Case Report - Anesthesiology and Clinical Science Research (2023) Volume 7, Issue 1
Case report on antiphospholipid antibody: clinical research on Asherson syndrome
Thummala Naga Shivani*, Bondula Sai Upendra
1Department of Anesthesiology, JNTUA College of Engineering, Anantapur, India
- Corresponding Author:
- Thummala Naga Shivani
Department of Anesthesiology, JNTUA College of Engineering, Anantapur, India
E-mail: nagashivani.thummala95@yahoo.com
Received: 11-Aug-2022, Manuscript No. AAACSR-22-71701; Editor assigned: 15-Aug-2022, AAACSR-22-71701 (PQ); Reviewed: 29-Aug-2022, QC No. AAACSR-22-71701; Revised: 27-Dec-2022, Manuscript No. AAACSR-22-71701 (R); Published: 05-Jan-2023, DOI: 10.35841/aaascr.7.1.131
Citation: Shivani TN, Upendra BS. Case report on antiphospholipid antibody: clinical research on Asherson syndrome. Anaesthesiol Clin Sci Res. 2023;7(1):1-4.
Abstract
Introduction: Thromboses in the arterial and venous systems characterize the Antiphospholipid Syndrome (APS). In the arterial, venous or minor arteries as well as pregnancy morbidity, when antiphospholipid antibody titters are chronically increased. Since virtually any organ can be involved, the clinical presentation of APS is very varied. Abdominal manifestations are rare but may be life threatening and include Budd-Chiari syndrome. We discuss a 26 years old lady with primary APS brought to In March 2017, the Bangabandhu Sheikh Mujib Medical University (BSMMU) in Dhaka, Bangladesh, was established. On aspirin medication with ascites for which she had been receiving treatment for abdominal tuberculosis. Following clinical and laboratory evaluation, she was diagnosed as a case of Budd-Chiari syndrome with portal hypertension and initiated treatment with warfarin.
Main symptom and/or important clinical finding: 25 years old female admitted in Acharya Vinoba Bhave Rural hospital on date 7-07-21 with the chief complaint of excessive breathing, weakness, fatigue, high blood pressure, headache blood clot etc. After physical examination and investigation doctor diagnose a case of antiphospholipid antibody syndrome.
The main diagnoses, therapeutic interventions and outcome: After physical examination and investigation doctor diagnose a case antiphospholipid antibody syndrome medical management was provided to the patient calcium and multivitamin supplementary was given for 7 days to enhance immune function. Tablet valproate 1.5 mg, anticoagulant tablets and atenolol 50 mg beta blocker tablets. Vitamin B12 for supplementary he was taking all treatment and outcome was good.
Conclusion: She was response to all medication as well as doctor treatment and her recovery was good.
Keywords
Aortic thrombosis, Cerebral infarcts, β2 glycoprotein 1 antibodies, Ascherson’s syndrome.
Introduction
Antiphospholipid Antibody syndrome (APLA) is a complicated illness that affects both men and women that is rarely seen in everyday practice. APLA is a fairly varied disease with a wide range of clinical manifestations [1-3].
The prevalence antiphospholipid antibody syndrome is defined as thromboembolic issues in the presence of regularly increased antiphospholipid antibody titters and/or pregnancy morbidity. It can manifest in a variety of ways and affect any organ and it is currently affecting most surgical and medical professions [4-6].
Antiphospholipid syndrome causes microangiopathy, which affects small blood arteries throughout the body. The majority of individuals develop thrombocytopenia, with hemolytic anaemia and disseminated intravascular coagulation occurring less commonly. Antibodies against the most prevalent antibodies linked to CAPS have been found as lupus anticoagulant and anticardiolipin [7,8].
Clinical signs of APS are generally nonspecific in there hasn't been a thrombotic incident; we recently saw a young man who had recently been diagnosed with hypertension and kidney disease who had primary APS. His kidney biopsy findings, which revealed chronic microangiopathy features under electron microscopy, multiple organ involvement and a triplepositive antiphospholipid antibody profile later, validated the diagnosis of APS [9,10].
Anti-beta-2-glycoprotein-1 the most commonly implicated antibodies include antibodies, lupus anticoagulant and antibeta- 2-glycoprotein-1 antibodies and anticardiolipinantibody. 1 and anticardiolipin antibody are the most often implicated antibodies. Anticoagulant activity is the primary function of these antibodies. These antibodies, contrary to their name, are linked to a rather than a bleeding diathesis, this is a procoagulant disorder. Antiphospholipid (APL) binds to membrane plasma proteins causes them to be activated chain reaction involving a prothrombotic state is caused by a combination of molecules are all involved in the healing process. While the popular belief is that thrombosis is the primary cause of APS, the importance of atherosclerosis should not be overlooked [11].
Discovery of antibodies and our understanding of the syndrome's pathobiology we suggest a method to explain how anti-beta-2-glycoprotein-1 antibodies have been associated to a number of different diseases of clinical conditions. The occurrence of thromboembolic problems and Antiphospholipid Antibody (APLA) syndrome is defined as pregnancy morbidity in the presence of Antiphospholipid Antibody (APLA) syndrome titters that are constantly growing. It can affect any organ and has a wide range of clinical symptoms making it a contemporary concern in a wide range of surgical and medical specialties. The example of a 34 year old woman with APLA syndrome who was diagnosed with the cerebral venous thrombosis and deep vein thrombosis of the left leg veins are discussed in this article. Three types of APLAs were found to be increased (IgG, IgM and activated protein C). Other autoimmune or systemic disorders were not found in clinical or laboratory tests, R is being used to treat the patient. Antiphospholipid Syndrome (APS) is an autoimmune disorder marked by hypercoagulability and the risk of thrombosis of all arterial bed segments of arterial and venous circulations, as well as pregnancy morbidity. Multiple organs are affected by this illness, which manifests itself in a variety of clinical symptoms. The most severe type, known as Catastrophic Antiphospholipid Syndrome (CAPS), affects less than 1% of patients and is linked to multiple organ thrombosis. The most common signs are DVT, PE and strokes are all examples of deep venous thrombosis. Anti-beta-2-glycoprotein-1 antibodies, lupus anticoagulant and anticardiolipin antibody are all examples of anti-beta-2-glycoprotein-1 antibodies the most typically implicated antibodies [12].
Recurrent thromboembolic events in the veins and/or the arteries, as well as pregnancy morbidity are all factors to consider are clinical features of the syndrome. Aside from these clinical signs, the existence of a distinct set of autoantibodies directed against certain phospholipid binding proteins is a need for the illness. The three laboratory tests evaluated in the updated version are antibodies against 2- glycoprotein I (a2GPI) and Cardiolipin (aCL), as well as the Lupus Anticoagulant functional assay (LAC) [13].
Case Presentation
Patient specific information: A 25 years old female admitted in Acharya Vinoba Bhave rural hospital on date 7-07-21 with the chief complaint of excessive breathing, weakness, fatigue, high blood pressure, headache, blood clot etc. After physical examination and investigation doctor diagnose a case of antiphospholipid antibody syndrome.
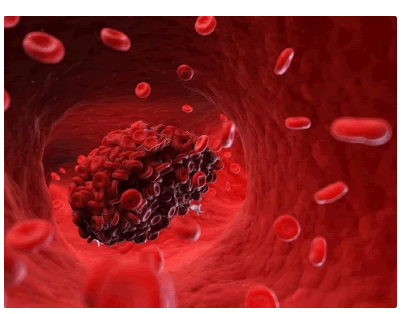
Primary concern and symptoms of the patient: Chief complaint of patient excessive breathing, weakness, fatigue, high blood pressure headache blood clots. After physical examination and investigations doctor diagnose a case of antiphospholipid antibody syndrome Asherson syndrome (Figure 1).
Relevant past interventions with outcome: History of antiphospholipid antibody syndrome 6 month back for which she was hospitalized. After CBC test, LFT test and other in Asherson syndrome was observed he took all support to treatment and his outcome was good.
Clinical finding: The patient was conscious and well oriented to time, place, date his body build was moderate and he had maintained good personal hygiene. Her weight 45 kg in milestone development the patient is anemic.
Timeline: 6 months ago, he was admitted in the hospital antiphospholipid antibody syndrome is treated with this drug. He is currently being treated for antiphospholipid antibody syndrome. Currently he was admitted for the treatment of antiphospholipid antibody syndrome calcium and multivitamin supplementary was given for 7 days to enhancement function.
Diagnostic assessment: On the basis of the of patient’s history collection, physical examination, CBS blood test investigation was also done WBC count (20,000/cumm) less than normal platelets count was less 1.57 lacks command haemoglobin was less 7.5 and other investigation was also done.
Diagnostic challenges: No any challenging during the diagnostic evaluation.
Diagnosis: After physical examination and investigation doctor diagnosed a case of antiphospholipid antibody Asherson syndrome.
Prognosis: It was good.
Therapeutic interventions: Medical management was provided to the patient calcium and multivitamin supplementary was given for 7 days to enhance immune function tablet valproate 1, 5 mg anticoagulant tablet, atenolol 50 mg beta blocker tablet, vitamin B12 for supplementary. She was taking all treatment and outcome was good, no any change in restorative.
Follow up and outcome
Clinical and patient assessment outcome: Patient conditions was improved important check out investigation and other test results to preventing to progression of disease and trying to reserve any sign and symptoms doctor advice to follow up blood investigation and other examination to know the disease progression.
Interventions adherence and tolerability: Patient took all prescribed medications regular but sometimes he was refused to take medication. He also followed the dietician advised. Dietician was advised healthy food and rich in calcium and multivitamin supplementation. Her interventional adherence was satisfactory.
Nursing perspective: Monitor the vital signs of patient person hourly multifluid and electrolytes balance.
Results and Discussion
APS is a type of autoimmune disease that causes thrombosis in the arteries and veins, as well as recurrent foetal loss and thrombocytopenia. It was first discovered in people with SLE (Systemic Lupus Erythematosus), which was later connected to other autoimmune disorders. Primary APS is another name for this condition which is a syndrome that can arise without any underlying disease. CAPS, a deadly variation of APS that affects about 1% of the population, was initially identified in 1992. APS is a thrombotic autoimmune disease that manifests itself in a variety of ways. For the diagnosis of definite APS, at least one clinical and one laboratory criterion is required.
Based on HIRA data, which is a state wide required insurance programme, offered by the Korean government, this is the first nationwide population based investigation of the incidence, prevalence and related consequences of APS. In contrast to a prior population based investigation, our findings revealed that the incidence rate of APS varied by gender and age group. Anionic phospholipids are antigenic bilaminar phospholipids that are found on the inner sides of membranes. Accessory proteins like beta-2-glycoprotein-1, on the other hand, may help to speed up and stabilize the shift to hexagonal antigenic forms. Antiphospholipid antibodies are thought to be made up of a variety of proteins of antiphospholipid I combination of antibodies and anti-beta-2-glycoprotein antibodies or I complex or antibodies and anti-beta-2-glycoprotein antibodies against phospholipids exclusively.
The phrase APLA syndrome refers to the clinical link between APLAs and a hypercoagulability syndrome. It's an autoimmune condition marked by thromboembolic issues and pregnant morbidity. Antibodies are the most often identified subgroups of APLAs. Rather than clinical bleeding, Thromboembolic events have been associated to lupus anticoagulant antibodies. Both pro and anticoagulant pathways can be disrupted by APL.
Sarcoidosis Expression Antiphospholipid Antibody Syndrome (APS), sarcoidosis and Systemic Lupus Erythematosus (SLE) are chronic immunological dysregulation illnesses causes are unknown in the previous 60 years, only a few incidences of individuals have been diagnosed with sarcoidosis and SLE. In this investigation, we present two cases with sarcoidosis and SLE that coexisted, with problems linked to anticardiolipin antibodies were found in both cases. Clinical, serological and pathological information are all available in each case confirmed the diagnoses and both patients responded well to treatment. The relationship between sarcoidosis, SLE and APS is unusual and it can make treatment challenging. Thrombosis manifests itself DVT, pulmonary thromboembolism and stroke are all examples of thromboembolism in people with APS. Valvular illness and intracardiac thrombus development are the most common cardiac symptoms of APS. Only 4% of the time does a myocardial infarction occur autoimmune illnesses, such as chronic inflammation is recognized to promote early atherosclerosis in systemic lupus erythematosus, rheumatoid arthritis, systemic sclerosis and other autoimmune illnesses and APS. While the role of APL antibodies in an etiology of thrombosis in APS is well understood, the existence of certain cardiovascular risk factors or medical conditions in these patients increases the risk of thrombosis [14].
Conclusion
Traditional cardiovascular risk factors have been shown to substantially enhance the risk of thrombosis and atherosclerosis time and time again. Due to the existence of antibodies against APL and chronic inflammation, both of which lead to early atherosclerosis thrombotic load is already high in APS patients. To prevent future endothelial and vascular damage, primary care physicians must be vigilant in identifying and actively managing conventional risk factors. To treat diabetes, hypertension, obesity, strict dietary and physical activity modifications are required. Furthermore, in the elderly, women, diabetics and silent myocardial infarction are prevalent further more silent in the elderly, women and diabetics. A common concern is myocardial infarction quitting smoking is another way to reduce the progression of atherosclerotic disease. To achieve improved patient outcomes, a multidisciplinary strategy combining primary care doctors, for coordinated management of these patients, hematologists and cardiologists are essential.
References
- Naik SN, Raghavendra Y. Antiphospholipid antibody syndrome: A case report. Ayu. 2017;38(1-2):62-5.
- Luma HN, Doualla MS, Temfack E, et al. The antiphospholipid antibody syndrome: A case report. Int Med Case Rep J. 2012;5:63-7
- Strakhan M, Hurtado-Sbordoni M, Galeas N, et al. 36 year old female with catastrophic antiphospholipid syndrome treated with eculizumab: A case report and review of literature. Case Rep Hematol. 2014;2014:704371.
- Tsiakas S, Skalioti C, Kotsi P, et al. Case of an unusual diagnosis of primary antiphospholipid syndrome with multiple clinical complications. Oxf Med Case Rep. 2020;2020(12):117
- Parsi M, Rai M, Swaab R, et al. Rare case of catastrophic antiphospholipid antibody syndrome: a case report and review of traditional cardiovascular risk factors implicated in disease occurrence. Cureus. 2020;12(3):e7221.
- Durrani OM, Gordon C, Murray PI, et al. Primary antiphospholipid Antibody Syndrome (APS): Current concepts. Surv Ophthalmol. 2002;47(3):215-38.
- Castañeda Ospina SA, Cardona Maya WD, Bueno Sanchez JC, et al. Pregnancy outcome in women with antiphospholipid syndrome and alloimmunity: A case report. Sao Paulo Med J. 2003;121(6):248-50.
- Pashnina IA, Krivolapova IM, Fedotkina TV, et al. Antinuclear autoantibodies in health: autoimmunity is not a synonym of autoimmune disease. Antibodies. 2021;10(1):9.
- Mohammad S, Bhute A, Acharya N, et al. Moschcowitz syndrome or thrombotic thrombocytopenic purpura and antiphospholipid antibody syndrome as a rare cause of thrombocytopenia in pregnancy mimicking hemolysis, elevated liver enzymes, and low platelets syndrome in a patient with bad obstetric history: A diagnostic dilemma. J Obstet Gynaecol Res 2020;12(4):250-3.
- Murray CJ, Abbafati C, Abbas KM, et al. “Five Insights from the global burden of disease study 2019.” Lancet. 2020;396(10258):1135-59.
- Vos T, Lim SS, Abbafati C, et al. “Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the global burden of disease study 2019.” Lancet. 2020;396(10258):1204-22.
- Franklin RC, Peden AE, Hamilton EB, et al. “The burden of unintentional drowning: global, regional and national estimates of mortality from the global burden of disease 2017 Study.” Inj Prev. 2020;26(Supp 1): 83-95.
- James SL, Castle CD, Dingels ZV, et al. “Estimating global injuries morbidity and mortality: methods and data used in the global burden of disease 2017 study.” Inj Prev. 2020;26(Supp 1):125-53.
- Behzadifar M, Spencer LJ, Chris DC, et al. “Global injury morbidity and mortality from 1990 to 2017: results from the global burden of disease study 2017.” Inj Prev 2020;96-114.