Research Article - Journal of Oral Medicine and Surgery (2022) Volume 5, Issue 6
Comparative evaluation of two different fixation systems using two mm titanium mini plates and 3Dlocking plate in the treatment of symphysis and parasymphysis fractures of mandible
Ravinder Pal Singh Rana*, Nanda Kishore Sahoo, Sujit Kumar Bhandari
Department of Dental Surgery and Oral Health Sciences, Armed Forces Medical College, Pune, India
- *Corresponding Author:
- Ravinder Pal Singh Rana
Department of Dental Surgery and Oral Health Sciences
Armed Aorces Medical College, Pune, India
E-mail: nicedentistrana@ gmail.com
Received: 01-Nov-2022, Manuscript No. AAOMT-22-78764; Editor assigned: 02- Nov-2022, PreQC No.AAOMT-22-78764(PQ); Reviewed: 18-Nov-2022, QC No.AAOMT-22-78764; Published: 29-Nov-2022, DOI: 10.35841/aaomt-5.6.126
Citation: Rana RPS. Comparative evaluation of two different fixation systems using two mm titanium mini plates and 3dlocking plate in the treatment of symphysis and parasymphysis fractures of mandible. J Oral Med Surg. 2022;5(6):126
Abstract
Purpose: To evaluate the efficacy of two mm titanium miniplates and screws versus 3D locking plates and screws in patients with symphysis and parasymphysis fractures of mandible. Patients and Methods: A prospective comparative study consisted of patients with symphysis and parasymphysis fractures of mandible reporting to our department and was divided randomly but equally. For patients in Group a conventional two mm miniplates were used and in Group B fracture segments were fixed by using 3-D locking plates. Results: Sample consisted of 42 patients, 21 in each group and was divided by simple random sampling. Patients were reviewed on the first, fourth and twelfth week to compare post-surgical parameters including reduction and stability, masticatory comfort, rate of recovery from preoperative paraesthesia, rate of bone healing complication rateusing two different fixation systems. Both of these osteosynthesis systems were not found to have any clinically significant difference on the above mentioned parameters (P-value>0.05). Conclusion: The results of this study showed that 3D locking plate is an alternative approach with a similar outcome to miniplates in the management of fractures of mandible symphysis and parasymphysis but cases of oblique fractures and those involving the mental nerve limits its usage where miniplates fixation is more viable clinically.
Keywords
Fracture, Symphysis, 3D Locking plates, Miniplates.
Introduction
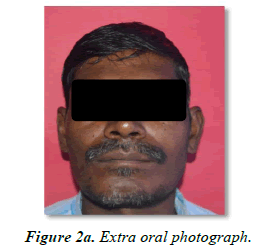
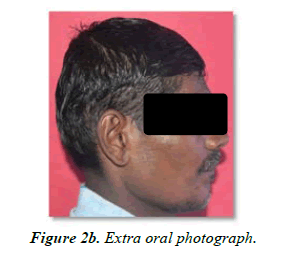
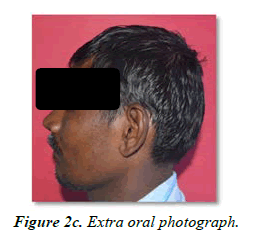
The face is a prominent part in the body and is well supported with facial bones and soft tissues [1]. Fracture of these facial bones can be caused due to road traffic accidents (RTA), falls, sport injuries, interpersonal assaults and industrial accidents [2]. When these injuries occur on face, it disrupts daily lifestyle of chewing, breathing, talking, smell and vision. Impairment of these functions can cause potentially serious effects on quality of life [3]. Although mandible is a solid bone, it has a prominent place in the face and hence is prone to injuries (Figure 2a to 2f). Hansman was the first to develop procedure of subcutaneous fixation with plate and screws [4]. Miniplate osteosynthesis was introduced in 1973 by Michelet and developed further by Champy [5]. These plating systems provide stability by the head of screw compressing the fixation plate to the bone as the screw is tightened. Under ideal conditions, the system remains stable till the fracture has healed. With development of different design of osteosynthesis material, fracture management has become easy and comfortable. Miniplate fixation is most popular and has become a standard, as fixation can be achieved intra-orally avoiding extra-oral incision [6].
Over a period of time however, the cortex of bone adjacent to the plate resorbs leading to loosening of hardware and infection [7]. This problem has been overcome by the development of screw which locks not only to the bone but to the bone plate as well resulting in an effective mini-internal fixation [8]. These locking plate and screws are expected to have certain advantages over conventional miniplate and screw osteosynthesis. It does not allow stripping and loosening of screws. Plates do not need to be precisely adapted and hence plate bending is simplified [9]. Hardware loosening following osteosynthesis is minimized or eliminated. There is less interference in bone healing even in cases of compromised vascularity [10]. Therefore, this prospective comparative study aims to evaluate two different fixation systems using 2 mm titanium mini plates and 3D locking plates in the treatment of symphysis and parasymphysis fractures of mandible.
Material and Methods
Material
This study consisted of patients with symphysis and parasymphysis fractures of mandible reporting to the department of oral and maxillofacial surgery Armed forces medicial college, Pune, India. A sample of 42 patients were divided randomly but equally using simple random sampling (SRS) into two groups and all of these were treated with open reduction and internal fixation. For patients in Group A conventional 2 mm miniplates was used as the method of fixation and in Group B fracture segments were fixed by using 3-D locking plates.
Inclusion criteria
• Clinical and radiological diagnosis of symphysis and parasymphysis fractures of mandible
• Parasymphysis fractures associated with additional fractures of mandible like body, condyle or angle fracture
• Age more than 18 years but less than 65 years of age
Exclusion criteria
• Previous history of lower face fractures and/or surgical procedures
• Patients with communited factures of the mandible
• Patients with infected fractures of the mandible/ cases with osteomyelitis
• Patients with associated midface fractures
• Patients with systemic diseases that may affect bone healing
• Patients on bisphosphonate therapy
• Patient with history of allergy to titanium implants/ materials
Place of study
This study was carried out in a tertiary care hospital in Western Maharashtra.
Nature of study
Prospective: Comparative Study
Period of study
1 year and 4 months i.e. from 02 Mar 19 to 30 Jun 2020
Armamentarium
a. Equipment for radiographic examination:
(i) Cone beam computed tomography (NewTom GiANO, High Frequency, Stationary Anode: 60-90 kV; 1-10 mA 0.5 mm focal spot dimension)
(ii) Computed Tomography Machine (Siemens Somatom Emotion 16 x 0.6 mm/16 x 1.2mm slice)
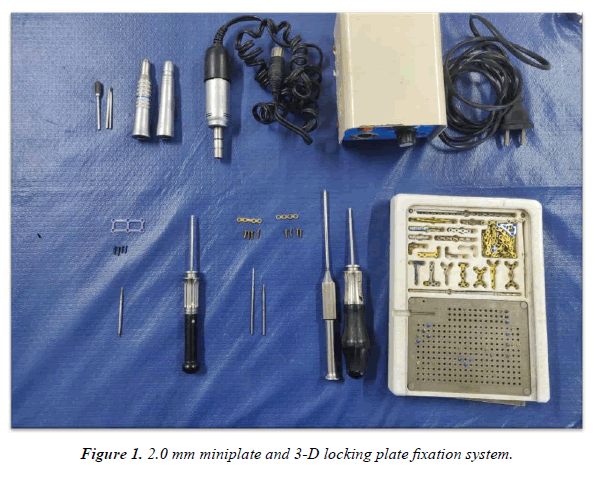
a. 2.0 mm miniplate fixation system (Figure 1):
(i) Titanium 2.0 miniplate profile thickness 1.0 mm
(ii) Titanium self - tapping screws 6-8 mm length and 2mm diameter
(iii) Screwdriver and drill bits for 2.0 mm bone screws
b. 3-Dimensional plating fixation system (Figure 1):
(i) Titanium ultra-lock 3-dimensional plates 2 x 4 holes
(ii) Titanium ultra- lock screws 6-8 mm length and 2 mm diameter
(iii) Screwdriver and 1.5 mm drill bit
Methods
Steps of the conduct of the study
c. Patients with symphysis and parasymphysis fractures of mandible as fore mentioned reporting to the Division of Oral and Maxillofacial Surgery, Dept of Dental surgery and Oral Health Sciences, Armed Forces Medical College, Pune with clinical and radiological diagnosis of symphysis and parasymphysis fractures of mandible fulfilling inclusion and exclusion criteria were selected.
d. The patients were divided randomly but equally using simple random sampling method into two groups based on two different fixation systems in the treatment of symphysis and parasymphysis fractures of mandible. Group A and Group B were assigned to patients undergoing fixation with 2 mm titanium miniplates and 3D titanium locking plates respectively.
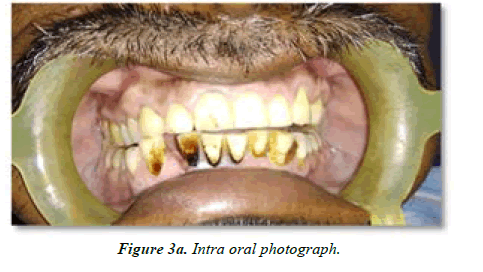
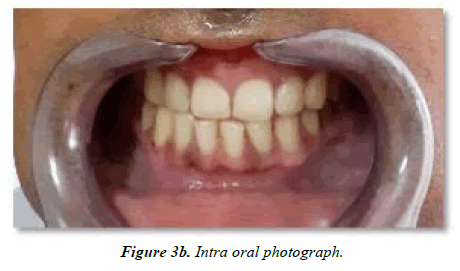
e. All the study subjects underwent thorough demographic data recording, history taking and clinical evaluation. Extra oral and intra oral photographs were taken for records (Figure 2a to 2f, Figure 3a, 3b).
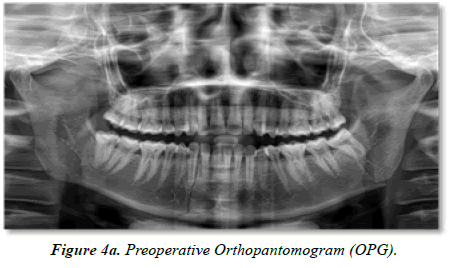
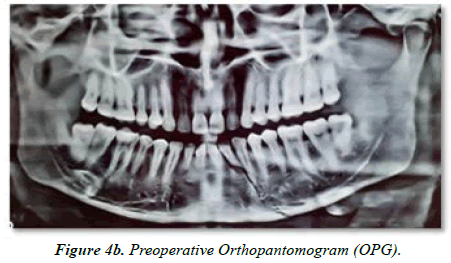
f. All patients were subjected to a preoperative radiological examination in the form of Orthopantomograms (OPG), Cone-Beam Computed Tomography (CBCT) scans or noncontrast computed tomography (NCCT) (Figure 4a, 4b).
g. Before surgery, arch bars /Intermaxillary fixation screws were secured to the upper and lower dentate arches of the patient.
h. Routine blood, urine and radiographic investigations required by anaesthesiology team were carried out, and all patients were evaluated for fitness to undergo the surgical procedure under general anaesthesia by the anaesthetic team.
i. All diagnostic procedures, the need for surgery, anaesthetic and surgical procedures were explained to the patients, and written informed consent for anaesthesia and surgery was obtained from all the participants before surgery (Annexure A).
j. Open reduction and internal fixation (ORIF) was carried out for patients in both the groups:
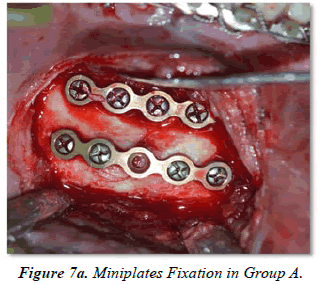
1. Group A: 21 cases were treated with 2 mm mini plate system according to the principles of Champy’s lines of osteosynthesis and zones of compression and tension.
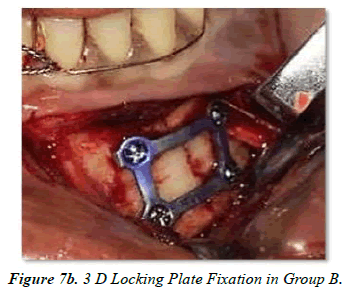
2. Group B: 21 cases were treated with 3 D locking plate system.
k. All the patients were operated under general anaesthesia (nasotracheal intubation), transoral gingivolabial and gingivobuccal incision approach or extraoral, submandibular approach (in case of an existing laceration). All surgeries were performed by an experienced faculty member of oral maxillofacial surgery. Duration of surgery was recorded for all patients.
Surgical Procedure
(i) A curvilinear incision was placed extending anteriorly out into the lip, leaving 10 to 15 mm of mucosa attached to the gingiva. Once through the mucosa, the underlying mentalis muscle fibers were sharply incised in an oblique approach and stripped from the mandible in a subperiosteal plane. Retraction of the labial tissues was facilitated by stripping them off from the inferior border of the symphysis.
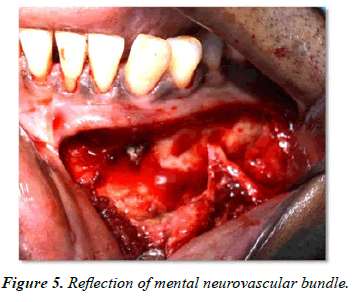
(ii) Controlled dissection and reflection of the mental neurovascular bundle was carried out to facilitate retraction of the soft tissue away from the mandible and the fracture segments were exposed (Figure 5).
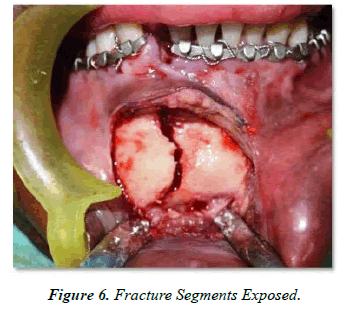
(iii) The fracture site was exposed, and fracture ends were manipulated for anatomic reduction (Figure 6).
(iv) Fixation was done either by using two standard miniplates and 2 mm x 4 monocortical screws each as per Champy’s principles of osteosynthesis in Group A or by a titanium 3D locking plate secured with 4 locking screws in Group B (Figure 7a,7b)
(v) For 3D locking plates and screws after achieving the anatomic reduction, vertical arm of the plate was placed parallel to the fracture line, drilling was done perpendicular to plate with help of drill guide, screws were placed perpendicularly to achieve proper head fit into the plate threads.
(vi) MMF was then released, and occlusion and mandibular movements were then verified, and closure was carried out in layers and a pressure dressing was placed.
l. All patients were given a standard postoperative regimen of antibiotics, analgesics and other medications as per the hospital’s policy.
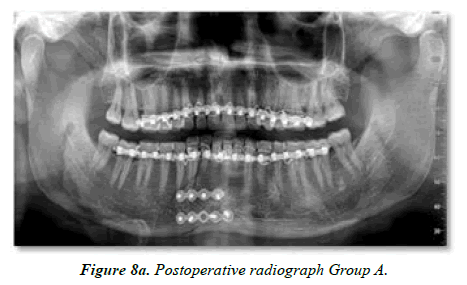
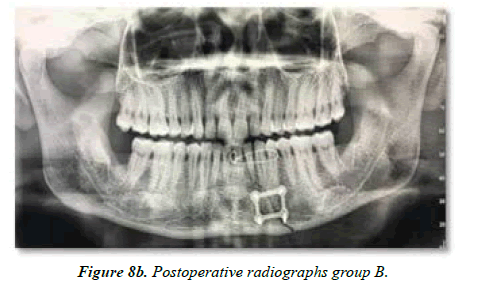
m. Postoperative radiographs were taken to assess the reduction of the fracture after 48 hours. (Figure 8a,8b).
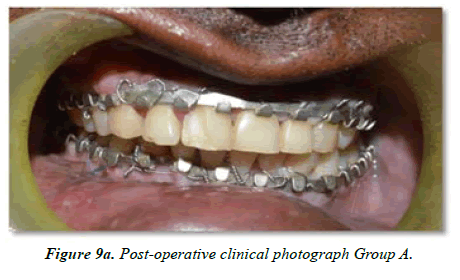
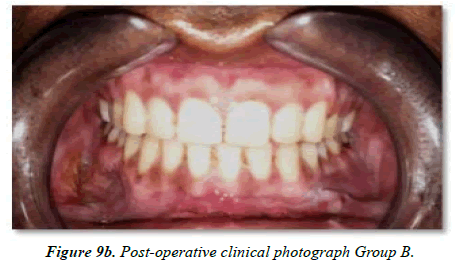
n. Once discharged, the patients were reviewed at one week, four weeks and twelve weeks postoperatively and appropriate post-operative clinical.
o. (Figure 9a, 9b) and radiographic records were obtained.
Results
The present study was a prospective comparative study undertaken to evaluate the two different fixation systems using two mm titanium mini plates and 3D locking plate in the treatment of symphysis and parasymphysis fractures of mandible.
The study included a total of 42 cases presented with the symphysis and parasymphysis fracture of mandible fulfilling the inclusion and exclusion criteria as per the study protocol.
The cases were divided in 2 groups randomly of 21 cases each using simple random sampling (SRS) procedure. Group a cases were allocated to mini plate fixation group and Group B cases were allocated to 3D locking plate fixation group.
In the entire study, the p-values less than 0.05 are considered to be statistically significant. All the hypotheses were formulated using two tailed alternatives against each null hypothesis (hypothesis of no difference). The entire data is statistically analyzed using Statistical Package for Social Sciences (SPSS ver 22.0, IBM Corporation, USA) for MS Windows.
Following section shows the detailed statistical analysis of the available data.
Inter-group distribution of mean age (Table 1)
| Age (years) | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (years) | 28.76 | 4.89 | 27.67 | 6.27 | 0.532NS |
Values are mean and SD, P-value by independent sample t tests. P-value<0.05 is considered to be statistically significant.
NS – Statistically non-significant.
Table 1. Inter-group distribution of meanage.
The mean ± SD of age of cases studied in Group A and Group B was 28.76 ± 4.89 years and 27.67 ± 6.27 years respectively. The minimum–maximum age range in Group A and Group B was 19-42 years and 19-42 years respectively.
Inter-group sex distribution of cases studied (Table 2)
| Sex | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Male | 18 | 85.7 | 16 | 76.2 | 0.697NS |
| Female | 3 | 14.3 | 5 | 23.8 | |
| Total | 21 | 100.0 | 21 | 100.0 | |
Values are n (% of cases), P-value by Chi-Square test. P-value<0.05 is considered to be statistically significant.
NS-Statistically non-significant.
Table 2. Inter-group sex distribution of cases studied.
Of 21 cases studied in Group A, 18 (85.7%) were male and 3 (14.3%) were female. Of 21 cases studied in Group B, 16 (76.2%) were male and 5 (23.8%) were female.
Inter-group distribution of mode of injury (Table 3)
| Mode of injury | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| RTA | 15 | 71.4 | 16 | 76.2 | 0.171NS |
| Fall | 3 | 14.3 | 5 | 23.8 | |
| Assault | 3 | 14.3 | 0 | 0.0 | |
| Total | 21 | 100.0 | 21 | 100.0 | |
Values are n (% of cases), P-value by Chi-Square test. P-value<0.05 is considered to be statistically significant.
NS-Statistically non-significant.
Table 3. Inter-group distribution of mode of injury (etiology).
Of 21 cases studied in Group A, 15 (71.4%) had RTA, 3 (14.3%) had fall and 3 (14.3%) had assault. Of 21 cases studied in Group B, 16 (76.2%) had RTA, 5 (23.8%) had fall and none had assault.
Inter-group and intra-group distribution of mean pain score (VAS) (Table 4)
| Pain Score (VAS) | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | (Inter-group) | |
| Pre-op | 8.76 | 0.44 | 8.71 | 0.46 | 0.733NS |
| Post-op 1 week | 7.05 | 0.80 | 7.00 | 0.77 | 0.846NS |
| Post-op 4 week | 4.62 | 0.81 | 4.90 | 0.83 | 0.264NS |
| Post-op 12 week | 2.24 | 0.54 | 2.43 | 0.59 | 0.285NS |
| P-value (Intra-group) | |||||
| Pre-op vs Post-op 1 wk | 0.001*** | 0.001*** | |||
| Pre-op vs Post-op 4 wk | 0.001*** | 0.001*** | |||
| Pre-op vs Post-op 12 wk | 0.001*** | 0.001*** | |||
Values are mean and SD, P-value (Inter-group) by independent sample t test. P-value (Intra-group) by paired t test. P-value<0.05
is considered to be statistically significant. ***P-value<0.001, NS – Statistically non-significant.
Table 4. Inter-group and intra-group distribution of mean pain score (VAS).
Inter-group distribution of mean pain score (VAS)
Distribution of mean pre-operative pain score among the cases studied did not differ significantly between two study groups (P-value>0.05).
Intra-group distribution of mean pain score (VAS)
In Group A and Group B distribution of mean pre-operative pain score among the cases studied is significantly higher compared to mean post-operative pain score at 1-week, 4-week and 12-week follow-ups (P-value<0.05 for all).
Inter-group and intra-group distribution of mean masticatory functions score (VAS)(Table 5)
| Masticatory functions Score (VAS) | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | (Inter-group) | |
| Pre-op | 2.24 | 0.44 | 2.43 | 0.51 | 0.199NS |
| Post-op 1 week | 3.57 | 0.59 | 3.86 | 0.73 | 0.172NS |
| Post-op 4 week | 6.33 | 1.02 | 6.29 | 0.96 | 0.877NS |
| Post-op 12 week | 8.48 | 0.60 | 8.43 | 0.68 | 0.811NS |
| P-value (Intra-group) | |||||
| Pre-op vs Post-op 1 wk | 0.001*** | 0.001*** | |||
| Pre-op vs Post-op 4 wk | 0.001*** | 0.001*** | |||
| Pre-op vs Post-op 12 wk | 0.001*** | 0.001*** | |||
Values are mean and SD, P-value (Inter-group) by independent sample t test. P-value (Intra-group) by paired t test. P-value<0.05 is
considered to be statistically significant. ***P-value<0.001, NS – Statistically non-significant.
Table 5. Inter-group and intra-group distribution of mean masticatory functions score (VAS).
Inter-group distribution of mean masticatory function score (VAS)
Distribution of mean pre-operative masticatory function score among the cases studied did not differ significantly between two study groups (P-value>0.05).
Distribution of mean post-operative masticatory function score at 1-week, 4-week and 12-week follow-up among the cases studied did not differ significantly between two study groups (P-value>0.05 for all) (Chart 6).
Intra-group distribution of mean masticatory function score (VAS)
In Group A and Group B, distribution of mean pre-operative masticatory function score among the cases studied is significantly lower compared to mean post-operative masticatory function score at 1-week, 4-week and 12-week follow-ups (P-value<0.05 for all).
Inter-group and intra-group distribution of neurosensory deficiency status (Table 6)
| Neurosensory deficiency status | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | (Inter-group) | ||
| Pre-op | Present | 10 | 47.6 | 9 | 42.9 | 0.999NS |
| Not present | 11 | 52.4 | 12 | 57.1 | ||
| Post-op 4-12 week | Present | 0 | 0.0 | 0 | 0.0 | 0.999NS |
| Not present | 21 | 100.0 | 21 | 100.0 | ||
| P-value (Intra-group) | ||||||
| Pre-op vs Post-op 4-12 wk | 0.001*** | 0.001*** | ||||
Values are n (% of cases), P-value (Inter-group) by Chi-Square test. P-value (Intra-group) by Wilcoxon;s signed rank test. P-value<0.05 is considered to
be statistically significant. ***P-value<0.001, NS – Statistically non-significant.
Table 6. Inter-group and intra-group distribution of neurosensory deficiency status.
Inter-group distribution of neurosensory deficiency status
Distribution of prevalence of pre-op neurosensory deficiency among the cases studied did not differ significantly between two study groups (P-value>0.05).
Distribution of incidence of post-op (4-12 weeks) neurosensory deficiency among the cases studied did not differ significantly between two study groups (P-value>0.05).
Intra-group distribution of neurosensory deficiency status
In Group A and Group B, distribution of pre-operative neurosensory deficiency status among the cases studied differs significantly compared to post-operative (4-12 weeks) neurosensory deficiency status (P-value<0.05). In other words, in group A; everyone who had neurosensory deficit pre-operatively got improved at post-operative (4-12 weeks) follow-up.
Inter-group distribution of radiographic evidence of bone healing (Table 7)
| Bone healing | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | ||
|---|---|---|---|---|---|
| N | % | n | % | ||
| Satisfactory | 18 | 85.7 | 19 | 90.5 | 0.999NS |
| Unsatisfactory | 3 | 14.3 | 2 | 9.5 | |
| Total | 21 | 100.0 | 21 | 100.0 | |
Values are n (% of cases), P-value by Chi-Square test. P-value<0.05 is considered to be statistically significant.
NS-Statistically non-significant.
Table 7. Inter-group distribution of radiographic evidence of bone healing.
Of 21 cases studied in Group A, 18 (85.7%) had satisfactory evidence of bone healing and 3 (14.3%) had unsatisfactory evidence of bone healing. Of 21 cases studied in Group B, 19 (90.5%) had satisfactory evidence of bone healing and 2 (9.5%) had unsatisfactory evidence of bone healing.
The distribution of radiographic evidence of bone healing among the cases studied did not differ significantly between two study groups (P-value>0.05).
Inter-group distribution of incidence of post-op complications (Table 8)
| Complications | Group A [Mini Plate] (n=21) | Group B [3D Locking Plate] (n=21) | P-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Absent | 19 | 90.5 | 19 | 90.5 | 0.999NS |
| Present | 2 | 9.5 | 2 | 9.5 | |
| Total | 21 | 100.0 | 21 | 100.0 | |
Values are n (% of cases), P-value by Chi-Square test. P-value<0.05 is considered to be statistically significant.
NS-Statistically non-significant.
Table 8. Inter-group distribution of incidence of post-op complications.
Patients in both the group were evaluated for any dehiscence, malunion, non-union, damage to root by screw, superficial incisional surgical site infection, neurosensory deficit, occlusal discrepancy and post-operative mobility at fracture site.
Of 21 cases studied in Group A, 19 (90.5%) did not have complications and 2 (9.5%) had post-op complications. Of 21 cases studied in Group B, 19 (90.5%) did not have complications and 2 (9.5%) had post-op complications.
Infection in one case of Group A and two cases in Group B, was found to be superficial incisional surgical site infection which was resolved with antibiotics and local oral hygiene methods. One patient of Group A during 3rd month of follow?up had a draining sinus tract which warranted excision of sinus tract under antibiotic coverage.
The distribution of incidence of post-op complications among the cases studied did not differ significantly between two study groups (P-value>0.05)
Discussion
Owing to distinctive anatomy the mandible is particularly susceptible to trauma due to its distinctive anatomy and prominent position in the face skeleton. Housman’s narrative of mandibular fixation employing plates and screws was first reported by Ewer's and Harle [11]. Since then, other authors have advocated for the adoption of several biocompatible and well-designed plating systems. The use of rigid internal fixation for maxillofacial fractures has gained popularity over the period time. The principal disadvantage of rigid plates is that they produce cortical resorption and endosteal new bone apposition on the plate's opposing side. As a result of these actions, the opposing cortex steadily moves towards the cortex plate, and more bone accumulates at the plate ends and outside screws. Historically these stresses resulting from the rigid plate are collectively known as stress protected or stress shielding osteopenia or osteoporosis [12].
Using small to medium sized bone plates on the mandiblex reduced the bone strain by 50% and had little impact on morphological and structural property of adjacent bone as smaller sized plates produce minimal physiologic stresses (less stress shielding) facilitating stimulation of the osteogenic cells and better healing [4].
In the past three decades, there has been a rapid development of techniques being applied in managing of maxillofacial trauma. The most noteworthy innovation related to the management of fractures of the mandible is based on specific technical enhancements in the internal fixation methods [13].
The universal goals of treating fractures include; restoration of accurate dental occlusion and functional jaw movements, avoid external surgical approach and prevent injury to the teeth roots, nerves and vessels. Although most surgeons agreed in general on these treatment goals but treatment modalities indicate a lack of consensus [11].
Spiessl and AO/ASIF surgeons believed in fixation that was strong enough to avoid interfragmentary motion while the mandible was in use. Primary bone union by compression osteosynthesis was the goal of treatment, and large bone plates with bicortical screws were employed. Bulky plates.
challenging adaptation, stress shielding, scar development due to extra oral approach, longer operating time, and a higher risk of nerve injury were some of the drawbacks [14].
Miniplates (Champy type) have been employed to improve the stability between bone fragments in the craniofacial region throughout the last decade and are now the preferred surgical procedure for fracture treatment. Raveh and colleagues developed a titanium reconstruction plate system (THORP – Titanium coated Hollow Screw and Reconstruction Plate System) that allowed the heads of the screws to lock into the plate's holes. The plate-to-screw lock eliminates the need for compression between the plate and mandible, which is required in a regular screw-plate system [15].
When comparing the different osteosynthesis methods, it was realized that when using miniplate fixation, increased torsion and gapping of the bone fragments occurred during screw tightening when the plates were pressed onto the bone, demonstrating the importance of precisely contouring the plate to the bone surface. The decrease remains practically unchanged if the locking system is secured using locking screws. As a result, unlike typical plating processes, the plate does not need to be shaped as accurately [16].
Self-drilling, self-tapping screws, locking miniplates, and 3D locking plates are among the most recent advances. Selfdrilling and self-tapping screws promise less instrumentation and quicker installation. They have been proven to be significantly more retentive in cancellous bone in preclinical tests. Locking miniplates use twin threaded screws to secure the plate to the bone, forming a mini-internal fixator. This results in a more rigid fixation with less fracture or osteotomy deformity. Because the plate is not placed closely on the bone, these fixations do not obstruct bone circulation. For mandibular fracture therapy, three combinations of plates in a variety of forms and lengths are offered. The thinner and medium types can be used for transoral plating of fractures with the Champy method [8].
Farmand developed a three-dimensional plate with a quadrangular configuration by merging two miniplates with interconnecting crossbars. The stability is achieved over a specific surface area in three dimensions due to its design, rather than its thickness or length, and it provides strong resistance to torsional forces. In mandibular osteosynthesis, conventional plates with a thickness of 0.9 mm are recommended. Excessive implant material due to extra vertical bars inserted to counter torque forces, difficult to adjust, and unfavourable to use in situations of fractures involving the mental nerve and oblique fractures are some of the drawbacks of 3D plates [17].
The fundamentals of 3D locking design are based on the 3D Miniplates and locking systems. The chief forces of concern when the mandible is in use are bending, vertical displacement, and shearing. The vertical bars linking the two horizontal bars in a 3D plate withstand bending forces. The plate's box structure distributes forces throughout a surface area rather than along a single line, resulting in greater three-dimensional stability against torsion forces, vertical displacement, bending, and shearing forces. As a result, three-dimensional stability is gained, hence the name 3D plate. The screw and plate becomes a single rigid functional unit in the locking mechanism, and stabilisation is no longer reliant on the bone-plate interface [7]. The locking system combines two principles: first, it inhibits screw stripping and movement, as well as loosening; and second, the fixator principle simplifies plate bending and reduces torsion or opening at the fracture point. The lack of pressure beneath the plate eliminates interference with the bone's vascular supply and allows periosteum to grow beneath the plates, which aids in fracture healing.
According to the findings of this study the use of a 3D locking plate in a mandibular fracture offers the advantage of better stability, less precision in plate adaptation due to the "internal/ external fixator," and a complication rate comparable to nonlocking miniplate osteosynthesis. These locking plates eliminate the requirement for exact adaptation and eliminate the necessity for the plate to make close contact with the bone, making 3D locking plates a preferable option for treating mandibular anterior fractures. If 3D plates are not used in oblique fractures, it is reasonable to anticipate that the combined qualities of 3D plates and locking plates will result in a better treatment outcome than Champy's miniplates.
Our study is a prospective comparative that study shows that in treatment of mandibular fracture, the use of locking plates has the advantage of greater stability less precision required in plate adaptation because of the "internal/external fixator" but there was no significant difference in treatment outcomes by miniplates, and both are equally successful in the treatment of mandibular symphysis and parasymphysis fractures, with sufficient rigidity often preventing or reducing the need for intermaxillary fixation.
The accurate adaption and placement of each miniplate becomes more difficult and time consuming in situations of comminuted and severely displaced fractures with significant gap (malunited fractures), whereas the 3-D locking plate is easier and faster to use and has better biomechanical behavior. It was also deduced that placing a 3D locking plate in the mental nerve region is technically difficult and poses a higher risk of nerve injury than miniplate adaption and fixing. Based on the findings of this study, we can conclude that 3D locking plates are a viable alternative to miniplates in the therapy of mandibular symphysis and parasymphysis fractures, but their use is limited in instances involving the mental nerve and oblique fractures.
References
- Singh V, Malkunje L, Mohammad S, et al. The maxillofacial injuries: A study. Natl J Maxillofac Surg 2012; 3:166-71.
- Rahim AR, Warraich RA. Mandibular fracture osteosynthesis: A comparison of three techniques. J Pak Dent Assoc. 2009; 29(2):201-205.
- Fasola AO, Obiechina AE, Arotiba JT. Soft tissue injuries of the face: a 10 year review. Afr J Med Med Sci. 2000;29(1):59-62.
- Worthington P, Champy M. Monocotical miniplate osteosynthesis. OtolaryngolClinNorth Am. 1987;20(3):607-620.
- Sauerbier S, Schon R, Otten J E, et al. The development of plate osteosynthesis for the treatment of fractures of the mandibular body. J Cranio-Maxillofac Surg. 2008;36:251-9.
- Feller KU, Richter G, Schneider M, et al. Combination of microplate and miniplate for osteosynthesis of mandibular fractures: An experimental study. Int J Oral Maxillofac Surg. 2002;31:78-83.
- Haug RH, Street CC, Goltz M. Does plate adaptation affect stability? A Biomechanical comparison of locking and non-locking plates. J Oral Maxillofac Surg. 2002;60:1319-1326.
- Alpert B, Gutwald R, Schmelzeisen R. New innovations in craniomaxillofacial ?xation: the 2.0 lock system. Keio J Med. 2003;52 (2): 120–7.
- Collins CP, Leonard GP, Tolas A, et al. A prospective randomized clinical trial comparing 2.0mm locking plates to 2.0mm standard plates in treatment of mandibular fractures. J Oral Maxillofac Surg. 2004,62:1392-5.
- Ellis E, Graham J. Use of a 2.0-mm locking plate/screw system for mandibular fracture surgery. J Oral Maxillofac Surg. 2002;60:642-5.
- Kuriakose MA, Fardy M, Sirikunera M et al. A comparative review of 266 mandibular fractures with internal fixation using rigid (AO/ASIF) plates or miniplates. Br J Oral Maxillofac surg. 1996;34:315-332.
- Dechow PC, Ellis E, Throckmorton GS. Structural properties of mandibular bone following application of a bone plate. J Oral Maxillofac Surg. 1995;53:1044-1051.
- Renton TF, Wiesenfeld D. Mandibular fracture osteosynthesis: A comparison of three techniques. Br J Oral Maxiilofac Surg. 1996;34:166-173.
- Cornelius CP, Audigé L, Kunz C, et al. The Comprehensive AOCMF Classification System: Mandible Fractures- Level 2 Tutorial. Craniomaxillofac Trauma Reconstr. 2014;7(Suppl 1):S015-S30.
- Sikes JW, Smith BR, Mukherjee DP et al. Comparison of fixation strengths of locking head and conventional screws, in fracture and reconstruction models. J Oral Maxillofac Surg. 1998;56:468-473.
- Ellis E, Muniz O, Anand K. Treatment considerations for comminuted mandibular fractures. J Oral Maxillofac Surg. 2003; 61:861-870.
- Farmand M. Three-dimensional plate fixation of fractures and osteotomies. Facial Plast Surg Clin North Am.1995;3(1):39–56.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref