Research Article - Current Pediatric Research (2021) Volume 25, Issue 12
Cognitive and ADHD disorders in benign epilepsy with Centrotemporal spikes: An Egyptian study
Khalaf Abdelaal Sayed*, Gamal Ali Abdelal, Nafisa Hassan Refat, Eman Fathala Gad
Department of Pediatrics, College of Medicine, Assiut University, Assiut, Egypt
- Corresponding Author:
- Khalaf Abdelaal Sayed
Department of Pediatrics
Faculty of Medicine
Assiut University
Egypt
E-mail: khalaf13013@gmail.com
Accepted date: 24th December, 2021
Abstract
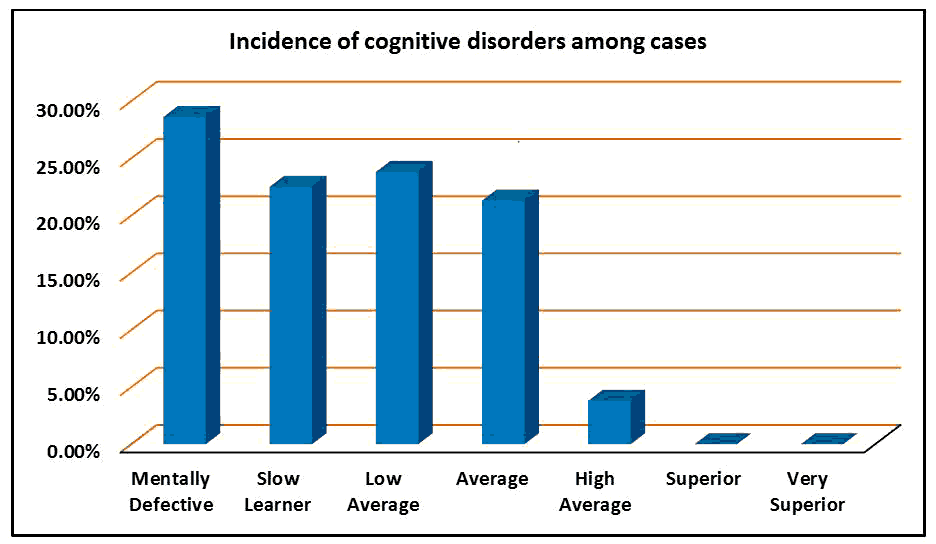
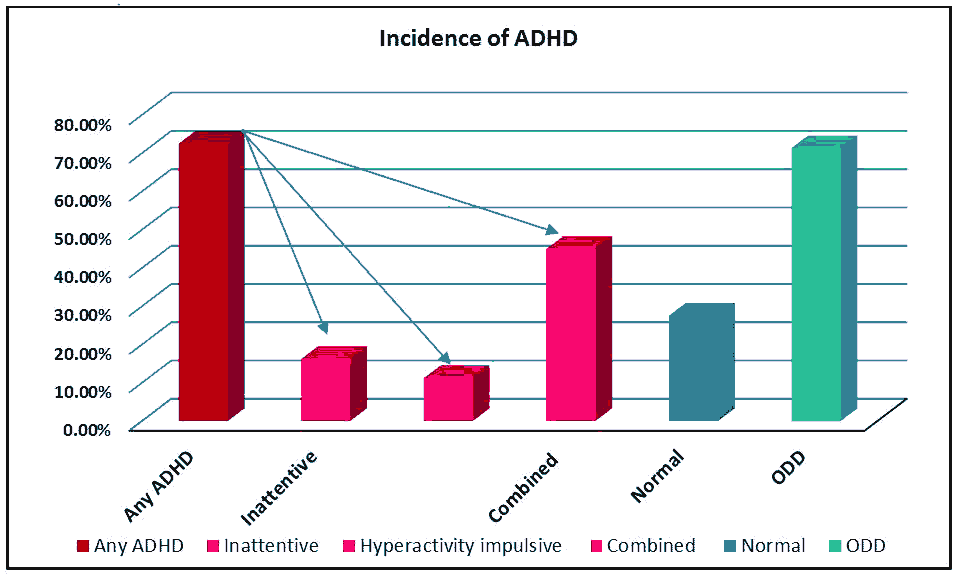
Background: Benign epilepsy with centrotemporal spikes is the most common type of focal epilepsy in children as it accounts for 15% to 25% of epilepsy in children. It is associated with neuropsychological problems which are suspected to be related to spike-wave index, the site of epileptiform discharge, age at onset, and seizures frequency. Therefore, we aimed to study the incidence of the problems associated with BECTS as ADHD, and cognitive disorders and to detect their relation to seizure criteria. Methods: At Assiut University Children Hospital from August 2018 to December 2020, 80 children, ages 3-14 years, were identified to have BECTS. Full history was taken. A complete examination, prolonged sleep EEG, ADHD-SC4 test, IQ assessment were done for all patients. Results: Mentally retarded was detected in 28.6 % of BECTS patients. Cognitive disorders are more common in BECTS patients with more frequent seizures, mixed diurnal, and nocturnal seizures, and higher SWI (P-value < 0.001). We did not find a relationship between cognitive disorder and the age at onset of seizures, sex, or laterality of epileptic focus in EEG. ADHD was detected in 72.5% of BECTS patients. The inattentive type was present in 16.25% of patients, the hyperactivity impulsive type in 11.25%, combined ADHD in 45%. Conclusions: Mentally retarded was detected in 28.6 % of BECTS patients, ADHD was detected in 72.5% of BECTS patients. The inattentive type was present in 16.25% of patients, the hyperactivity impulsive type in 11.25%, combined ADHD in 45%.
Keywords
Benign epilepsy with centrotemporal spikes, ADHD, Cognitive disorder, Spike-wave index.
Introduction
Benign Epilepsy with Centro Temporal Spikes (BECTS) is the most common type of focal epilepsy in children as it accounts for 15% to 25% of epilepsy in children. The age of onset ranges from one to 14 years [1]. BECTS in general is characterized by infrequent focal seizures in the face during sleep, which may secondarily generalize, resulting from excitability from Rolandic regions without any organic brain lesion. The prognosis is usually considered to be excellent but neuropsychological deficits, such as cognitive and behavioral impairments were noted to be common problems in BECTS children [2,3]. These problems are suspected to be related to the sleep-wake cycle and Spike-Wave Index (SWI), the site of epileptiform discharge, age at onset, frequency of seizures, and duration of disease [4]. Also, the SWI is closely related to the atypical evolution of BECTS as Landau-Kleffner Syndrome (LKS), and epileptic encephalopathy with Continuous Spike-And-Wave during Sleep (CSWS), which are thought to be a single spectrum of disorders [5]. The evolution of BECTS to CSWS occurs when SWI exceeds 25% to 85% with a controversy between different studies [6].
Cognitive disorders, ADHD, and learning disorders are more common in epileptic children, and about 50% of them need specific education programs [7]. Several factors contribute to neuropsychiatric impairments in these children including interactions between seizures, anti-seizure drugs, underlying causes of epilepsy, and the innate properties of epilepsy [8]. Cognitive affection in children newly diagnosed to have epilepsy before the first seizure suggests the presence of common biological mechanisms. Also, the relationship between ADHD and epilepsy is thought to be bidirectional [9].
The prevalence of cognitive deficits in children with BECTS is reported as 21.8% [10] compared to the prevalence of intellectual disability in the general population is 1% to 3% [11]. In a systematic review, Aricò et al. found the prevalence of ADHD in patients with BECTS was about 60% [12]. Cognitive and behavioral problems are important issues in children with BECTS because they are at a critical phase of neurodevelopment, education, and acquiring skills [13]. Therefore, we aimed to study the incidence of the problems associated with BECTS as ADHD, learning, and cognitive disorders, and to detect their relation to seizure criteria.
Materials and Methods
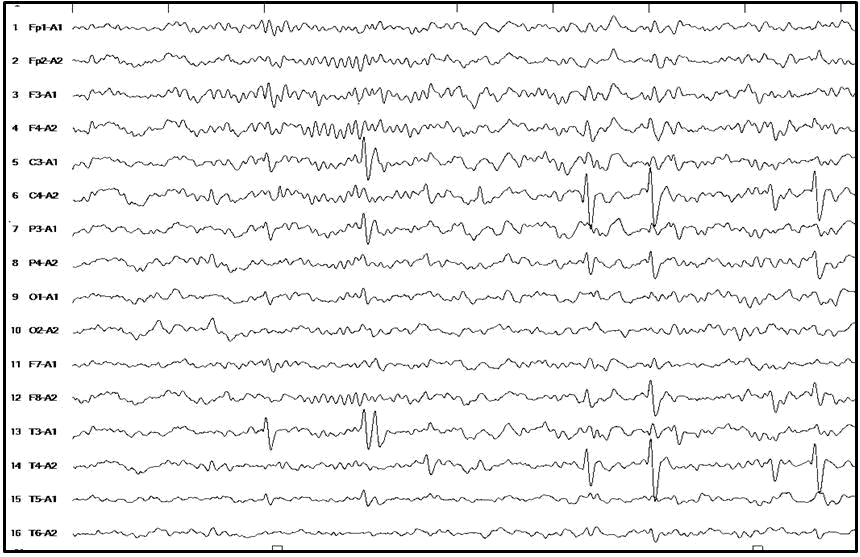
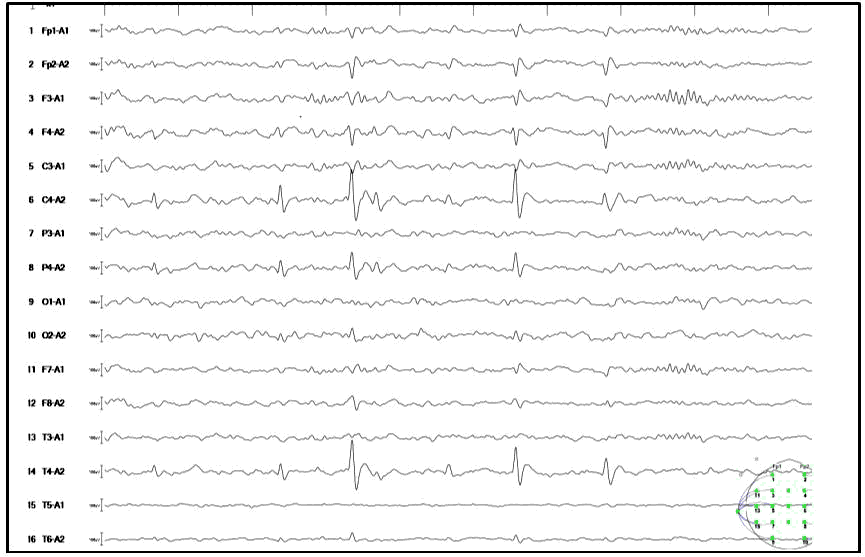
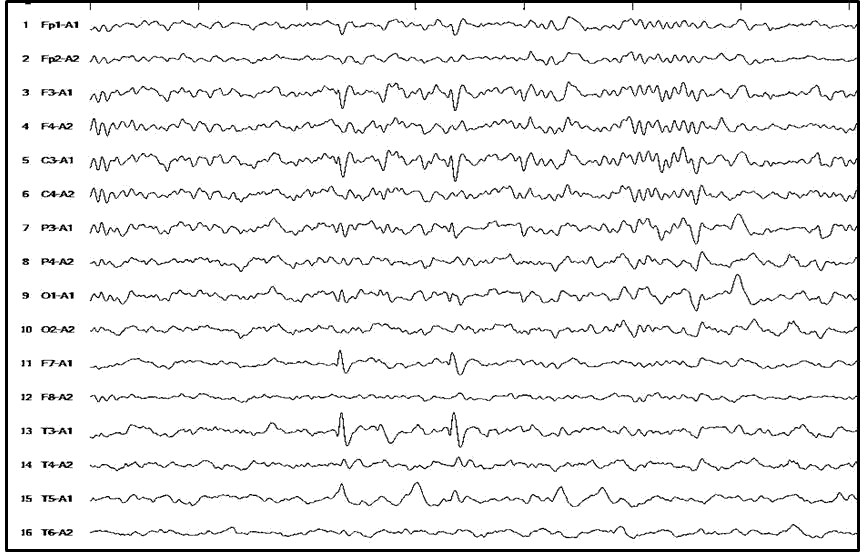
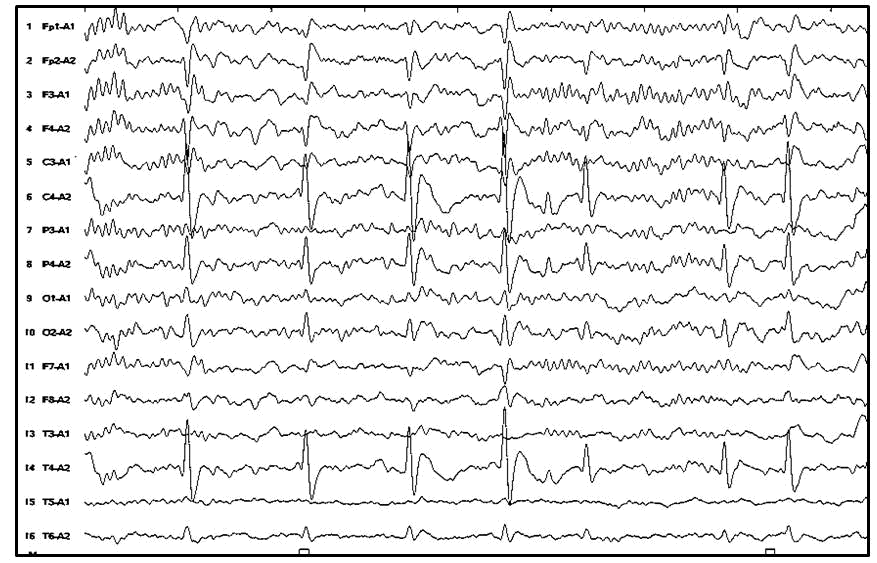
At Assiut university children hospital from August 2018 to December 2020, 80 children, ages 3-14 years, were identified to have BECTS from history and EEG findings. Children with genetic disorders, metabolic or neurodegenerative disease, and motor deficit were excluded. Full history including name, age, sex, age of seizure onset, the type of convulsions and their relation to sleep, developmental history, behavioral problems, and school performance was taken. The EEG was done during sleep, and we looked at the full sleep recording and visually picked the epoch with the highest spike density. The counting started with a page of high spikes and continued for 10 consecutive minutes. The site and laterality of epileptic spikes were detected and the SWI was calculated for every patient. ADHD assessment with ADHD-SC4 test and IQ assessment with Stanford-Binet scales, version IV was done. Written consent was obtained from every parent whose children were included in the study. Obtaining approval from the ethical committee of the faculty of medicine at Assiut University.
Statistical analysis
The collected data were analyzed using the Statistical Package for Social Sciences (SPSS) release 22.0 program (SPSS for Windows; SPSS Inc, Chicago, IL). Numerical data were expressed as mean ± standard deviation and compared using independent student's t-test. Categorical data were reported in frequencies and percentages and compared with the chi-square test when appropriate. Statistical significance was accepted at P-value less than 0.05
Results
The study included 80 children (47 males, 33 females) with benign epilepsy with centrotemporal spikes attended to Assiut university children hospital during the period from August 2018 through December 2020. The median age at the time of diagnosis was 7.9 years with a range of 3-14 years old (Figures 1 to 7).
Discussion
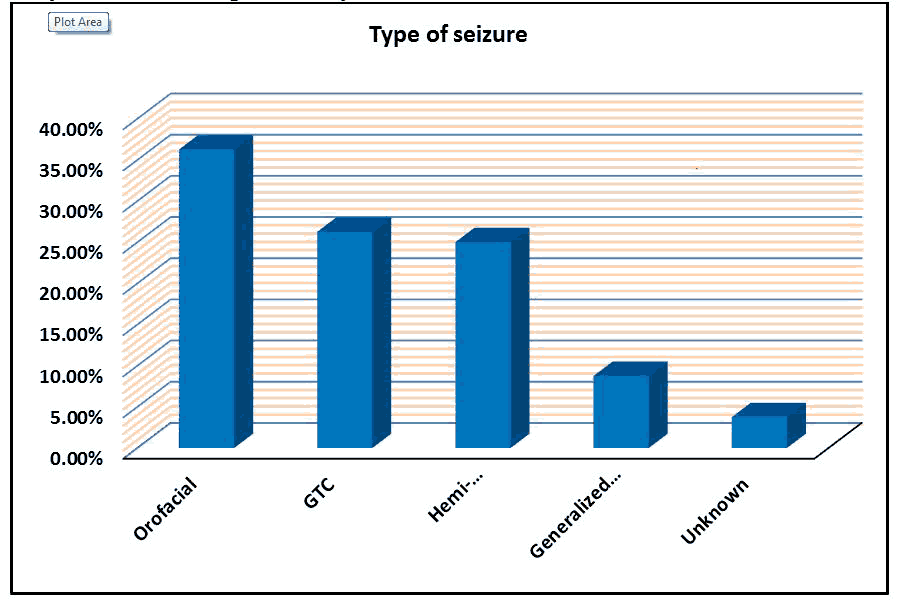
The study included 80 children (47 males, 33 females) with benign epilepsy with centrotemporal spikes attended to Assiut university children hospital during the period from August 2018 through December 2020. The median age at the time of diagnosis was 7.9 years with a range of 3-14 years old. Seizures were nocturnal in 86.3% of cases, nocturnal and diurnal in 13.7% of cases. The mean number of seizures was 1.71 ranging from one to 7 attacks. The type of seizures was or facial in 36.25% of patients, generalized tonic-colonic in 26.25%, hemi convulsions in 25%, generalized tonic in 8.75%, and unknown in 3.75%. The occurrence of generalized convulsions is overestimated because most of them occur at night and the onset is seen [14]. This may explain the high percentage of generalized tonic-colonic convulsions and hemi convulsions in our study.
Interictal Epileptic Discharges (IEDs) were unilateral in 50% (left in 28.7% and right in 21.3%) and bilateral in 50%. The spike site is unilateral in 60% and sometimes changes from one side to the other over time or maybe in both sides in 40% in BECTS [15]. Berroya et al. [16] studied the laterality of IEDs of BECTS in wakefulness, drowsiness, and sleep. They reported unilateral IEDs in 74.5% (45.4% right and 29.1% left) and bilateral IEDs in 25.5% in wakefulness. During drowsiness unilateral IEDs were in 62.2% (35.5% right and 26.7% left) and bilateral IEDs in 37.8%. During sleep unilateral IEDs were in 51.5% (30% right and 21.5% left) and bilateral IEDs in 48.5%. During the transition from wakefulness to sleep, the IEDs become more abundant and more bilateral.
In the present study, SWI was calculated for every patient from a prolonged sleep EEG. The SWI was <25% in 55% of patients, >25% to 50% in 25% of patients, >50% to 85% in 17.5% of patients, and >85% in 2.5% of patients. CSWS was first described by Patry et al. [17] as a subclinical “electrical status epilepticus” induced by sleep in children. The term “continuous spikes and waves during slow sleep” is synonymous with electrical status Epilepticus in Slow-Wave Sleep (ESES) [18]. In our study, 20% of patients with BECTS had ESES (SWI>50%). Tovia et al. [10] reported 4.6% of patients with BECTS to have ESES and Ross et al. [4] reported 6.6% meet the criteria for either LKS or CSWS. On the other hand, Berroya et al. [16] reported 51.5% of patients with BECTS to have ESES (SWI>50%). Kessi et al. [19] surprisingly reported a higher prevalence of ESES among patients with BECTS. They detect 10.3% of 185 patients having SWI>85% and 49.7% of 185 patients having SWI>50%.
Mentally retarded was detected in 28.6%, slow learner in 22.5%, low average in 23.8%, average in 21.3%, high average in 3.8%, and no detected superior or very superior IQ. Our findings also support previously published articles that claimed that BECTS is not benign in terms of cognitive deficits [3,10]. Up to 28.6% of the patients in our cohort were diagnosed as having mental retardation. Tovia et al. [10] reported 21.8% of BECTS patients to have cognitive deficits and similar to the findings of Yung et al. [20]. The prevalence of intellectual disability in the general population is about 1% to 3% in western countries and it is 1.5 times more common among males than females with the highest prevalence occurring between the ages of 6 and 16 years [11].
The percentage of our BECTS patients with ADHD in our study was 72.5%. This is similar to the study of Kim et al. [21] which detected 64.9% of the 74 children with BECTS had ADHD, and Danhofer et al. [22] detected 65.6% compared to the rate of 31% reported by Tovia et al. [10], and 11% reported by Datta et al. [23]. In a systematic review, Aricò et al. [12] found the reported prevalence of ADHD in patients with BECTS was around 60%.
The inattentive type was present in 16.25% of patients, the hyperactivity impulsive type in 11.25%, and combined ADHD in 45%. ADHD increased by 42% from 2003 to 2011 in the USA. In 2003, 7.8% of children were diagnosed with ADHD, in 2007, they were 9.5%, and in 2011, they were 11% [24]. The prevalence of ADHD in Fayooum City, Egypt, was 20.5% [25]. The annually increasing prevalence of ADHD, the more common in males, the difference according to age groups, and using different diagnostic tools may partially explain the higher prevalence of ADHD in our study. Also, it can be explained by the higher Spike-Wave Index in our study (SWI>50% in 20% of patients).
These neuropsychological deficits are suspected to be related to the sleep-wake cycle and SWI, the localization of epileptiform discharge, age at onset, frequency of seizures, and duration of disease though these relationships are not always detected [4,26,27]. In our study cognitive disorders are more common in BECTS patients with more frequent seizures (P-value=0.017), mixed diurnal and nocturnal seizures than only nocturnal seizures (P-value=0.005), and higher SWI (P-value<0.001). We did not find a relationship between cognitive disorder and the age at onset of seizures, sex, or laterality of epileptic focus in EEG. This finding provides support for a common mechanism underlying both the neuropsychiatric deficits and epilepsy in this disorder. The lack of effect of the laterality of the electrical focus on cognitive ability in our patients is in agreement with the study of Goldberg-Stern et al. Also, several studies have not found seizure focus lateralization effect on cognitive processes [28]. This may be because both hemispheres contribute to language and cognitive function early in life with an increase in left lateralization of language with advancing age [29]. Also, epileptic focus can travel from one hemisphere to the other in BECTS patients [15]. Some studies show more cognitive impairment in BECTS patients with left-sided focus [30], right-sided focus [31], and other studies in bilateral BECTS [32].
We found a relationship between inattentive ADHD and certain seizure criteria. Inattentive ADHD is more common in BECTS patients with more frequent seizures (P-value=0.024), male patients (P-value=0.042), and SWI (P-value=0.021). We did not find a relationship between inattentive ADHD and the age at onset of seizures, time of seizures, or laterality of epileptic focus in EEG. Also, hyperactive-impulsive ADHD is more common in BECTS patients with more frequent seizures (P-value=0.041), and SWI (P-value=0.033). We did not find a relationship between hyperactive-impulsive ADHD and the age at onset of seizures, sex, time of seizures, or laterality of epileptic focus in EEG. Different studies found a relation between ADHD and age at seizure onset [33], the SWI [21], or the site of epileptic focus [32]. The pathophysiology of ADHD in children with BECTS is unknown but it may be due to common genetic or biochemical factors [34,35]. Also, it may be due to poor maturation of the brain as a result of suppression of the same cortical region by frequent spikes [21].
Conclusion
BECTS is commonly associated with neuropsychological deficits. Mentally retarded was detected in 28.6% of BECTS patients, ADHD was detected in 72.5% of BECTS patients. The inattentive type was present in 16.25% of patients, the hyperactivity impulsive type in 11.25%, combined ADHD in 45%.
Acknowledgments/Source of Funding
No funding
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- Uliel-Sibony S, Kramer U. Benign Childhood Epilepsy With Centro-Temporal Spikes (BCECTSs), Electrical Status Epilepticus In Sleep (ESES), and academic decline. How aggressive should we be? Epilepsy Behav 2015; 44(5): 117-20.
- Ay Y, Gokben S, Serdaroglu G, et al. Neuropsychologic Impairment in children with Rolandic epilepsy. Pediatr Neurol 2009; 8(6): 94-7.
- Danielsson J, Petermann F. Cognitive deficits in children with benign Rolandic epilepsy of childhood or Rolandic discharges: A study of children between 4 and 7 years of age with and without seizures compared with healthy controls. Epilepsy Behav 2009; 16(4): 646-51.
- Ross EE, Stoyell SM, Kramer MA, et al. The natural history of seizures and neuropsychiatric symptoms in Childhood Epilepsy with Centro Temporal Spikes (CECTS). Epilepsy Behav 2020; 103(11):106437-440.
- Fejerman N. Atypical rolandic epilepsy. Epilepsia 2009; 50(4): 9-12.
- Loddenkemper S, Cosmo G, Kotagal P, et al. Epilepsy surgery in children with electrical status epilepticus in sleep. Neurosurgery 2009; 64(2): 328-37.
- Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics 2012; 7(1): 76-83.
- You SJ. Cognitive function of idiopathic childhood epilepsy. Korean J Pediatr 2012; 55(5): 159-65.
- Chou IC, Chang YT, Chin ZN, et al. Correlation between epilepsy and attention deficit hyperactivity disorder: A population-based cohort study. PLoS One 2013; 5(2): 87-9.
- Tovia E, Goldberg-Stern H, Ben Zeev B, et al. The prevalence of atypical presentations and comorbidities of benign childhood epilepsy with centrotemporal spikes. Epilepsia 2011; 52(8): 1483-8.
- Bisconer S, Ahsan S. Intellectual disability. In the curated reference collection in neuroscience and bio-behavioral psychology. Elsevier Science Ltd 2016; 8(3): 86-7.
- Aricò M, Arigliani E, Funck-Brentano C, et al. ADHD and ADHD-related neural networks in benign epilepsy with centro temporal spikes: A systematic review. Epilepsy Behav 2020; 112(3): 51-9.
- Kang S-H, Yum M-S, Kim E-H, et al. Cognitive function in childhood epilepsy: Importance of attention deficit hyperactivity disorder. J Clin Neurol 2015; 11(1): 20-5.
- Loiseau P, Beaussart M. The seizures of benign childhood epilepsy with Rolandic paroxysmal discharges. Epilepsia 1973; 14(4): 381-9.
- Dryżałowski P, Jóźwiak S, Franckiewicz M, et al. Benign epilepsy with centro temporal spikes–Current concepts of diagnosis and treatment. Polish JNeurolNeurosurg 2018;52(6):677-89.
- Berroya AM, Bleasel AF, Stevermuer TL, et al. Spike morphology, location, and frequency in benign epilepsy with centro temporal spikes. JChild Neurol 2005; 20(3): 188-94.
- Patry G, Lyagoubi S, Tassinari CA. Subclinical electrical status epilepticus induced by sleep in children: A clinical and electroencephalographic study of six cases. ArchNeurol 1971; 24(3): 242-52.
- Engel J. A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: Report of the ILAE task force on classification and terminology. Epilepsia 2001; 42(6): 796-803.
- Kessi M, Yan F, Pan L, et al. Treatment for the benign childhood epilepsy with centrotemporal spikes: A monocentric study. FrontNeurol 2021; 12(5): 670958-.
- Yung AWY, Park YD, Cohen MJ, et al. Cognitive and behavioral problems in children with centrotemporal spikes. Pediatr Neurol 2000; 23(5): 391-5.
- Kim EH, Yum MS, Kim HW, et al. Attention-deficit/hyperactivity disorder and attention impairment in children with benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav 2014; 37(8): 54-8.
- Danhofer P, Pejčochová J, Dušek L, et al. The influence of EEG-detected nocturnal centrotemporal discharges on the expression of core symptoms of ADHD in children with Benign Childhood Epilepsy with Centrotemporal Spikes (BCECTS): A prospective study in a tertiary referral center. Epilepsy Behav 2018; 79(5): 75-81.
- Datta A, Sinclair DB. Benign epilepsy of childhood with Rolandic spikes: Typical and atypical variants. Pediatr Neurol 2007; 36(3): 141-5.
- Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry 2014; 53(1): 14-23.
- Aboul-ata MA, Amin FA. The Prevalence of ADHD in Fayoum City (Egypt) among school-age children: Depending on a DSM-5-based rating scale. J Atten Disord 2018; 22(2): 127-33.
- Goldberg-Stern H, Gonen OM, Sadeh M, et al. Neuropsychological aspects of benign childhood epilepsy with centrotemporal spikes. Seizure 2010; 19(1): 12-6.
- Callenbach PMC, Bouma PAD, Geerts AT, et al. Long term outcome of benign childhood epilepsy with centrotemporal spikes: Dutch study of epilepsy in childhood. Seizure 2010; 19(8): 501-6.
- Northcott E, Connolly AM, Berroya A, et al. The neuropsychological and language profile of children with benign Rolandic epilepsy. Epilepsia 2005; 46(6): 924-30.
- Kadis DS, Pang EW, Mills T, et al. Characterizing the normal developmental trajectory of expressive language lateralization using magneto encephalography. J Int Neuropsychol Soc 2011; 17(5): 896-904.
- Monjauze C, Broadbent H, Boyd SG, et al. Language deficits and altered hemispheric lateralization in young people in remission from BECTS. Epilepsia 2011; 52(8): e79-e83.
- Pinton F, Ducot B, Motte J, et al. Cognitive functions in children with Benign Childhood Epilepsy with Centrotemporal Spikes (BECTS). Epileptic Disord 2006; 8(1): 11-23.
- Bedoin N, Ciumas C, Lopez C, et al. Disengagement and inhibition of visual-spatial attention are differently impaired in children with rolandic epilepsy and Panayiotopoulos syndrome. Epilepsy Behav 2012; 25(1): 81-91.
- Klenberg L, Korkman M, Lahti-Nuuttila P. Differential development of attention and executive functions in 3-12 year old finish children. Dev Neuropsycho 2001; 20(1): 407-28.
- Parisi P, Moavero R, Verrotti A, et al. Attention deficit hyperactivity disorder in children with epilepsy. Brain and Development 2010; 32(1): 10-6.
- Sharaf MA, Hashem HE, Ahmed WO. Simultaneous use of factor xiii and fibrin degradation products in diagnosing early cases of nec and neonatal SEPSIS. Journal of Scientific Research in Medical and Biological Sciences 2021; 2(4): 1-10.