Research Article - Biomedical Research (2016) Volume 27, Issue 4
Clinical research on loss of resistance technique in fascia iliaca compartment block
Liang-Jing Yuan, Jun Yi, Li Xu and Qing-Guo Yang*Department of Anesthesia, Beijing Jishuitan Hospital, Beijing 100035, PR China
Accepted date: March 26, 2016
Abstract
This study aims to investigate the positioning accuracy and effectiveness of the loss of resistance technique (LOR) in fascia iliaca compartment block (FICB). A total of 175 patients prepared for hip surgery were enrolled; the injection needle was inserted at the centrolateral one-third point of the junction of the anterosuperior iliac spine and external pubic angle, 2 cm parallel to the tail end; after sensing a feeling of "breaking through" twice, 30 mL 0.5% ropivacaine was injected, and its spread was assessed by ultrasound-guidance. The patients were divided into three groups according to needling positions: group A: accurate, group B: too shallow (above the fascia iliac), and group C: too deep (inside the iliopsoas). The sensation blocks of the femoral, lateral femoral cutaneous, and obturator nerves were recorded 20 min after the injection. As observed under ultrasound, the positioning accuracy rate of LOR inside the FIC was 56.6%. The success rate of FICB using LOR was 91.4% 20 min later, and the complete block rate was 68.0%. The successful and complete block rates in group A were significantly higher than those in groups B and C (P < 0.001). The key for successful and complete FICB was accurate injection of the medicine into the FIC, but traditional LOR showed unsatisfactory accuracy when positioning within the FIC.
Keywords
Fascia iliaca compartment, Loss of resistance technique, Ultrasound technique.
Introduction
Fascia iliaca compartment block (FICB) can effectively block the femoral, lateral femoral cutaneous, and obturator nerves. Single or continuous FICB could improve postoperative analgesia in patients, reduce postoperative morphine use [1,2], and be used as preoperative analgesia for patients with fractures [3]. Because its needling point is far away from the femoral nerve and blood vessels compared to the traditional "3- in-1" method, the FICB procedure is simple, safe, and effective [4,5]. The most commonly used method for FICB is the loss of resistance technique (LOR), but its success rate varies widely from up to 96% [6] to only 67% [7]. However, to our knowledge, no studies have clearly confirmed the success rate and efficiency of the LOR technique in clinical anesthesia, and there are currently no effective evaluation criteria. In recent years, the ultrasound-guided peripheral nerve block technique has been applied in clinical anesthesia, which allows visualization of the blood vessels, nerves, surrounding tissues, as well as the ability to visualize the spread of medicine [8]. Ultrasound-guided peripheral nerve block also allows direct observation of each anatomical structure and monitoring of the blocking process in real-time [9]. Ultrasound-guidance has proven to be a valuable method for peripheral nerve block positioning and is currently used in clinical anesthesia [8]. The current study assessed the accuracy and evaluated the clinical effects of ultrasound-guided LOR in FICB.
Materials and Methods
General data
Patients aged 20-80 years old with American Society of Anesthesiology (ASA) classifications I-III who were prepared for hip surgery were enrolled in the study. The exclusion criteria included: 1) operation contraindications such as infection at the puncture site, anatomic variations, coagulation abnormalities, or unsuitable posture; 2) previous history of long-term administration of non-steroidal anti-inflammatory analgesics, or addiction to opioids; 3) neurological limb abnormalities.
Ultrasound-guided LOR in FICB
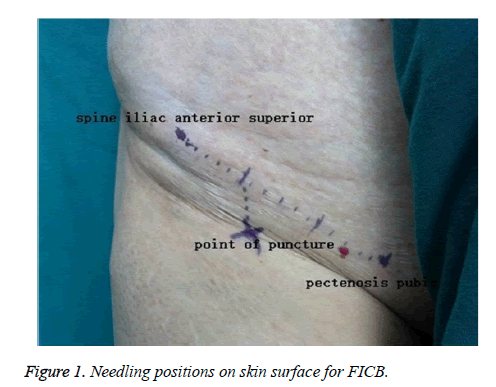
Each patient underwent routine monitoring after entering the operation room, and the sense of temperature was tested at the anterior zone of 1/3 lower limb thigh, two-thirds of the way above the median knee joint and the lateral zone of thigh to ensure consistency in both lower extremities. Each patient was then placed in a supine position; a line was drawn between the anterosuperior iliac spine and the external pubic angle, which was then equally divided into three segments, and the point at the centrolateral one-third junction and 2 cm parallel to the tail end was selected as the needling point (Figure 1).
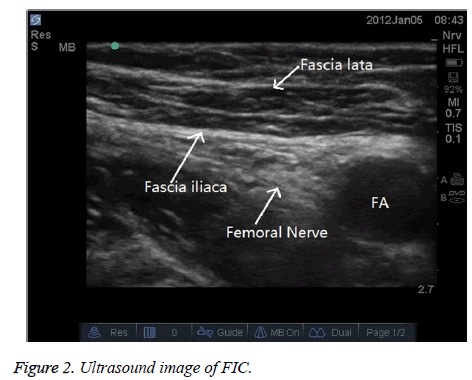
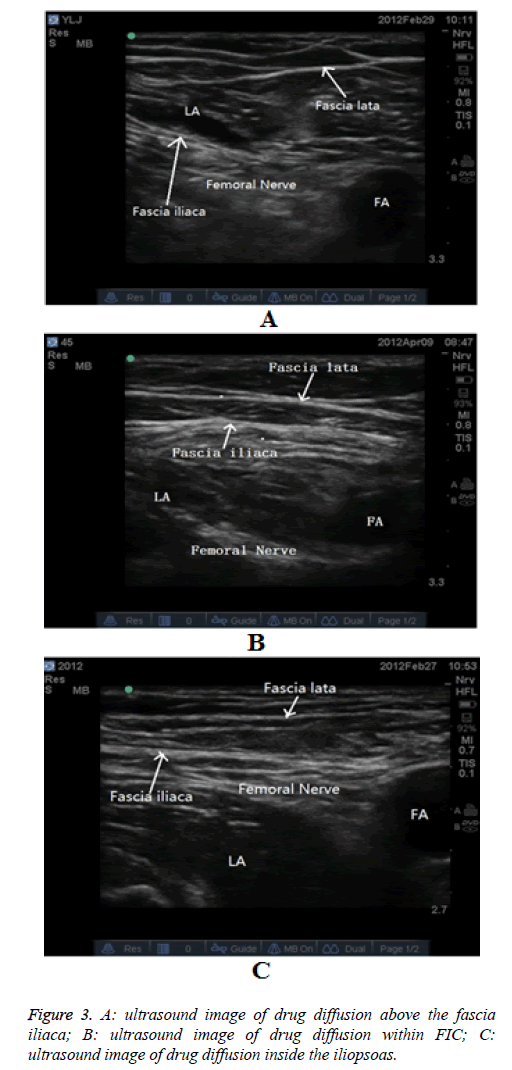
After puncturing skin, a needle with 50-mm short bevel (Plexufix® 50 mm, 24G. B.Braun Co., Germany) was placed at a 60° angle with the skin and used to pierce the skin; the needle was withdrawn after the anesthetists felt the needle "breaking through" twice, and fixed when no blood appeared. A nerve-block ultrasound-guided (M-Turble, SonoSite, USA) was then performed, placing the probe (HFL 38 × /13-6 MHz, SonoSite, USA) along and below the inguinal ligament to observe the puncture needle; the ultrasound images were adjusted to clearly identify the femoral artery, femoral nerve, and fascia iliaca (Figure 2). Next, 30 mL of 0.5% ropivacaine (batch number: IL1619, AstraZeneca AB, Sweden) was then administrated via the needle. The drug diffusion site was observed (above the fascia iliaca, within the FIC, and inside the iliopsoas, Figures 3A-3C), and diffusion in the FIC was defined as observable diffusion of the drug below the fascia iliaca and surrounding the femoral nerve (Figure 3B). The depth of the needle was measured, and the degree of block was evaluated 20 min later by testing the sense of temperature using an alcohol swab on the anterior zone of 1/3 lower limb thigh (femoral nerve-innervated area), two-thirds of the distance above the median knee joint of the thigh (obturator nerve-innervated area), and the lateral zone (lateral femoral cutaneous nerve-innervated area). The results were scored as 0 (feeling normal)=no sensation loss, and 1 (sensation changed)=temperature sense diminished or disappeared. A temperature sensation change (temperature sensation decreased or disappeared) on one or more sights of the thigh was defined as a successful block, while a temperature sensation change on all three sides was defined as a complete block.
Statistical analysis
SPSS version 13.0 was used for statistical analysis. Measurement data were expressed as means ± standard deviations and compared using analysis of variance (ANOVA); counting data were expressed as percentages (%) and compared using χ2 tests, with P<0.05 considered statistically significant.
Results
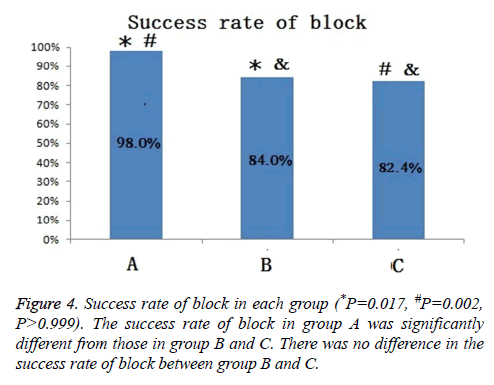
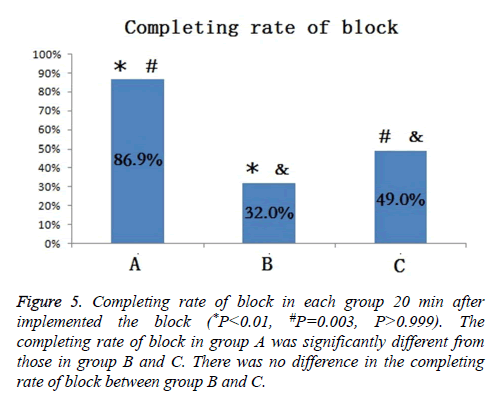
This study included 175 patients (82 men and 93 women), with a mean age, height, and weight of 57.3 ± 15.9 years, 165.2 ± 14.7 cm, and 64.9 ± 11.1 kg, respectively. Groups A, B and C, based on drug diffusion, contained 99 (56.6%), 25 (14.3%), and 51 cases (29.1%), respectively, and there were no statistically significant differences in the general patient conditions among these three groups (Table 1). A total of 160 cases appeared to experience changes in temperature sensation on any side of the thigh 20 min after LOR for FICB, resulting in a successful block rate of 91.4%; furthermore, a total of 119 cases experienced changes in temperature sensation change on all three sides, corresponding to a complete block rate of 68.0%. The success and complete block rates in group A were significantly different from those in groups B and C (Figures 4 and 5).
| Group | Cases | Gender (M/F) | Age (years) | Height (cm) | Weight (kg) |
| A | 99(56.6%) | 50/49 | 58.1 ± 15.3 | 166.6 ± 12.3 | 65.4 ± 10.5 |
| B | 25(14.3%) | 12/13 | 58.3 ± 15.0 | 160.9 ± 20.2 | 66.4 ± 11.8 |
| C | 51(29.1%) | 20/31 | 55.1 ± 17.5 | 164.5 ± 15.7 | 62.0 ± 11.6 |
| Statistics | -- | 1.738 | 0.653 | 1.557 | 1.183 |
| P | -- | 0.419 | 0.522 | 0.214 | 0.309 |
Table 1: General information of the patients in the three groups (͞x ± s).
Discussion
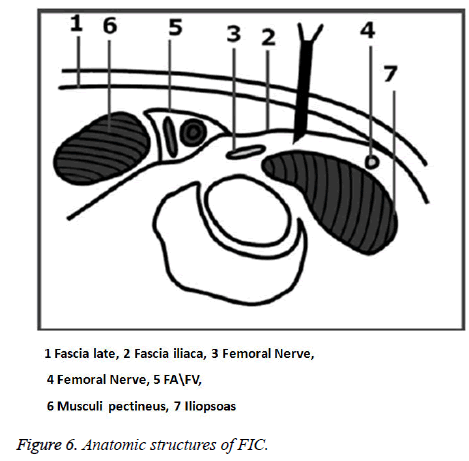
The ultrasound-guided imaging used in this study revealed that the success rate of traditional LOR was only 56.6%. This low success rate was mainly related to the anatomic structures of the FIC. The FIC is a potential cavity with the iliopsoas and fascia iliaca as the posterior and anterior borders, respectively, and the superficial layer of the fascia iliaca is covered by the fascia lata. The femoral, lateral femoral cutaneous, obturator, and reproductive femoral nerves also distract in the FIC to varying degrees. The ventral side of the FIC is covered by the fascia lata and fascia iliaca, such that there is a definite sense of a needle “breaking through” these two layers, namely the feeling of a loss of resistance, beyond which the needle enters the FIC (Figure 6). Several studies have indicated that that FIC is less commonly used in adult patients because the presence of the fascia iliaca and thus clear differentiation of “breaking through” cannot be easily confirmed [10]. Analysis of cadaveric anatomies [11] revealed that human subcutaneous tissue is composed of multiple fascial layers, and LOR might be associated with the needle broke through any of these layers. Thus, it is possible with traditional LOR to mistake other fascia as the fascia iliaca, leading to incorrect FIC positioning as well as injection of the drug outside the FIC (above the FIC or inside the iliopsoas) [12]. Incorrect injection sites would reduce the success rate of regional anesthesia [13].
Traditional LOR emphasizes feeling the "breaking through" sensation twice, indicating successful penetration of the needle through the fascia lata and fascia iliaca. However, mistaking the fascia of the subcutaneous tissue for the fascia iliaca would result in too-shallow needling. Use of short-bevel needles requires extra force to break through the fascia because the needle tip slope is 45°, which may result in too-deep needling after penetrating the fascia. Compared with traditional nerve block methods such as blind detection, nerve stimulator guidance, computed tomography (CT), or magnetic resonance assistance, the advantages of ultrasound-guided peripheral nerve block include the ability to directly "observe" each anatomical structure and simultaneously monitor the block process in real-time. In this study, when the anesthetist felt the sense of "breaking through" twice, one ultrasound probe was placed at the inguinal folds to observe drug diffusion after administration, thus marking the exact location of the needle. The results showed that the drug diffusion was above the fascia iliaca in 25 cases (14.3%), within the FIC 99 in cases (56.6%), and inside the iliopsoas in 51 cases (29.1%). In other words, ultrasound confirmed that the traditional LOR methods only had an accuracy rate of 56.6%; thus, the traditional LOR method had certain limitations when used to for positioning within the FIC.
Previous studies have used corresponding nerve block situations to assess block success or when evaluating the effects of FICB. Lopez et al. [6] used the temperature sensation test on the anterior, lateral, and median side of the thigh 10 min after drug administration to evaluate the block effects, in which temperature sensation loss on all the three sides of thigh was defined as a complete block, loss on one or two sides of the thigh was defined as a partial block, and no loss of sensation was defined as block failure; complete and partial blocks were considered successful blocks, and the success rate in their study was 96.4%. According these criteria, 160 cases in the current study lost temperature sensation on any side of thigh 20 min after drug administration, accounting for 91.4% of all cases, similar the rate reported by Lopez. Meanwhile, 20 min after the block, 119 cases exhibited hypoesthesia on all three sides of the thigh, accounting for 68% of cases. Therefore, the success rate of LOR for FICB was 90% in the current study, while the rate of complete block was over 65%, indicating its high clinical efficiency.
Drug diffusing outside the FIC may also result in anesthetic effects. This is because the FIC is a type of deep fascia composed of dense connective tissues. Ropivacaine is a long-term local anesthetic; when injected above the FIC, some drug might penetrate the fascia iliaca and reach the FIC, resulting in the corresponding effects. Furthermore, 30 mL of 0.5% ropivacaine was used in the current study, which is a relatively high dosage and concentration; therefore, injection of the drug inside the iliopsoas, could still affect the corresponding nerve through trans-muscle diffusion and result in a successful block. However, 20 min after the block, the success rate of FICB was 98.0% and the complete block rate was 86.9%, rates, which were both significantly higher than the other two situations; thus, accurate positioning within the FIC could significantly improve success and complete block rates in FICB.
Ultrasound guided nerve block is good method in FICB; however, it has some limitations in clinical work. First of all it need ultrasonic equipment in special and it is not available in most hospitals and secondary it can increase the cost in clinic and also is not easily to be carried with operator at any time because of its inconvenient moving in addition of all above the clinical doctors still need a certain courses of training on the ultrasonic using so that they can keep reaching the well-done blocking effect. Therefore, corresponding ultrasound guiding nerve blocking, the traditional blocking without it still has its superiority in clinical work.
FICB has traditionally been performed using the method of blindly detecting the LOR, and the success rate of this technique varies in different studies [14]. In order to ensure block consistency in this study, all operations were performed by anesthetists with more than six years of experience with anesthesia, and all anesthetists had independently completed more than 50 FICB procedures before this study, thus ensuring the correctness and accuracy of needling in our study.
In recent years, ultrasound-guided nerve blocks have offered advantages such as increased success rates, shorter block onset times, longer block duration, lower effective concentrations, and higher patient satisfaction than traditional methods [15-21], resulting in its increasing application in clinical work. Dolan reported that ultrasound-guided FICB could effectively improve success block rates [12] because the needle could be accurately positioned within the FIC under ultrasound guidance, an observation similar to the results of the current study, in which accurate positioning of the needle within the FIC resulted in significantly higher successful block rate compared to rates in the other two groups.
The results of this study showed that accurate positioning in the FIC could improve the success rate and completing rate of block in FICB. While LOR had good clinical efficacy for FICB, its accuracy was not satisfactory. Because ultrasound maybe useful for accurately locating the FIC, it could effectively improve the accuracy of FIC positioning.
Conflicts of interest
All of the authors declare that they have no conflicts of interest regarding this paper.
References
- Cuignet O, Pirson J, Boughrouph J, Duville D. The efficacy of coutinuous fascia iliaca compartment block for pain management in burn patients undergoing skin grafting procedures. Anesth Analg 2004; 98: 1077-1081.
- Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg 1998; 87: 88-92.
- Godoy Monzon D, Iserson KV, Vazquez JA. Single fascia iliaca compartment block for post-hip fracture pain relief. J Emerg Med 2007; 32: 257-262.
- Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg 1989; 69: 705-713.
- Stevens M, Harrison G, Mc Grail M. A modified fascia iliaca compartment block has significant morphine-sparing effects. Anaesth Int Care 2007; 35: 949-952.
- Lopez S, Gros T, Bernard N, Plasse C, Capdevila X. Fascia iliaca compartment block for femoral bone fractures in prehospital care. Reg Anesth Pain Med 2003; 28: 203-207.
- Foss NB, Kristensen BB, Bundgaard M, Bak M, Heiring C, Virkelyst C, Hougaard S, Kehlet H. Fascia iliaca compartment blockade for acute pain control in hip fracture patients. Anesthesuology 2007; 106: 773-778.
- Gray AT. Ultrasound-guided regional anesthesia. Anesthesiology 2006; 104: 368-373.
- Awad IT, Chan V. Ultrasound imaging of peripheral nerves: a need for a new trend. Reg Anesth Pain Med 2005; 30: 321-323.
- Kizelshteyn G, Crevecoeur E. Anatomic consideration of the fascia iliaca compartment block. Anesth Analg 1990; 71: 200-212.
- Markman B, Barton FE. Anatomy of the subcutaneous tissue of the trunk and lower extremity. Plast Reconstr Surg 1987; 80: 248-254.
- Dolan J, Williams A, Murney E, Smith M, Kenny GN. Ultrasound guided fascia iliaca block: a comparison with the loss of resistance technique. Reg Anesth Pain Med 2008; 33: 526-531.
- Denny NM, Harrop-Griffiths W. Location, location, location! Ultrasound imaging in regional anaesthesia. Br J Anaesth 2005; 94: 1-3.
- Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d'Athis F. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: clinical and radiological analysis. Anesth Analg 1998; 86: 1039-1041.
- Eichenberger U, Stöckli S, Marhofer P, Huber G, Willimann P, Kettner SC, Pleiner J, Curatolo M, Kapral S. Minimal local anesthetic volume for peripheral nerve block: a new ultrasound guided, nerve dimension-based method. Reg Anesth Pain Med 2009; 34: 242-246.
- Latzke D, Marhofer P, Zeitlinger M, Machata A, Neumann F, Lackner E, Kettner SC. Minimal local anaesthetic volumes for sciatic nerve blockade: evaluation of ED99 in volunteers. Br J Anaesth 2010; 104: 239-244.
- Danelli G, Fanelli A, Ghisi D, Moschini E, Rossi M, Ortu A, Baciarello M, Fanelli G. Ultrasound vs nerve stimulation multiple injection technique for posterior popliteal sciatic nerve block. Anaesthesia 2009; 64: 638-642.
- Kapral S, Greher M, Huber G, Willschke H, Kettner S, Kdolsky R, Marhofer P. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med 2008; 33: 253-258.
- Perlas A, Brull R, Chan VW, McCartney CJ, Nuica A, Abbas S. Ultrasound guidance improves the success of sciatic nerve block at the popliteal fossa. Reg Anesth Pain Med 2008; 33: 259-265.
- Redborg KE, Antonakakis JG, Beach ML, Chinn CD, Sites BD. Ultrasound improves the success rate of a tibial nerve block at the ankle. Reg Anesth Pain Med 2009; 34: 256-260.
- Abrahams MS, Aziz MF, Fu RF, Horn JL. Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth 2010; 102: 408-417.