Case Report - Journal of Gastroenterology and Digestive Diseases (2022) Volume 7, Issue 4
Clostridioides difficile infection presenting as an ileus.
Bhangale Nikhil*Department of Gastroenterology, P D Hinduja Hospital and MRC, Mumbai, Maharashtra, India
- *Corresponding Author:
- Bhangale Nikhil
Department of Gastroenterology
P D Hinduja Hospital and MRC
Mumbai, Maharashtra, India
E-mail: nikhilb.ebox@gmail.com
Received: 13-Dec-2021, Manuscript No. JGDD-22-117; Editor assigned: 15-Dec-2021, PreQC No. JGDD-22-117 (PQ); Reviewed: 03-Jan-2022, QC No. JGDD-22-112; Revised: 08-Apr-2022, Manuscript No. JGDD-22-112 (R); Published: 14-Apr-2022, DOI: 10.35841/jgdd-7.4.117
Citation: Nikhil B. Clostridioides difficile infection presenting as an ileus. J Gastroenterology Dig Dis. 2022;7(4):117
Abstract
Clostridioides difficile (previously, Clostridium difficile) is a frequent cause of hospital-acquired diarrhoea and has shown a rising trend in community-acquired infections as well, with widespread use of antibiotics, among other risk factors. The disease has significant morbidity; a fulminant course may result in death. Rarely, the disease may present with only ileus, with delayed diagnosis, leading to toxic megacolon, colonic perforation and high fatality rates. We report two such patients who improved following specific treatment, leading to full recovery.
Keywords
Clostridioides difficile, Diarrhoea, Nosocomial diarrhoea.
Case Presentation
Clostridioides difficile (previously, Clostridium difficile) is a frequent cause of nosocomial diarrhoea leading to complications that prolong hospital stay as well as increase mortality rate. The widespread use of antibiotics has led to community outbreaks as well [1]. Community carriage rates range from 0-3% whereas the rate in hospital inpatients is as high as 10-20%. Indian studies have found prevalence ranging from 7% to 25% amongst patients with diarrhoea. In most cases the illness presents as watery diarrhoea and is best managed by holding incriminated or offending antibiotics and giving Vancomycin orally. However, occasionally the disease may present without diarrhoea as ileus/pseudo-obstruction, which may lead to delay in diagnosis and lower survival.
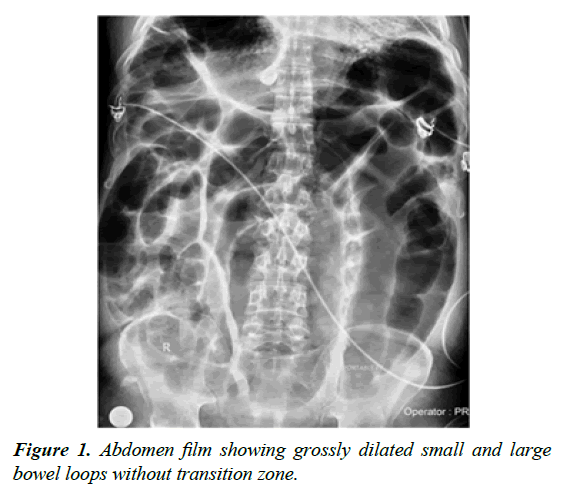
We report two such patients in whom the diagnosis led to rapid response and complete recovery. A 53-year-old gentleman presented with anorexia, early satiety and constipation followed by progressive generalised abdominal distension. He had undergone haemorrhoidectomy 2 weeks ago for per-rectal bleeding, but continued to have drops of blood per rectum. He had interstitial lung disease and was on pirfenidone for 3 years, with a course of corticosteroids 1 month back for worsening dyspnoea; he had recently received a course of co-amoxiclav for cough [2]. On examination, he was afebrile and blood pressure was normal; there was tachycardia (120/min) and desaturation room air. Abdomen was distended and tympanic with feeble bowel sounds; rectal examination revealed faecal loading. Routine labs showed only neutrophilic leucocytosis. Abdominal film showed grossly dilated small and large bowel loops without transition zone (Figure 1). CT scan of abdomen showed dilatation of transverse and sigmoid colon and rectum with faecal loading of right colon and mild wall thickening of left colon with surrounding fat stranding. With a diagnosis of sepsis-induced ileus, supportive management and IV antibiotics including third-generation cephalosporins were initiated in the ICU [3].
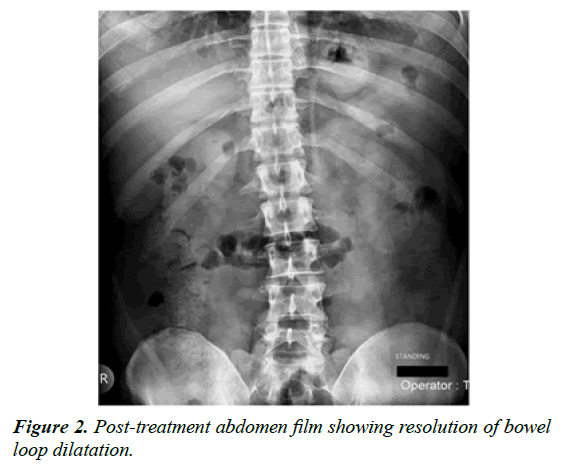
The patient developed an episode of fresh bleeding per rectum and hence flexible sigmoidoscopy was done, this revealed multiple discrete ulcerations with overlying pseudomembranes and surrounding erythema, with normal intervening mucosa. Stool tested positive for C. difficile toxin A and B. The patient was started on oral vancomycin for 10 days and IV metronidazole was co-administered (Figure 2). He improved on the third day and made full recovery with normal X-ray on day 8 of treatment [4].
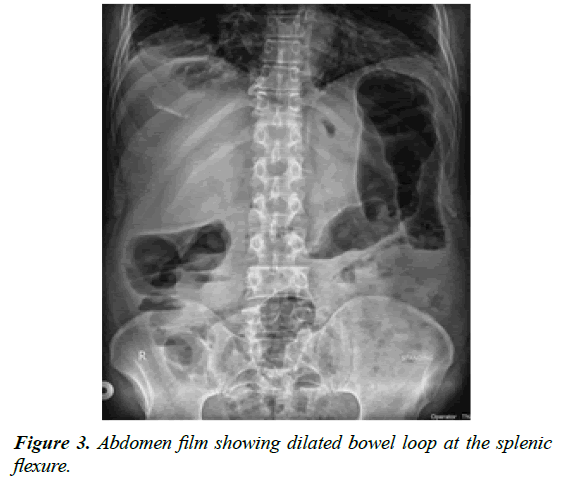
A 64-year-old gentleman presented with painless progressive abdominal distension and constipation for 10 days, without vomiting or fever. He had undergone fistulotomy for perianal fistula 15 days ago. He had been on treatment for hypertension for 10 years. Examination revealed normal vital signs and distended tympanic abdomen. Per-rectal exam showed faecal loading in rectum without blood staining. Abdomen film showed dilatation at the splenic flexure (Figure 3).
Routine labs were normal. CT abdomen showed diffuse colonic wall thickening with surrounding fat stranding. Colonoscopy was planned, but meanwhile the patient passed small amounts of mucoid stools that tested positive for C. difficile toxin A and B. He was started on oral vancomycin for 10 days. His condition improved from day 5 and he recovered completely with resolution of colonic dilatation on X-ray. Colonoscopy 2 months later was unremarkable. Both patients were discharged to home after resolution of symptoms and radiologic findings. Both were asymptomatic 3 months after the illness [5].
Discussion and Conclusion
The mechanism of ileus in C. difficile infection has been linked to the in-vitro inhibitory effect of C. difficile toxin B on intestinal smooth muscle activity. Ileus as an isolated manifestation of C. difficile infection has been reported only as case reports. All these reported patients were in-hospital and had significant co-morbidities when they acquired the infection; our patients had history of surgery 2 weeks earlier, had comorbidities, and one of them had received antibiotics recently. Both our patients recovered completely on specific treatment. The presentation of the disease as ileus is often associated with higher mortality rate secondary to the development of toxic megacolon and perforation. These cases highlight the need for early diagnosis to improve outcome.
References
- Mylonakis E, Ryan ET, Calderwood SB. Clostridium difficile-associated diarrhea: A review. Arch Intern Med. 2001;161:525-33.
- Ingle M, Deshmukh A, Desai D, et al. Prevalence and clinical course of Clostridium difficile infection in a tertiary-care hospital: A retrospective analysis. In J Gastroenterol. 2011;30:89-93.
- McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):41-8.
- Gilbert RJ, Triadafilopoulos G, Pothoulakis C, et al. Effect of purified Clostridium difficile toxins on intestinal smooth muscle. I. Toxin A. Am J Physiol Liver Physiol. 1989;256:759-66.
- Elinav E, Planer D, Gatt ME. Prolonged ileus as a sole manifestation of pseudomembranous enterocolitis. Int J Colorectal Dis. 2004;19:273-276.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref