Research Article - Current Pediatric Research (2023) Volume 27, Issue 8
Clinical characteristics and treatment response of childhood lichen planus: Insights from a Tunisian study.
Ichrak Khamassi1, Wiem Barbaria1*, H Zribi2, A.Ben Osman2
1Department of Pediatric, Habib Bougatfa Hospital, Bizerta, Tunisia
2Department of Dermatology, La Rabta Hospital, Tunis, Tunisia
- Corresponding Author:
- Wiem Barbaria Pediatric department, Habib Bougatfa Hospital in Bizerta-Tunisia E-mail: wiem.barbaria@gmail.com
Received: 28 July, 2023, Manuscript No. AAJCP-23-112430; Editor assigned: 31 July, 2023, Pre QC No. AAJCP-23-112430 (PQ); Reviewed: 14 August, 2023, QC No. AAJCP-23-112430; Revised: 21 August, 2023, Manuscript No. AAJCP-23-112430 (R); Published: 31 August, 2023, DOI:10.35841/0971-9032.27.07.1971-1975.
Abstract
Lichen Planus (LP) is an autoimmune, chronic inflammatory dermatological condition seldom encountered in children, with limited data available outside the Indian subcontinent.
This retrospective study delves into the epidemiological characteristics, clinical features, and treatment responses of LP in Tunisian children, spanning two decades. Among 255 LP patients, 11 (4.3%) were children aged 18 or younger. The median age of onset was 15 years, with a male-to-female ratio of 1.7. Pruritus was a universal symptom, with skin involvement observed in most cases. Classic LP was the predominant morphological variant. Histopathological analysis confirmed the diagnosis, revealing characteristic features. Treatment outcomes varied, with some patients experiencing complete clearance and others partial improvement. Actinic LP cases exhibited seasonal recurrences.
Our series specifies some epidemiological and clinical features of LP in Tunisian children. The data from the literature is insufficient to determine the characteristics of LP in children. Prospective studies are needed for a better understanding of the incidence and prognostic factors of this disease.
Lichen planus, Child, Skin disease
Introduction
Lichen Planus (LP) is a chronic autoimmune disorder characterized by inflammatory manifestations that affect the skin and mucous membranes. This condition typically presents as a series of distinctive, itchy, flat-topped, and polygonalshaped papules or plaques on the skin. LP is relatively uncommon in children, making it a less-studied dermatosis within this age group and its prevalence varies significantly across different age groups and geographical contexts [1].
While the medical literature has provided comprehensive insights into LP in adults, research focusing on childhood occurrences of this condition remains relatively limited, with the majority of reports originating from the Indian subcontinent [2]. This geographical bias has led to gaps in our understanding of LP in children from other parts of the world.
In this study, we present the epidemiologic characteristics, clinical features and response to treatment of LP in a series of Tunisian children.
Materials and methods
A retrospective study spanning two decades was conducted. We collected pediatric LP cases at the La Rabta hospital's dermatology department. Patients aged ≤ 8 years with LP or its variants were included. The diagnosis of cutaneous LP was considered if suggestive clinical features and histologic proof. In the cases of nails affection without skin involvement, the diagnosis was made clinically. Demographic details, lesion characteristics, histopathology findings, therapeutic interventions, and treatment outcomes were recorded.
Results
Among the 255 LP-diagnosed patients during the study period, a subset of 11 children (4.3%) met the inclusion criteria. All belonged to the Tunisian populace. Mean onset age was 15 years and varies from 6 years and 2 months to 17 years and 10 months. Male predominance was observed (male-to-female ratio of 1.7). There was no history of drug intake prior to the onset of LP. No positive family history of similar disease was available. The mean interval between the onset of symptoms and consultation was 6-7 months.
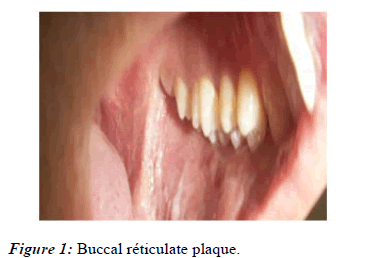
All patients with skin involvement had pruritus of varied severity. The involvement of skin was observed in nine cases. Cutaneous lesions were associated to mucosal involvement (Figure 1).
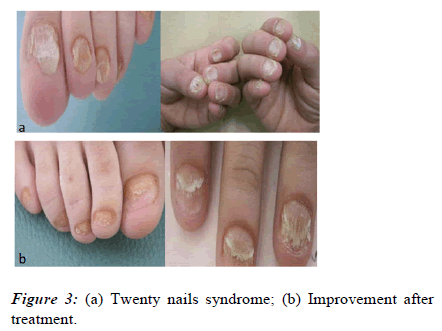
In one patient (n°5) and to nails involvement in another patient (n°2). Nails involvement was isolated in two cases (n°1 and 7). One patient (n°1) had a twenty nail syndrom (Figure 2 and 3).
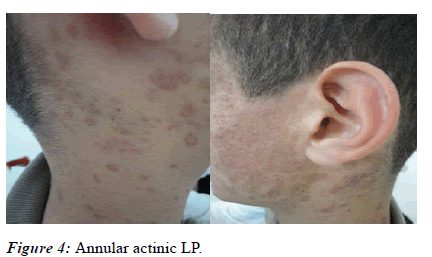
Widespread lesions were observed in 4 cases (n°2,5,6,11). The limbs were the most common sites of the lesions (nine cases).The involvement of the soles was observed in one case (n°2).The most common morphologic variant seen was classic LP (7 cases). Two patients had actinic LP (n°8,10) (Figure 4).
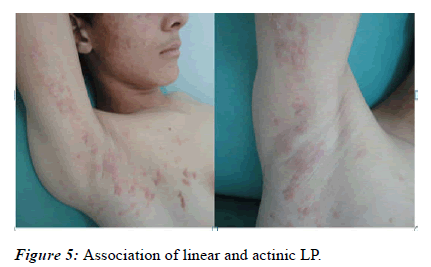
Linear lesions were observed in two cases (n°3,10). Patient n °10 showed bowth linear and actinic LP (Figure 5).
Association of linear LP and lichen nitidus was observed in one case (n°3).Histopathologic examination was performed in all cases with skin involvement. Nail and mucosal involvement were not verified by biopsy specimens. All patients demonstrated a bandlike lympho-histiocytic infiltration, hyperkeratosis and orthokeratosis. Pigment incontinence was seen in five cases (n° 1,2,3,8,10,11) and acanthosis in three cases (n°2,4,8).The presence of numerous melanophages confirmed the diagnosis of actinic LP in two patients (Table 1).
| Patient n° | A/G | Onset/consultation | Topography | Type of lesions | Type of LP |
|---|---|---|---|---|---|
| 1 | 6y 4m/M | 2m | 20 Nails | Longitudinal ridging | 20 nails dystrophy |
| Nail plate thinning | |||||
| 2 | 17y/F | 7m | UEs, T, S, FN | Violaceous and pigmented scaly papules | Classic LP |
| Longitudinal ridging, splitting of nails | |||||
| 3 | 15y 3m/M | 3m | UEs, LEs, Df, T, P | Scaly linear papules | Linear LP+Lichen nitidus |
| Scaly papules | |||||
| Translucent papules | |||||
| 4 | 18y/F | 3y | Scalp, In F | Erythematosus papules witn violaceous center | Classic LP |
| 5 | 17y/M | 2m | T, UEs, Bm | Pigmented papules | Classic LP |
| Oral reticulate plaque | |||||
| 6 | 9y/F | 1m | UEs, LEs, T, Df, Dh | Violaceous papules | Classic LP |
| Translucent micro papules | |||||
| koebner | |||||
| 7 | 17y/M | NR | LBT, RI, RM | Total nail dystrophy+pterygium | Nail LP |
| 8 | 18y/F | 2m | UEs, F, N | Annular pigmented papules | Actinic LP |
| Translucent micro papules | |||||
| 9 | 16y/M | NR | UEs, LEs | Violaceous papules | Classic LP |
| 10 | 14y/M | 2,5m | F, N, T, UEs | Scaly annular pigmented papules | Linear LP+Actinic LP |
| Linear Translucent papules | |||||
| 11 | 17y/M | 5m | UEs, LEs, T | Violaceous papules | Classic LP |
| Wickham striae |
Note: A/G: Age/Gender; Y: Years; M: Month; M: Male; F: Female; NR: Not Recorded;Ues: Upper Extremities; T: Trunk; S:Soles; FN: Finguer Nails; Les: Lower extremities; P: Penis; Inf: Inguinal fold; Bm: Buccal mucosa; Df: Dorsum of feet; Dh: Dorsum of hands; LBT: Left Big Toenail; RI: Right Index; RM: Right Major; F: Face; N: Neck
Table 1: Patients characteristics
The biopsy specimen of a translucent papule in case n°3 showed an expended dermal papillae containing a dense epitheloid infiltration confirming the diagnosis of lichen nitidus.
Details of the treatment offred to the patients are presented in Table 2.
| Patient n° | Treatment |
|---|---|
| 1 | Topical corticosteroid under occlusion |
| 2 | Topical corticosteroid, Oral corticosteroids, Antihistamines |
| 3 | Topical corticosteroid |
| 4 | Topical corticosteroid, Anti histamines |
| 5 | Topical corticosteroid, Antihistamines |
| 6 | Topical corticosteroid, Antihistamines, photoprotection |
| 7 | Topical corticosteroid under occlusion |
| 8 | Topical corticosteroid, Antihistamines, photoprotection |
| 9 | Topical corticosteroid, Antihistamines |
| 10 | Topical corticosteroid, Antihistamines, Photoprotection, Anti paludeens synthetisis |
| 11 | Topical corticosteroid,Anti histamines |
Table 2: Treatment data
The mean duration of follow up was 7 months and varies from 2 to 21 months. Four patients had complete clearance after a mean treatment duration of nine weeks (n°3,6,8,9). Four other patients had partial improvement (n°1,2,7,10).Patients with actinic LP had reccurence of lesions in summer.
Discussion
The epidemiology and clinical nuances of childhood LP unveil distinct patterns. While adult LP prevalence approximates 1% of the general populace [1], childhood occurrences are rarer, constituting merely 2%-3% [2-7] of cases and 2.5%-5% of pediatric dermatoses [8,9].
Prevalence is higher It seems more frequent among arabs and indian with a frequence of 7.5%-11.2% [10,11]. In our study the LP occurs in childhood in 4.3% of all cases. The average age of onset in the largest pediatric series varies from 7.1 to 10 years while The age of onset is older in our study (8,9,12-15). Childhood LP occurs at any age and to our knowledge theyoungest case reported is aged 15 days [8,16]. Handa and Nnoruka found that the lesions occured earlier in boys than in girls [9,17]. As in literature data, there was a slight boys predominance among our patients [8,9,17]. Sharma found a ratio of almost 2 boys:1 girl [12]. Kanwar explains this fact by a higher frequency of consultation for dermatological lesions in indian boys compared to girls [8]. The frank predominance of boys, found in the series of Balasubramaniam is explained by the Indian origin of the majority of patients [15].
As has been documented by all pediatric series, the limbs were the most commonly affected. The involvement of the trunk represented the second localisation (Table 3).
| Authors | Nb of cases | Localisation of lesions | |||||
|---|---|---|---|---|---|---|---|
| Limbs | Trunc | Face | Scalp | Nails | Mucosa | ||
| Kanwar [15] | 100 | 54 | 14 | - | 12 | - | |
| Handa [16] | 87 | 60 | 14 | 10 | - | - | - |
| Sharma [23] | 50 | 35 | 11 | 3 | - | - | 1 |
| Nnoruka [12] | 13 | 9 | 3 | - | 1 | 4 | |
| Kanwar [7] | 17 | 7 | 5 | 1 | - | - | |
| Our series | 11 | 9 | 6 | 2 | 1 | 3 | 1 |
Table 3: Distribution of the different locations of lesions according to published series
Koebner phenomenon was seen in only one patient. It was frequent (24%-38%) of cases in the series of Nnoruka [12], Handa [16], Sharma [12] and Kanwar [3]. It is however found in only 6% of cases in the series of Kanwar [8] and in only one patient in the series of Balasubramaniam [16].
The lesions were wide spread in four cases. The disseminated nature of the lesions is more common in children [15,17-19]. One patient had an asymptomatic reticulate plaque in the buccal mucosa with concomitant skin lesions. In the series of Kabita [20] erosive form is more common (63%) unlike other series where the reticular form predominates [8,9,21].
Nail LP was observed in three patients. Isolated typical nail LP with total onychodystrophy and pterygium was diagnosed in one case. Nail LP with longitudinal ridging and splitting concomitant to typical skin lesions was diagnosed in another case. In one patient the 20 nails showed evident thinning associated to nail plate roughness caused by excessive longitudinal striations.
Nail involvement is seen in 1 to 15% of cases in adult [1,2,10,22-24]. Tosti [25] found that the ingueal LP occurs during childhood in 10.8% of cases. It represents 6.8% of the nail pathology in children and 4% of pediatric dermatosis.The author conclude that the frequency of pediatric LP would be underestimated.
Classic LP was the commonest variant observed. Its frequency varies from 42% to 76% in several pediatric series [3,8,9,11-13,26]. However, one patient from six in the series Milligan has the classical form of LP [27]. According to Dammak this form is not a majority among children in southern Tunisia [28]. The linear LP wasseen in two patients. This variant is known to be more common in children than in adults. However, several publications report a higher frequency in adults [9,29,30]. Two patients had an annular actinic LP. One of them had a combination of linear and actinic LP. In our series, an association of lichen nitidus and lichen planus has been described. In the series of Kanwar [8], this association was found in 5% of cases. The prognosis of childhood LP is not well known. In our study, the response to treatment is partial or absent in half of cases.
Conclusion
Our series specifies some epidemiological and clinical features of LP in tunisian children. To our knowledge this is the largest Tunisian series about childhood LP. Prospective studies are needed for a better understanding of the incidence and prognostic factors of this disease. Furthermore, the findings from this study underscore the importance of early detection and management of childhood LP in Tunisia, as timely intervention can potentially improve outcomes and quality of life for affected children. Collaborative efforts with neighboring regions and international research initiatives can facilitate the development of prospective studies, allowing for a more comprehensive exploration of the disease's epidemiology, long-term prognosis, and potential therapeutic strategies in the Tunisian context.
References
- Pihelkow MR, Daoud MS. Chapter 26. Lichen Planus. 2016.
- Katz SI, Gilchrest BA, Paller AS, et al. Fitzpatrick's dermatology in general medicine. New York: McGraw-Hill 2008.
- Boyd AS, Neldner KH. Lichen planus. Journal of the American Academy of Dermatology 1991; 25(4):593-619.
- Kanwar AJ, Handa S, Ghosh S, et al. Lichen planus in childhood: a report of 17 patients. Pediatric dermatology 1991; 8(4):288-91.
- Marshman G. Lichen planus. Australasian journal of dermatology 1998; 39(1):1-3.
- Michel JL, Montelmard N, Fond L et al. Lichenoïd eruptions in child. Archives of pediatrics 1998; 5:909-15.
- Rybojad M, Moraillon I, Cordoliani F, et al. Lichen planus in the child: 25 cases. Clinical, follow-up and therapeutic aspects. In Annales de dermatologie et de Venereologie 2000; 127(6-7): 661.
- Tasanen K, Renko M, Kandelberg P, et al. Childhood lichen planus after simultaneous measles-mumps-rubella and diphtheria-tetanus-pertussis-polio vaccinations. British Journal of Dermatology 2008; 158(3):646-8.
- Kanwar AJ, De D. Lichen planus in childhood: report of 100 cases. Clinical and experimental dermatology 2010; 35(3):257-62.
- Handa S, Sahoo B. Childhood lichen planus: a study of 87 cases. International journal of dermatology 2002; 41(7):423-7.
- Kanwar AJ, Belhaj MS. Lichen planus among Arabs—A study from Libya. The Journal of Dermatology 1984; 11(1):93-6.
- Ben Yahia K, Kourda M, Kennou H, et al. Le lichen: A propos de 100 cas. Maghreb Médical 1998; (324):21-3.
- Sharma R, Maheshwari V. Childhood lichen planus: a report of fifty cases. Pediatric dermatology 1999; 16(5):345-8.
- Nanda A, Al-Ajmi HS, Al-Sabah H. Childhood lichen planus: a report of 23 cases. Pediatric dermatology 2001; 18(1):1-4.
- Rybojad M, Moraillon I, Laglenne S, et al. Lichen planus in children: 12 cases. InAnnales de Dermatologie et de Venereologie 1998; 125(10):679-681.
- Balasubramaniam P, Ogboli M, Moss C. Lichen planus in children: review of 26 cases. Clinical and experimental dermatology 2008; 33(4):457-9.
- Pusey WA. Lichen planus in an infant less than six months old. Archives of Dermatology and Syphilology 1929; 19(4):671-2.
- Nnoruka EN. Lichen planus in African children: A study of 13 patients. Pediatric dermatology 2007; 24(5):495-8.
- Kanwar AJ, De D. Lichen planus in children. Indian Journal of Dermatology, Venereology and Leprology 2010; 76:366.
- Chatterjee K, Bhattacharya S, Mukherjee CG, et al. A retrospective study of oral lichen planus in paediatric population. Journal of Oral And Maxillofacial Pathology: JOMFP 2012; 16(3):363.
- Woo VL, Manchanda-Gera A, Park DS, et al. Juvenile oral lichen planus: a report of 2 cases. Pediatric Dentistry 2007; 29(6):525-30.
- MM B. Lichen planus and lichenoid disorders. Rook/Wilkinson/Ebling textbook of dermatology 1998:1899-926.
- Samman PD. The nails in lichen planus. British Journal of Dermatology 1961;73:288-92.
- Pérez Oliva N, Velasco Vaquero B. Lichen planus of the nails. Cutis (New York, NY) 1993; 52(3):171-2.
- Tosti A, Piraccini BM, Cambiaghi S, et al. Nail lichen planus in children: clinical features, response to treatment, and long-term follow-up. Archives of dermatology 2001; 137(8):1027-32.
- Luis-Montoya P, Domínguez-Soto L, Vega-Memije E. Lichen planus in 24 children with review of the literature. Pediatric dermatology 2005; 22(4):295-8.
- Milligan A, Graham-Brown RA. Lichen planus in children—a review of six cases. Clinical and experimental dermatology 1990; 15(5):340-2.
- Dammak A, Masmoudi A, Boudaya S, et al. Lichen plan actinique de l’enfant (à propos de 6 cas). Archives de pédiatrie 2008; 15(2):111-4.
- Hartl C, Steen KH, Wegner H, et al. Unilateral linear lichen planus with mucous membrane involvement. Acta dermato-venereologica 1999; 79(2):145-6.
- Long CC, Finlay AY. Multiple linear lichen planus in the lines of Blaschko. British Journal of Dermatology 1996;135(2):275-6.