Case Report - Biomedical Research (2017) Volume 28, Issue 9
Clinical management of 10 cases of idiopathic scrotal calcinosis
Wen-bo Bu1, Guo-hua Ren2, Qiang Wang1, Meng-li Zhang1, Qian Zhang1, Xu Chen1, Fang Fang1* and Xiu-lian Xu1*1Institute of Dermatology, Chinese Academy of Medical Sciences, Peking Union Medical College, Nanjing, China
2Department of Dermatology, Heze Municipal Hospital of Shandong, Heze, China
- *Corresponding Author:
- Fang Fang
Institute of Dermatology
Chinese Academy of Medical Sciences
Peking Union Medical College, China
Xiu-lian Xu
Institute of Dermatology
Chinese Academy of Medical Sciences
Peking Union Medical College, China
Accepted on February 2, 2017
Abstract
Idiopathic scrotal calcinosis is a rare benign disease which presents with multiple asymptomatic various sized nodules on the scrotal skin wall. Few cases with multiple skin lesions have been reported. Between January 2011 and December 2014, 10 patients with multiple skin lesions were admitted and treated at our hospital. Here we reported their clinicopathological characteristics and our experience of management of these patients.
Keywords
Idiopathic scrotal calcinosis, Management, Surgery.
Introduction
Calcinosis cutis is a group of idiopathic skin calcifications that are classified into four major types according to aetiology: idiopathic, metastatic, iatrogenic, or injury and dystrophic calcinosis. Calcification of idiopathic calcinosis is usually localized to a specific area such as the genital area or chest [1,2]. Idiopathic scrotal calcinosis is the most common type which was first reported by Lewiuski [3]. Idiopathic scrotal calcinosis usually occurs in males between 20 to 40 years of age. Its characteristics include the presence of multiple and various sized nodules that progressively increase in number and enlarge in size, a single nodule or multiple nodules, and scattered, grouped or pedunculated lesions. The larger lesions may cause a heavy sensation, whereas some of the matured nodules may ulcerate to produce a white, chalky, and sand-like material.
Case Report
Idiopathic scrotal calcinosis is a rare metabolic disorder and commonly presents as a solitary skin lesion. Few cases with multiple skin lesions have been reported. Between January 2011 and December 2014, 10 patients with multiple skin lesions were admitted and treated at our hospital. Here we reported their clinicopathological characteristics and our experience of management of these patients.
The age at onset for these 10 patients ranged from 21 to 50 years. The course of the disease lasted from 2 months to 30 years. The skin lesion characteristics were as follows: the skin lesions were present with multiple and firm papules or nodules, some of which were grouped and some of which were solitary and no adhesion occurred between the lesions and the deep tissue of the scrotum. Each patient exhibited between 10 and 100 skin lesions, and the skin lesions varied in size. The skin lesions were small at first onset but tended to increase in size and number over time. Some patients described increased itching secondary to the lesions, and chalky white exudative material was reported in some patients. Serum calcium examinations were normal for all patients.
The skin lesions were completely removed in all patients under local or spinal anaesthesia, and good outcomes were achieved. The follow-up periods of patients ranged from 12 to 48 months, and no recurrence was reported.
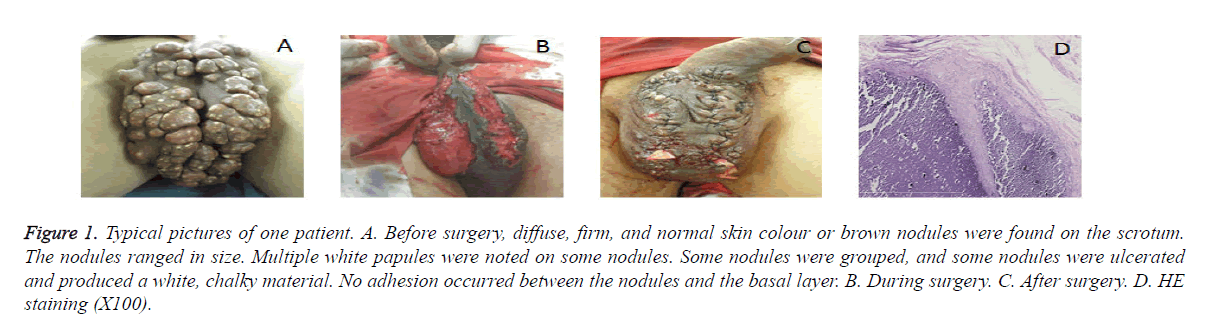
Of the 10 patients in this study, some patients presented with more than 100 nodules, and the maximum area of the grouped nodules was 5 × 5 cm (Figure 1A). After surgery the nodules were completely removed (Figures 1B and 1C). The patients experienced apparent heavy sensations that affected their quality of life.
Figure 1. Typical pictures of one patient. A. Before surgery, diffuse, firm, and normal skin colour or brown nodules were found on the scrotum. The nodules ranged in size. Multiple white papules were noted on some nodules. Some nodules were grouped, and some nodules were ulcerated and produced a white, chalky material. No adhesion occurred between the nodules and the basal layer. B. During surgery. C. After surgery. D. HE staining (X100).
Histological presentations of skin calcinosis in various locations were substantially similar, showing calcium deposits of varying sizes that stained dark blue with Hematoxylin and Eosin (HE) staining and black with von Kossa staining (Figure 1D).
Discussion
The pathogenesis of idiopathic scrotal calcinosis remains controversial. The controversy is currently focused on whether the occurrence of calcinosis is idiopathic or secondary to dermoid cysts or sweat gland cysts [4]. Some studies suggest that the absorption of the nodule wall leads to scrotal calcium deposits [5]. However, other studies suggest that the deposits form from a dilated epidermal cyst [6]. In the clinical, differential diagnosis is required to differentiate between secondary calcinosis and steatocystoma multiplex.
The treatment of idiopathic scrotal calcinosis includes non-surgical and surgical treatments. Non-surgical treatment includes the use of corticosteroids and a low-calcium diet with cellulose phosphate supplementation. Multiple nodules are generally indicated for surgical treatment. The majority of patients achieve satisfactory results after surgical excision [7]. In all patients in this study, the solitary or grouped nodules were excised en bloc in the superficial perineal fascia layer, whereas the normal tissues were preserved as much as possible. The small size of normal skin can provide favourable conditions for final closure due to the good elasticity of the scrotal skin. To avoid injury to subcutaneous blood vessels, the separation of the skin at the edges of skin defects is not recommended. The autologous scrotal skin was used to repair skin defects in all patients, which not only could preserve the normal appearance of the scrotum but also could avoid affecting normal scrotal function. Satisfactory results were achieved in both the appearance and function of the scrotum. Recurrence of scrotal calcinosis is rare but has been reported in a patent after surgical excision [8]. In this study, recurrence of scrotal calcinosis was not observed in any patient during follow-up.
In conclusion, idiopathic scrotal calcinosis is a rare benign disease which presents with multiple asymptomatic various sized nodules on the scrotal skin wall. Surgical treatment can achieve good outcomes.
Conflict of Interest
None
References
- Cohen PR, Tschen JA. Idiopathic calcinosis cutis of the penis. J Clin Aesthet Dermatol 2012; 5: 23-30.
- Aksoy HM, Ozdemir R, Karaaslan O, Tiftikcioglu YO, Oruc M, Koçer U. Incidental idiopathic calcinosis cutis in a rhytidectomy patient. Dermatol Surg 2004; 30: 1145-1147.
- Dubey S, Sharma R, Maheshwarl V. Scrotal calcinosis: idiopathic or dystrophic. Dermatol Online J 2010; 16: 5.
- Yahya H, Rafindadi AH. Idiopathic scrotal calcinosis: a report of four cases and review of the literature. Int J Dermatol 2005; 44: 206-209.
- Parlakgumus A, Canpolat ET, Caliskan K. Scrotal calcinosis due to resorption of cyst walls: a case report. J Med Case Rep 2008; 8: 375.
- Shah V, Shet T. Scrotal calcinosis results from calcification of cysts derived from hair follicles: a series of 20 cases evaluating the spectrum of changes resulting in scrotal calcinosis. Am J Dermatopathol 2007; 29: 172-175.
- Karaca M, Taylan G, Akan M, Eker G, Gideroglu K, Gul AE. Idiopathic scrotal calcinosis: surgical treatment and histopathologic evaluation of etiology. Urology 2010; 76: 1493-1495.
- Bhawan J, Malhotra R, Franks S. The so called idiopathic scrotal calcinosis. Arch Dermatol 1983; 119: 709.