- Biomedical Research (2008) Volume 19, Issue 2
Changes in plasma fibrinogen, homocysteine and lipid profile in coronary artery disease patients of north Indian (Punjab) popu-lation
Kuldip Singh and Amandeep Singh
Department of Biochemistry, Government Medical College, Amritsar (Punjab), India
- *Corresponding Author:
- Kuldip Singh
House No. 4319, Word No. 13
Near Punjab Hindustan Combine
G. T. Road, Bara -Sirhind
Fategarh Sahib 140406 (Punjab)
India
E-mail: kuldip70@rediffmail.com
Accepted date: May 03 2008
Abstract
Conventional risk factors such as age, smoking, hyperlipidemia and hypertension do not ex-plain all the mortality and morbidity due to coronary artery disease. Novel factors like plasma fibrinogen, homocysteine, C - reactive protein have been recently recognized as in-dependent risk factors for coronary artery disease. The objective of the present study was to examine the change in plasma fibrinogen, homocysteine along with lipid profile in the pathogenesis of angiographically established coronary artery disease. 75 male patients in the age range of 30-60 years with angiographically established coronary artery disease and equal number of age and sex matched normal healthy subjects were re-cruited in the present study. Coronary artery disease patients had significant high plasma fibrinogen, homocysteine, total cholesterol, triglyceride and LDL-cholesterol levels whereas the level of HDL-cholesterol significantly decreased in them as compared to normal healthy subjects (control). Elevated levels of plasma fibrinogen, homocysteine contribute signifi-cantly to the risk of coronary artery disease and might be considered in screening program to identify individuals at increased thrombotic risk.
Key Words
Fibrinogen, Coronary Artery Disease (CAD), Homocysteine.
Introduction
Coronary artery disease (CAD) represents one of the major causes of death and morbidity in the World. Prevention of CAD can be approached in many ways including health promotion campaigns, specific protection strategies, life style modification programs, early detection and control of risk factors and constant vigilance of emerging risk factors [1]. The concept of cardiovascular risk factors arose from the Framing Heart Study, a landmark study in cardiovascular disease epidemiology. Prospective cardiovascular Munster (PROCAM), simple scoring scheme identified risk factors such as age, smoking, hypertension, hyperlipidemia, diabetes, obesity etc [2,3].
Despite these classic risk factors, a continued focus on newer factors is warranted as they may further improve our ability to predict future risk and manage cardiovascular disease (CVD), when they are included along with the classic risk factors. The study of these new risk factors is important since the ability to accurately predict the CVD risk of specific individual based on his/her conventional risk factor profile is limited [4]. These new risk factors are called Novel risk factors, which includes fibrinogen (primarily thrombosis marker), homocysteine (primarily atherogenic marker) and Creactive protein [5,6].
Several studies [4,5,6] conducted in different parts of the world on normal healthy subjects have reported that elevated levels of plasma fibrinogen and homocysteine are associated with CAD as an independent of other risk factors but studies reporting fibrinogen levels in coronary artery patients are limited. Moreover very few studies have been conducted in India to the best of our knowledge and also the increasing prevalence of CAD due to changing lifestyle, gave us an impetus to evaluate the changes in plasma fibrinogen, homocysteine along with lipid profile such as total cholesterol, triglyceride, High density lipoproteins-cholesterol (HDL- cholesterol) and low density lipoproteins cholesterol (LDL- cholesterol) in CAD patients of North India (Punjab) population.
Material and Methods
Subjects
The present study was conducted on 75 male patients in the age range of 30 - 60 years with angiographically established coronary artery disease (CAD) and equal numbers of age, sex matched normal healthy controls were the subjects of the present study. CAD patients were taken from the Department of Cardiology, Guru Nanak Dev Hospital attached to Govt. Medical College -Amritsar. CAD-patients had not received any lipid lowering drugs before taking the blood samples. All subjects were vegetarian, non-smoker, non-diabetic and non-alcoholic and there was no positive family history of CAD in these subjects.
Blood Sampling
5ml of peripheral venous blood was collected by vein puncture using a dry, disposable syringe between 8 AM- 9AM after an overnight fast. Blood was collected in sterile tubes containing potassium oxalate as anticoagulant for plasma separation. For serum separation, blood was collected without potassium oxalate. Plasma and serum were separated by centrifugation at 3000 rpm for 15 mints and were stored at 4°C and used for various biochemical assays.
Biochemical Assays
1. Plasma Fibrinogen: Fibrinogen content in plasma was measured by tyrosine method as given in Varley et al, 1980 [7]. The fibrin clot is formed in the diluted plasma by the addition of calcium ions. The clot then separated from the solution and washed free of other proteins. The clot is dissolved in alkali and the protein is determined with the Folin-Ciocalteu reagent. Blue color developed was measured at 680nm. Results were expressed as mg/dl of fibrinogen.
2. Homocysteine: Homocysteine level in plasma was estimated by using homocysteine microplate substrate trapping enzymes assay (Diazyme laboratories). This technology employs genetically engineered enzymes that lack catalytic activity but specifically and tightly trap their substrate or product molecules as the basis of diagnostic test.
3. Total cholesterol: Serum total cholesterol level was assayed by the method of Allain et al 1974 [8].
4. Triglyceride: Serum triglyceride level was estimated by using the method of Mc Gowan et al, 1983 [9].
5. HDL-cholesterol: HDL- cholesterol was estimated by the method of Grillo and Izzo, 1985 [10].
6. LDL-cholesterol: serum LDL-cholesterol was esti-mated from the primary measurements by using the em-pirical equation of Friedewald et al 1972 [11]. Serum LDL cholesterol = Total cholesterol – (HDL cho-lesterol - Triglyceride/5).
Statistical Analysis: Numerical data were performed as mean values ± S.D. The statistical significance was evaluated by students “t” test and the difference between CAD –patients and normal health subjects (control) was considered significant at p<0.05.
Results and Discussion
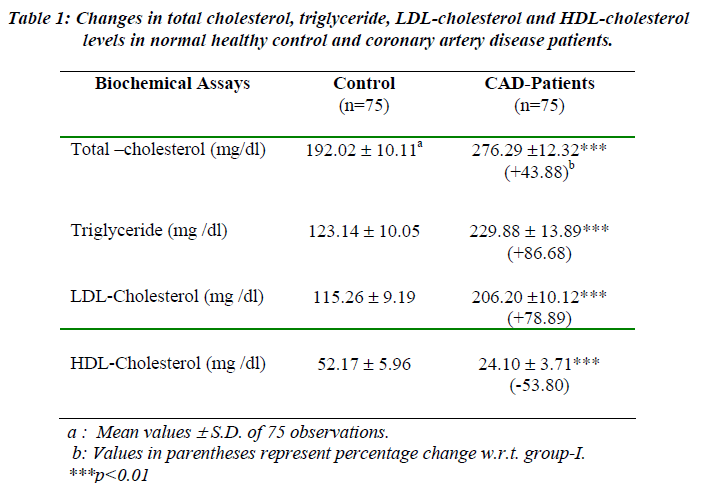
A significant increase was observed in the serum total cholesterol, LDL-cholesterol and triglyceride level from 192.02 mg/dl ± 10.11 to 276.29 mg/dl ± 12.32 (by 43.88% with respect to control subjects), 115.26 mg/dl ± 9.19 to 206.20 mg/dl ± 10.12 (by 78.89% with respect to control subjects) and 123.14 mg/dl ± 10.05 to 229.88 mg/dl ± 13.89 (by 86.68% with respect to control subjects) respectively in CAD patients (Table-1), whereas the level of serum HDL-cholesterol was significantly decreased from 52.17 mg/dl ± 5.96 to 24.10 mg/dl ± 3.71 in CAD patients (Table- 1). The existence of a causal relationship between altered levels of lipids & lipoproteins and CAD is well-established fact [12,13]. The United States Lipid Research Clinical trial has shown that cholesterol makes most significant individual contribution to risk of CAD [14,15]. Our findings of alteration in serum total cholesterol, LDL-cholesterol, triglyceride and HDL-cholesterol levels in the CAD patients are in agreement with the repots [16,17,18] that hyperlipidemia is one the risk factor for the onset of CAD.
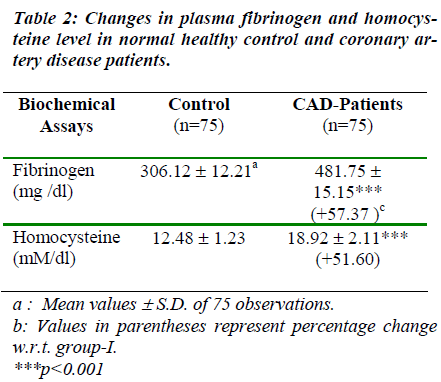
In CAD patients, we found a significant increase (p<0.001) in fibrinogen level by 57.37% with respect to control subjects that is from 306.12 ± 12.21 mg/dl to 481.75 ± 15.15 mg/dl (Table-2). Fibrinogen is a circulating glycoprotein that acts at final step in the coagulation response to vascular and tissue injury. There are several mechanisms by which fibrinogen may increase cardiovascular risk. First, it binds specifically to activated platelets via glycoprotein IIb/IIIa, contributing to plate aggregation. Second, increased fibrinogen levels promote fibrin formation. Third, it is a major contributor to plasma viscosity. Finally, fibrinogen is an acute phase reactant that is increased in inflammatory states [19,20]. A significant increase of fibrinogen level in the present study suggesting that fibrinogen is directly associated with CAD and also indicates that fibrinogen may play an important role in plaque rupture & thrombosis in response to inflammation.
Homocysteine, a nonessential, sulphur containing amino acid and an intermediate from the metabolic demethylation of dietary methionin found to be significantly increased (p<0.001) from 12.48 ± 1.23 to 18.92 ± 2.11 mM/dl by 51.62% with respect to normal healthy subjects (Table-2). The increase of homocysteine level might induce atherothrombosis via the formation of homocysteine thiolactate, a byproduct of oxidation of homocysteine. Homocysteine thiolactate combines with LDL to form foam cells [21,22].. The LDL rich foam cells embed themselves in the vascular endothelium and become fatty streak, which is the beginning of an atherosclerotic plaque. Homocysteine thiolactate could also impair the oxidative phosphoryation and enhancement of the proliferation and fibrosis of smooth muscle cells [23]. Homocysteine may also induce atherosclerosis by affecting endothelial derived relaxing factor that is nitric oxide. Nitric oxide combined with homocysteine in the presence of oxygen to form snitroso homo-cysteine, which inhibits sulfhydryl dependent generation of hydrogen peroxide. The bioavailability of NO. is decreased due to endothelial cell injury. This dysfunctional endothelial may be due to generation of oxygen radicals produced by homocysteine. Homocysteine may also reduce the antioxidant status, which could injure endothelial cells [24]. Therefore, a significant increase of homocysteine level in the present work could be responsible for the pathogenesis of CAD.
In conclusion, the aforementioned observations suggested that elevated levels of fibrinogen and homocysteine could be responsible for the pathogenesis of CAD and thereby the estimation of fibrinogen and homocysteine might be considered for screening programs, aimed for identifying individuals at high risk for cardiovascular disease in Indian population.
References
- Knopp RH. Risk factors for coronary artery disease in women. Am J Cariol 2002; 89(S12A): 28E-34E.
- Assmann G, Cullen P and Schulte H. Simple scoring calculating the risk of acute coronary events based on 10 year followup of the Prospective Cardiovascular Munster (PROCAM) study. Circulation 2002; 105: 310-315.
- Iftikar JK and Christie MB. Conditional risk factor for atherosclerosis. Mayo Clin Proc 2005; 80: 219-30.
- Gensini GF, Comeglio M, Colella A. Classical risk factor and emerging elements in the risk profile for coronary artery disease. Eur Heart J 1998; 195: 53A-61A.
- Ramachandran A, Sathyamuthy I, Snehaltha C, Satyavani K, Sivasankari S, Misra J, Girinath MR, Viswanathan V. Risk variable for coronary artery disease in Asian Indians. Am J Cadiol 2001; 88: 201-202.
- Harish RB, Govindaraju V and Manjunath CN. Risk prediction-Homocysteine in coronary heart disease. Ind J Clin Biochem 2007; 22: 18-21.
- Varley H, Gowenlock AK and Bell M. Determination of plasma fibrinogen: Tyrosine Method (Lempert). Practical Clinical Biochemistry (William Hienemann Medical Book Ltd. London) 1980, 5th Edition; 557-558.
- Allain CC, Poon S, Chan CSG, Richmond S and Fu PC. An enzymatic method for estimating serum cholesterol. Clin. Chem., 1974; 20: 470-474.
- Mc Gowan BA, Artiss MW, Stranberg JD, Zak DR. Peroxidase coupled method for the colorimetric determination of serum triglycerides. Clin Chem 1983; 29: 538-542.
- Grillo F and Izzo C. Serum highdensity lipoprotein determination using enzyme. Clin. Chem. 1985; 31: 746.
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of lowdensity lipoprotein in serum using a simple empirical equation. Clin Chem 1972; 18: 499-509.
- Casrelli WP. Lipids risk factors and ischemic heart disease. Atherosclerosis 1996; 124: S1-S9.
- Yeolekar ME. Coronary artery disease in Asian Indians. JPGM 1998; 44: 26-28.
- Wilson PW. High density lipoprotein, low density lipoprotein and coronary artery disease. Am J Cardiol 1990; 66: 7A-10A.
- Elisaf MS, Siamopoulos KC, Tselegarides TJ, Bairaktari ET, Goudevenous JA, Tselepis AD, Tsolas OE, Sideris DA. Lipid abnormalities in Greek patients with coronary artery disease. Inter J Cardiol 1997; 59: 177-184.
- Sloop GD, Garber DW. The effect of low density lipoprotein and high density lipoprotein on blood viscosity correlation with their association with risk of atherosclerosis in human. Clin Sci 1997; 92: 473-479.
- Jappesen J, Hein HO, Suadicani P, Gytelberg F. Relation of high TG, HDL Cholesterol and LDL Cholesterol to the incidence of isheamic heart disease. Arteriosclerosis, Thrombosis and Vascular Bio 2005; 85: 113.
- Kashyap ML. Cholesterol and atherosclerosis: a contemporary persperative. Ann Acad Med. Singapore 1997; 26: 517-523.
- VonEyben EF, Mouritsen EA, Home J, Montvilas P, Dimcevski G, Rasmussen IH, Kristensen, LL, Sucin G, VonEyben R. Fibrinogen and other coronary risk factors. Metabolism 2005; 54: 165-170.
- Koenig W. Fibrinogen in cardiovascular disease: an update. Thomb Haemost 2003; 89: 601-609.
- Ernst E. Fibrinogen as a cardiovascular risk factor Interrelationship with infections and inflammation. Eur Heart J 1993; 14: 82K-87K.
- Angeline T, Aruna RM, Ramadevi K, Mohan G, Jeyaraj N. Homocysteine status and acute myocardial infarction among Tamilians. Ind. J. Clin. Biochem. 2005; 20: 18-20.
- Miller AL. Cardiovascular disease-Towards a unified approach. Alt Med Rev 1996; 3: 132-147.
- McCully KS, Wilson RB. Homocysteine theory of arteriosclerosis. Arteriosclerosis.1975; 22: 215-227.