- Biomedical Research (2013) Volume 24, Issue 1
Comparative study of Heart Rate Variability in normotensive offsprings of hypertensive parents.
Surekharani Chinagudi*, Anita Herur, Shailaja Patil, Shashikala G V and Roopa ADepartment of Physiology, S Nijalingappa Medical College, Navanagar, Bagalkot, Karnataka, India
- *Corresponding Author:
- Surekharani Chinagudi
Department of Physiology
S Nijalingappa Medical College
Navanagar, Bagalkot 587102, Karnataka, India
Accepted date: October 27 2012
Abstract
Hypertension or prehypertension are the diseases which affect entire body. Many times there would have been organ damage even before the diagnosis of hypertension. So it becomes very essential to diagnose hypertension or rather prehypertension at an early stage so that the preventive measures can be employed. Heart rate variability (HRV) proves to be the best tool to diagnose prehypertension at early stage. The aim of this study was to record HRV in offsprings of hypertensive parents and offsprings of normotensive parents and compare the results between the two groups. A cross sectional study was done in I MBBS students (2011-2012) of S.Nijalingappa Medical college, Bagalkot, Karnataka, India. 20 cases were obtained and were matched with 20 controls, HRV was recorded in both the groups using polyrite and analysed for time and frequency domain parameters. Statistical analysis was done by Unpaired t test using EPI-info software. The time domain parameters were found to be decreased in cases but were not statistically significant. Low frequency domain (LF) was higher and high frequency domain (HF) was lower in cases when compared to controls and the difference was statistically significant. The LF/HF ratio was also higher in cases and was statistically significant. There is increased sympathetic drive and decreased parasympathetic drive in cases when compared to controls indicating autonomic imbalance in the predisposed group. So if detected earlier, preventive measures can be undertaken to prevent prehypertension and subsequently hypertension in them.
Keywords
HRV, Prehypertension, Autonomic imbalance, Predisposed group
Introduction
Hypertension is a multifaceted progressive disease process spanning several decades of life. In all, 25% of children with one hypertensive parent and 50% of children with two hypertensive parents will eventually become hypertensive demonstrating that heredity plays a major role in the development of the disease. However, numerous other causal factors are involved, including stress, exercise, obesity, ethnicity, sex and age [1].
Hypertension runs in families, and parental history of hypertension increases the risk of developing hypertension, especially if both the parents are hypertensives [2].
Autonomic abnormality in the form of increased sympathetic tone has been demonstrated in young normotensive offsprings of hypertensive parents [3]. Though hypertension is more common in middle aged and elderly population, prehypertension is relatively more common in young adults especially in those who have family history of hypertension [3].
However, till date, not much work has been conducted to understand the nature of autonomic imbalance that facilitates the normotensive offspring of hypertensive parents to enter into a stage of prehypertension or hypertension. A recent report suggests that increased sympathetic and decreased parasympathetic activities in young adults alters the sympathovagal balance, which could be the major mechanism in the causation of prehypertension [3].
Spectral analysis of Heart rate variability has been recently used as sensitive tool for assessment of autonomic dysfunctions in various clinical disorders [4] At present spectral analysis of beat to beat cardiovascular variability has been a novel method in the assessment of risk in primary hypertension [5,6]. At present HRV investigation has superseded classic test for autonomic function because it quantifies sympathetic and parasympathetic activity [7,8].
Therefore in the present study, we have analyzed the indices of Heart Rate Variability in the offsprings of hypertensive parents and offsprings of normotensive parents to understand if there is any autonomic imbalance between the two groups.
Subjects and Methods
The present study was conducted on healthy normotensive subjects who studying in 1st year of MBBS( aged between 18 to 22 years) in S.Nijalingappa Medical College, Bagalkot, Karnataka, whose parents are hypertensive, either father or mother or both being hypertensive. Ethical clearance was obtained from the institutional ethical clearance committee.
The control group consisted of healthy normotensive subjects who are studying in 1st year of MBBS (aged between 18 to 22 years) of same college, whose both the parents are normotensive. The sample size worked out to be 20 i.e. 20 cases compared with 20 controls.Those who are known to have any cardiovascular or cardio respiratory disorders or any disease known to alter the cardiovascular hemodynamics are excluded from the study.
The subject was asked to come to the cardiovascular laboratory in S.N.Medical College, Bagalkot and asked to relax for 10 minutes. The subjects were briefed in detail about the experimental procedure. Written informed consent was taken from the subjects. Height in meters and weight in kgs were measured and BMI calculated. Baseline blood pressure was measured with sphygmomanometer. Then the ECG recorded for 5 minutes in lead II using powerlab, AD instrument polyrite which is data acquisition system and the Heart Rate Variability analyzed with respect to time and frequency domain.
In Time domain analysis the Standard deviation of all normal-to-normal intervals{SDNN(milliseconds)} was taken as index of overall HRV. Root Mean Square Successive Difference {RMSSD(milliseconds)} was also studied. Frequency domain analysis done with respect to low frequency (LF) analysis and high frequency (HF) analysis. Low frequency and high frequency spectral powers were determined by integrating the power spectrum between 0.04 and 0.15 Hz and between 0.15 and 0.4 Hz respectively. Low and high frequency power were expressed in normalized units.
The results were analyzed statistically using unpaired t test. EPI-info software and Microsoft excel were used. P value <0.05 was considered significant.
Results
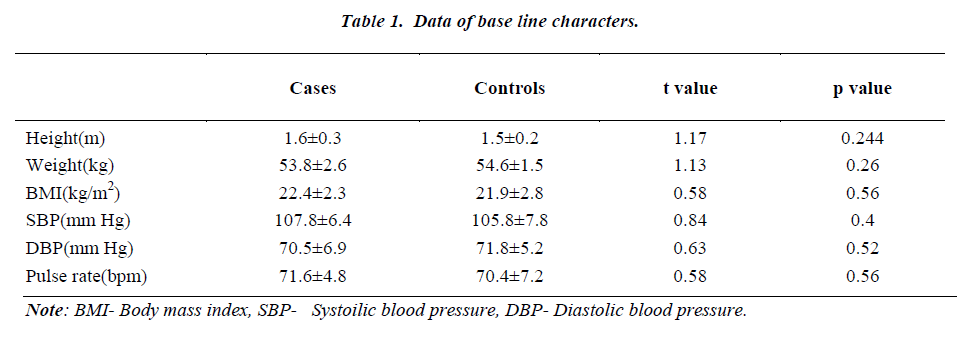
The values of all the parameters are expressed in mean ± SD. There was no significant difference in the height, weight and Body mass index(BMI) between the two groups. There was no significant difference in the systolic blood pressure (SBP) and diastolic blood pressure (DBP) between the groups. The results are depicted in Table 1.
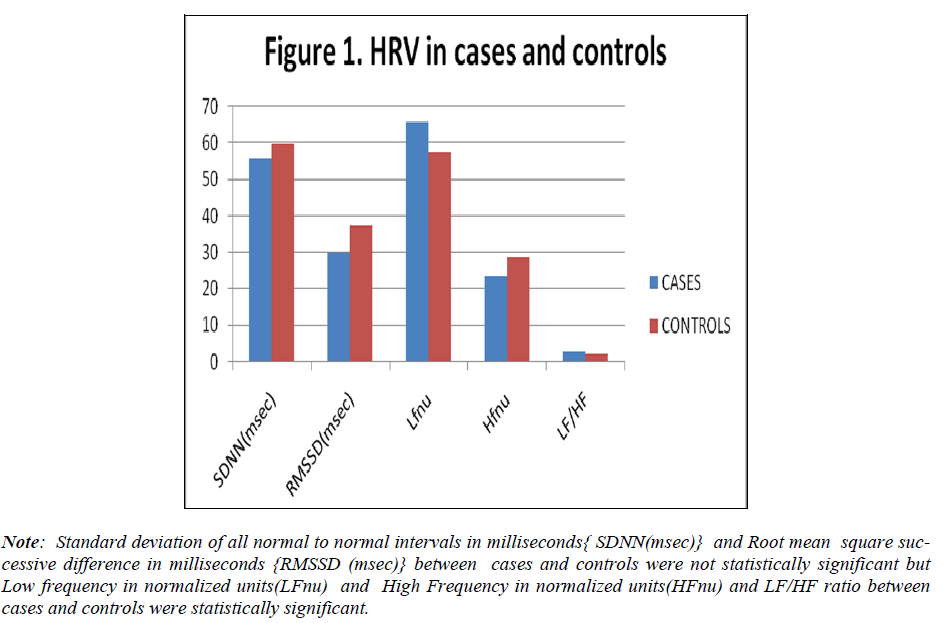
The SDNN in cases was 55.79± 22.59 and in controls was 59.9±23.93. Though it was reduced in cases but was not statistically significant. RMSSD in cases was 30.2±16.38 and in controls was 37.38±18.4. Though it was reduced in cases, it was not statistically significant. LFnu in cases was 65.75±7.44 and in controls was 57.6±16.02. LFnu was found to be higher in cases and the difference between the groups was statistically significant. The HFnu in cases was 23.78±6.15 and in controls was 28.7±6.75. HFnu was reduced in cases and the difference was statistically significant.
LF/HF ratio in cases was 2.8±1.09 and in controls was 2.1±1.02. The ratio was found to be higher in cases and the difference was statistically significant. The results are shown in Figure 1.
Figure 1: Standard deviation of all normal to normal intervals in milliseconds{ SDNN(msec)} and Root mean square successive difference in milliseconds {RMSSD (msec)} between cases and controls were not statistically significant but Low frequency in normalized units(LFnu) and High Frequency in normalized units(HFnu) and LF/HF ratio between cases and controls were statistically significant.
Discussion
As we know the role of heredity and autonomic imbalance in the pathogenesis of hypertension, we at our basic level have tried to recognize the autonomic imbalance in the risk group i.e. the offsprings of hypertensive parents, so that if recognized at the earlier stage could evaluate the preventive measures in the development of prehypertension and subsequently hypertension.
Our study showed us that there is increased LFnu and decreased HFnu and increased LF/HF ratio along with decreased SDNN in the study group i.e. normotensive offsprings of hypertensive parents when compared with controls i.e. normotensive offsprings of normotensive parents. These findings indicate that there is increased sympathetic activity and decreased parasympathetic activity in the study group when compared with the control group. Similar results have been reported by other investigators [3,9].
LF reflects the sympathetic activity when represented in the normalized units. Framingham study has shown adiposity to be the strong predictor of hypertension in men and women [10]. It is worth to note that LF component of HRV to be a strong predictor of future hypertension though BMI being a measure of adiposity. Increase in LF power was observed in recent onset hypertension [11].
Either HF in power or HFnu is the direct representation of vagal tone. Vagal tone is an important determinant of cardiovascular health. Vagal tone of an individual has insightful influence on the heart rate, cardiac output and blood pressure. Any reduction in the HF power and/or HFnu indicate decreased vagal activity [9]. In the present study HFnu was found to be significantly less in the study group when compared to control group. So our study shows early cardiovascular vagal changes in the study group.
Our study reveals increased LF/HF ratio in the study group when compared with controls which also is an indicator of sympathovagal imbalance. Many studies concur that LF/HF ratio can be used as an indicator of sympathovagal imbalance [9].
SDNN represents the long term vagal modulation of cardiac functions. A lower SDNN indicates diminished baroreflex modulation of RR intervals. In our study though there was decrease in SDNN, it was not statistically significant. Decreased SDNN along with decreased HF would indicate poor vagal control in the study group.
There was decreased RMSSD in the study group when compared with the control group. RMSSD reflects vagal modulation of heart rate, and therefore RMSSD is considered as an important short term indicator of parasympathetic drive [7].
So the present study reveals that incidence of prehypertension and the risk of cardiovascular dysfunction linked to their degree of sympathovagal imbalance is more in the offsprings of hypertensive parents than in the offsprings of normotensive parents. Sympathovagal imbalance in the form of increased sympathetic drive and decreased parasympathetic drive would lead to causation of prehypertension in these genetically predisposed individuals.
Though the baseline blood pressure values were normal in both the groups, it was by HRV the autonomic imbalance could be made out in the study group. So recording of HRV in the predisposed group becomes mandatory to prevent them from progressing to prehypertension and hypertension subsequently. As a preventive measure, the predisposed group i.e. offsprings of hypertensive parents should aim at decreasing the sympathetic drive and increasing their parasympathetic drive which can be achieved by slow breathing exercises [12,13].
Conflict of interest statement: No conflict of interest.
References
- Schneider GM, Jacobs DW, Gevirtz RN and O’Connor DT. Cardiovascular hemodynamic response to repeated mental stress in normotensive subjects at genetic risk of hypertension: evidence of enhanced reactivity, blunted adaptation, and delayed recovery. Journal of human hypertension 2003; 17: 829-840.
- Wang NY, Young JH, Meoni LA, Ford DE, Erlinger TP, Klag MJ. Blood pressure change and risk of hypertension associated with parental hypertension: the john’s Hopkins precursor study. Archieves of Internal Medicine 2008; 168(6): 643-648.
- Pal GK, Pal P, Nanda N, Lalita V, Datta TK, Adithan C. Sympathovagal Imbalance in Prehypertensive. Offsprings of Two Parents versus One Parent Hypertensive. International Journal of Hypertension 2011; doi:10.4061/2011/263170.
- Milliani A. Heart Rate Variability: from bench to bedside. European journal of internal medicine2005; 16(1): 12-20.
- Pagani M, Lucini D. Autonomic Dysregulation in essential Hypertension, insight from Heart and Arterial Blood Pressure Variability.Auton Neurosci 2001; 90:76-82.
- Huikuri HV, Ylitalo A, Sirkku MP, Ikaheimo MJ, Aivaksinen KEJ, Rantala AO et al. Heart Rate Variability In Systemic Hypertension. Am J Cardiol 1996; 77(12): 1073-1077.
- Task Force Report: Task Force Of The European Society Of Cardiology and The North American Society Of Pacing And Electrophysiology. Heart Rate Variability: Standards Of Measurement, physiological interpretation and clinical use. Circulation 1990; 93: 1043-1065.
- Bailey JJ, Berson AS, Garson A Jr, Horan LG, Macfarlane PW, Mortara DW et al. Recommendations for standardization and specifications in automated electrocardiography. Circulation 1990; 81: 730-739.
- Krishnan Muralikrishnan, KabaliBalasubramanian and Badanidiyur Vishwanatha Rao. Heart Rate Variability In Normotensive Subjects With Family History of Hypertension . Indian J Physiol Pharmacol 2011; 55(3):253-261.
- Garrison RJ, Kannel WB, Stokes J III, Castelli WP. Incidence and Precursors of Hypertension in Young Adults: the Framingham Offspring Study. Prev Med 1987; 16: 235-251.
- Prakash ES, Madanmohan, Sethuraman KR, Narayanan SK. Cardiovascular Autonomic Regulation In Subjects With Normal Blood Pressure, High- Normal blood pressure And Recent Onset Hypertension. Clin Exper Pharmacol Physiol 2005; 32(5-6): 488-494.
- Pramanik T, Sharma HO, Mishra S, Mishra A, Prajapathi R and Singh S. Immediate Effect Of Slow Pace Bhastrika Pranayama On Blood Pressure and Heart Rate. Journal of Alternative and Complimentary Medicine 2009; 15(3): 293-295.
- Wang SZ, Li S, Xu XY, Lin GP, Li S, Zhao Y et. Al. Effect of slow abdominal breathing combined with biofeed back on blood pressure and heart rate variability in prehypertension. Journal Of Alternative and Complimentary Medicine 2010; 16(10): 1039-1045.