted post operatively. Both patients and postoperative raters were blinded to the establishment of TAP block. Assignments of the study group maintained concealed until data were collected.
Premedication was not administered to any patient; Electrocardiography (ECG), Peripheral Oxygen Saturation (SpO2), and Non-invasive Blood Pressure (NIBP), Heart Rate (HR) and Bispectral Index (BIS) monitoring were performed. Induction of anaesthesia was accomplished with 1 μg/kg remifentanil, 2 mg/kg propofol and 0.1 mg/kg vecuronium; standard monitoring was performed. Maintenance of anaesthesia was continued with desflurane at a concentration of 6-8% in a mixture of 60% N2O+40% O2. All TAP blocks were performed by the same experienced anaesthetist. The TAP block was performed bilaterally with real-time US-guide using a 6-13 MHz linear probe (Esaote MyLab™Five, Italy), and 22 G 80 mm needle (Pajunk Sonoplex Nanoline Stim Cannula, Germany), in-plane technique. US probe was placed transversely in the flank between the anterior superior iliac spine and the costal margin. The external oblique muscle, the Internal Oblique Muscle (IOM) and Transversus Abdominis Muscle (TAM) were identified using US. Aspiration was conducted and the needle placement was verified by administering a 1 mL local anaesthetic test dose following the placement of the needle between IOM and TAM.
The local anaesthetic solution was injected after confirming with US that the solution was spreading in the plane between the IOM and the TAM. Two 20 ml syringes were prepared with a local anaesthetic concentration of 1.5 mg/kg 0.5% bupivacaine diluted to 40 mL with saline. These were administered to the left and right abdominal walls. IV acetaminophen 1000 mg was started to all patients before extubation. IV acetaminophen 1000 mg and oral ketorolac 30 mg every 6 hours combined with PCA morphine in both groups for multimodal analgesia. Patients were extubated after reversal of the muscle relaxant agent at the end of the operation and were taken to the Post-Anaesthesia Care Unit (PACU). The primary outcome measure in our study was 24 hours morphine consumption. Secondary outcomes were pain score at rest and on movement, sedation scores, nausea and vomiting. Following assessment of the VAS score, the first morphine dose was administered to patients with a VAS score of 3 or more via a PCA device. The PCA morphine protocol was as follows: 10 mL morphine sulphate (100 mg) was prepared with 90 mL saline. The PCA device with a lockout time of 15 minutes and an intermittent bolus of 2 mg was used.
Patients were observed in the PACU for at least 30 minutes and were transferred to the postsurgical ward when their vital signs stabilized. The rest period VAS, movement period VAS, sedation score, nausea and vomiting, and the need for additional analgesics and anti-emetics were recorded by researchers who were blinded to the study groups at 2, 4, 6, 12 and 24 hours post operatively. The VAS scores were: 0=no pain, 1, 2, 3, 4, 5, 6, 7, 8, 9, and 10=excruciating pain. Nausea was measured using a 4-point categorical scoring system (no nausea=0, mild=1, moderate=2, and severe=3). A dose of 10 mg metoclopramide was used for the treatment of nausea and vomiting. Sedation was measured using a 4-point sedation scale (0=awake, 1=prone to sleeping, 2=asleep, easy to rouse, and 3=deep sleep). In a previous study, effective post-operative analgesia of TAP block has been evaluated in patients undergoing abdominal surgery, a power analysis with an alpha error of 0.05 and a beta error of 0.20 revealed that a minimum of 14 patients were required in each group, when a 24 hours morphine requirement of 60 mg, with a standard deviation ± 10 mg was considered [7]. We decided to enrol 30 patients per group into the study to minimize any effect of data loss.
Statistical analyses were performed using the SPSS 16.0 statistical package. Data were expressed as the mean ± standard deviation (mean ± SD) or case (patient) frequency and percentage. The data related to normal distribution were confirmed by Shapiro-Wilk test. The independent samples t-test was used for the comparison of dual-group averages. The Yates corrected chi-square test was used for the comparison of need for additional analgesia and the comparison of side effects. Variables with p>0.05 were considered to have a normal distribution. Statistically, p<0.05 was regarded as significant and p<0.01 was regarded as highly significant.
Results
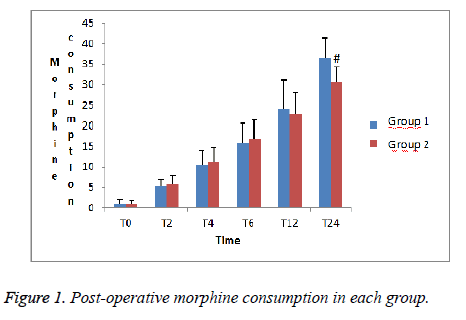
A total of 60 patients were included in our study. The patients were similar in terms of demographic characteristics and duration of surgery (p>0.05), (Table 1). The 24 hours cumulative morphine consumption was significantly lower in Group 2 when compared with Group 1 (p<0.05), (Figure 1)
| Group 1 (n=30) | Group 2 (n=30) | |
| Weight (kg) | 76.6 ± 11.9 | 72 ± 10.1 |
| Age | 49.3 ± 7.4 | 50.9 ± 5.8 |
| Height (cm) | 158 ± 4.0 | 161 ± 6.0 |
| Duration of surgery (min) | 173 ± 51.2 | 169 ± 53.6 |
| Nausea (no/mild/moderate/severe) | 26/3/1/0 | 25/4/1/0 |
| Vomiting | 1 | 1 |
| Group 1=preoperative administration of TAP block; Group 2=post-operative administration of TAP block. | ||
Table 1: Demographic characteristics and duration of surgery.
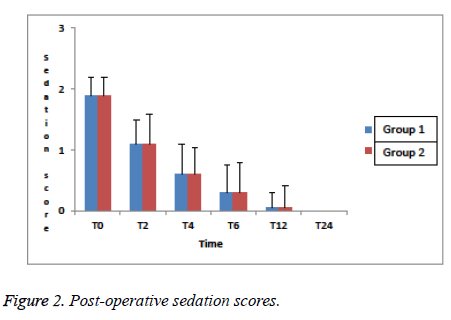
When Group 1 was compared with Group 2, VAS pain scores at rest were significantly lower in Group 2 at 2 and 4 hours (p<0.05), (Table 2). VAS pain scores on movement were similar in all monitoring periods in the both groups (p>0.05), (Table 3). There was no significant difference between the two groups in terms of nausea and vomiting (p>0.05), (Table 1). Sedation scores were similar in both groups and no excessive sedation was observed (p>0.05), (Figure 2).
| Group 1 (n=30) | Group 2 (n=30) | |
|---|---|---|
| T0 | 5.5 (3-7) | 5.7 (4-7) |
| T2 | 5.1 (2-6) | 4 (2-5)* |
| T4 | 4 (2-5) | 3 (1-4)* |
| T6 | 3 (1-4) | 3 (1-4) |
| T12 | 1.7(1-4) | 1.6(1-4) |
| T24 | 0.7 (1-3) | 0.7 (1-2) |
| VAS: Visual Analog Scale; Group 1=preoperative administration of TAP block; Group 2=post-operative administration of TAP block. *Indicates significantly lower VAS score compared to Group 1. (P<0.05). |
||
Table 2: Post-operative Visual Analog Scale (VAS) pain scores at rest in each group.
| Group 1 (n=30) | Group 2 (n=30) | |
|---|---|---|
| T0 | 6.5 (4-8) | 6.5 (4-8) |
| T2 | 6 (3-7) | 5.8 (3-8) |
| T4 | 5(2-7) | 5 (2-7) |
| T6 | 4 (1-6) | 4 (1-6) |
| T12 | 3 (1-5) | 3 (1-5) |
| T24 | 1.5 (1-3) | 1.5 (1-3) |
| VAS=Visual Analog Scale; Group 1=preoperative administration of TAP block; Group 2=post-operative administration of TAP block. | ||
Table 3: Post-opertive Visual Analog Scale (VAS) pain scores on movement in each group.
Discussion
Our study found that post-operative administration of the US guided TAP block significantly reduced the 24 hours cumulative morphine consumption and decreased pain scores at 2 and 4 hours after surgery compared to preoperative administration of the block in total hysterectomy patients. The TAP block has been used for post-operative analgesia in wide variety of abdominal surgeries [7-20]. However, conflicting results have been reported regarding the benefits of the TAP block. Belavy et al. [14] showed that an US guided TAP block reduced morphine consumption as a component of a multimodal analgesic regimen in caesarean patients. The study of Costello et al. [21], which was a similar study conducted on the same patient group and using the same technique, suggested that a TAP block did not increase the quality of postoperative analgesia. Despite conflicting results, many studies have indicated that the TAP block is helpful in reducing post-operative pain and early morphine requirements [5,7,12,17]. Therefore, we preferred total abdominal hysterectomy patients receiving a lower abdominal incision for multimodal post-operative analgesic to obtain which period TAP block is more effective in the present study. 24 hours cumulative IV morphine consumption was reduced by an average of 23.71 mg in TAP block [6]. Griffiths et al. obtained 34 mg mean morphine usage with TAP block. Our 24 hours cumulative morphine consumption in both groups were similar the previous study [11].
It has been reported that post-operative VAS pain score at rest and on movement were reduced after TAP block [22-24]. The VAS pain scores (scale of 0-10) were between 1 and 4 [8,12,13,16]. In our study, similar VAS scores were recorded at rest and on movement at all interval period in the both groups. TAP block can be performed with the anatomical landmark technique, blind technique or US guided [25]. The blind technique, which is also known as the pop technique, carried out using palpation alone, is associated with serious complications [26-28]. US guidance can facilitate the movement of the needle and help to control the distribution of anaesthetics to appropriate regions. US can also improve the quality of the nerve block [3]. Moreover, US guidance reduces procedure time, decreases the number of attempts, accelerates block starting time and prevents gastrointestinal organ injury [3,29]. Considering these advantages, our study was carried out using US guidance without any complication. A study investigating the ideal period for TAP block showed that preoperative TAP was superior to reduce the severity of acute pain, analgesic usage, side-effects and incidence of pain in comparison with post-operative [30]. In the previous study TAP block has been performed with blind TAP block technique, however we used US guided TAP block.
Timing injection can affect acute postoperative analgesic efficacy [2,5,31]. Abdullah et al. [2] found the following result about timing TAP block in a systematic review included 18 studies, preoperative TAP block was performed in half of the studies, and the others half performed postoperatively. De Olivera et al. [5] in a meta-analysis and suggested that the optimal timing for TAP block is in the preoperative period. Preoperative TAP block was benefit in the early period of pain at rest and decreased postoperative opioid consumption. However, preoperative TAP block was not benefit in the late period of pain at rest. In contrast to the results of these meta-analysis, postoperative TAP blocks were more benefit in the early period of pain at rest in our study; postoperative morphine consumption was also reduced [2,5]. It can explain with following. In the meta-analysis; surgeries, the number of patients and analgesic regimens used the postoperative period were differences from our study. There are some limitations to our study. First, the level of the block could not be determined because the block was performed after the induction of general anaesthesia. Second, postoperative analgesic consumption was limited to 24 hours. Third, there was no control group in our study. However, previous studies that have control group have been reported the analgesic effect of TAP block [7,12,13,16].
Conclusion
In conclusion, we found that post-operative administration of an US guided TAP block significantly decreased pain scores in early periods and also reduced 24 hours morphine consumption when compared with preoperative administration of the block in total hysterectomy patients.
References
- Bhatia N, Jyotsna Wig SA, Kaur G. Comparison of posterior and subcostal approaches to ultrasound-guided transverse abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy. J Clin Anesth 2014; 26: 294–299.
- Abdallah FW, Chan VW, Brull R. Transversus abdominis plane block: a systematic review. Reg Anesth Pain Med 2012; 37: 193-209.
- Petersen PL, Mathiesen O, Torup H, Dahl JB. The transversus abdominis plane block: a valuable option for postoperative analgesia? A topical review. Acta Anaesthesiol Scand 2010; 54: 529-535.
- Siddiqui MRS, Sajid MS, Cheek L, Baig MK. A meta-analysis on the clinical effectiveness of transversus abdominis plane block . J Clin Anesth 2011; 23: 7-14.
- De Oliveira GS Jr., Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg 2014; 118: 454-463.
- Johns N, O'Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of Transversus Abdominis Plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis 2012; 14: 635-642.
- McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg 2007; 104: 193-197.
- O'Donnell BD, McDonnell JG, McShane AJ. The Transversus Abdominis plane (TAP) block in open retropubic prostatectomy. Reg Anesth Pain Med 2006; 31: 91.
- Bharti N, Kumar P, Bala I, Gupta V. The Efficacy of a Novel Approach to Transversus Abdominis Plane Block for Postoperative Analgesia after Colorectal Surgery. Anesth Analg 2011; 112: 1504-1508.
- Walter CJ, Armonstrong CM, Pinkney TD, Conaghan PJ, Bedforth N, Gornall CB, Acheson AG. A randomised controlled trial of the efficacy of ultrasound–guided transversus abdominis plane block in laparascopic colorectal surgery. Surg Endosc 2013; 27: 2366-2372.
- Griffiths JD, Middle JV, Barron FA. Transversus Abdominis Plane Block does not provide additional benefit to multimodal analgesia in gynecological cancer surgery. Anesth Analg 2010; 111: 797-801.
- Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg 2008; 107: 2056-2060.
- McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, Laffey JG. The analgesic efficacy of transversus abdominisplane block after cesarean delivery: a randomized controlled trial. Anesth Analg 2008; 106: 186-191.
- Belavy D, Cowlishaw PJ, Howes M, Phillips F. Ultrasound-guided transversus abdominis plane block for analgesia after Caesarean delivery. Br J Anaesth 2009; 103: 726-730.
- Kanazi GE, Aouad MT, Abdallah FW. The Analgesic Efficacy of Subarachnoid Morphine in Comparison with Ultrasound Guided Transversus Abdominis Plane Block After Cesarean Delivery: A Randomized Controlled Trial. Anesth Analg 2010; 111: 475-481.
- Niraj G, Searle A, Mathews M, Misra V, Baban M, Kiani S, Wong M. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth 2009; 103: 601-605.
- El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, Kapral S, Marhofer P. Ultrasound-guided transversusabdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth 2009; 102: 763-767.
- Albrect E,Kirkham KR, Endersby RVW, Chan VWS, Jackson T, Okrainec A,Penner T, Jin R,Brull R. Ultrasound-Guided Transversus Abdominis Plane Block for Laparascopic Gastric-Bypass Surgery. Obes Surg 2013; 23: 1309-1314.
- Hosgood SA, Thiyagarajan UM, Nicholson HFL, Jeyapalan I, Nicholson ML. Randomized Clinical Trial of Transversus Abdominis Plane Block Versus Placebo Control in Live-Donor Nephrectomy. Transplantation 2012; 94: 520-525.
- Milan ZB, Duncan B, Rewari V, Kocarev M,Collin R. Sobcostal Transversus Abdominis Plane Block for postoperative analgesia in Liver Transplant Recipients. Transplant Proc 2011; 43: 2687-2690.
- Costello JF, Moore AR, Wieczorek PM, Macarthur AJ, Balki M, Carvalho JC. The Transversus Abdominis Plane Block, When Used as Part of a Multimodal Regimen Inclusive of Intrathecal Morphine, Does Not Improve Analgesia After Cesarean Delivery. Regional Anesthesia and Pain Medicine 2009; 34: 586-589.
- Peng K, Ji FH, Liu HY, Wu SR. Ultrasound-guided Transversus Abdominis Plane Block for Analgesia in Laparoscopic Cholecystectomy: A Systematic Review and Meta-analysis. Med Princ Pract 2016; 25: 237-246.
- Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block in Adult Patients: A Meta-Analysis. Anesth Analg. 2015; 121: 1640-1654.
- Gasanova I, Alexander J, Ogunnaike B, Hamid C, Rogers D, Minhajuddin A, Joshi GP. Transversus Abdominis Plane Block Versus Surgical Site Infiltration for Pain Management After Open Total Abdominal Hysterectomy. Anesth Analg. 2015; 121: 1383-1388.
- Mrunalini P, Raju NVR, Nath, VN, Saheb SM . Efficacy of transversus abdominis plane block in patients undergoing emergency laparotomies. Anesth Essays Res. 2014; 8: 377-382.
- Shivashanmugam T, Kundra P, Sudhakar S. Iliac compartment block following ilioinguinal iliohypogastric nerve block. Paediatr Anaesth 2006; 16: 1084-1086.
- Jöhr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg 1999; 88: 1051-1052.
- Farooq M, Carey M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg Anesth Pain Med 2008; 33: 274-275.
- Finnerty O, Sharkey A, McDonnell JG. Transversus abdominis plane block for abdominal surgery. Minerva Anestesiol 2013; 79: 1415-1422.
- Amr YM, Amin SM. Comparative study between effect of pre- versus post-incisional transversus abdominis plane block on acute and chronic post-abdominal hysterectomy pain. Anesth Essays Res 2011; 5: 77-82.
- Ong CK, Lirk P, Seymour R, Jenkins B. The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. Anesth Analg 2005; 100: 757-773.