Case Report - Asian Journal of Biomedical and Pharmaceutical Sciences (2022) Volume 12, Issue 86
Cancer and infertility: A major problem.
Shubhangi P Kawale1, Ranjit Ambad2*, Radhika Lahoti3, Minal Kalambe4
1Department of Clinical Embryology, Datta Meghe Medical College Wanadongri Hingna, Nagpur, India
2Department of Biochemistry Datta Meghe Medical College Shalinitai Meghe Hospital and Research Centre Wanadongri, Nagpur, India
3Clinical Embryologist Datta Meghe Medical College Shalinitai Meghe Hospital and Research Centre Wanadongri, Nagpur, India
4Department of OBGY Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences Sawangi (Meghe) Wardha, India
- Corresponding Author:
- Ranjit Ambad
Department of Biochemistry
Datta Meghe College of Physiotherapy
Nagpur, India
E-mail: am.sawan32@gmail.com
Received: 27-Jan-2022, Manuscript No. AABPS-22-55768; Editor assigned: 29-Jan-2022, Pre QC No. AABPS-22-55768(PQ); Reviewed: 12-Feb-2022, QC No. AABPS-22-55768; Revised: 15-Feb-2022, Manuscript No. AABPS-22-55768(R); Published: 22-Feb-2022, DOI:10.35841/2249-622X.86.110
Citation: Ambad R, Kawale SP, Lahoti R, et al. Cancer and infertility: A major problem. Asian J Biomed Pharmaceut Sci. 2022;12(86):110
Abstract
Introduction: People dealing with cancer are at the majority level in the world’s population. But thanks to decades of treatment and oncological diagnosis cancer patients’ survival has significantly improved. A Cancer patient deals with both life-threatening diagnoses and also the desire to have a child. During the treatment of cancer, the fertility in both males and females have reduced. Although children and young adults have benefited the most from advances in the treatment of cancer this progress has come at a high cost, with long-term treatment side effects leading to infertility in patients. However, recent fertility preservation techniques and increased awareness of fertility preservation options for family planning have improved the survival rates of infertility among cancer patients. Fertility is survivorship must be discussed before starting therapy in order to make informed decisions about treatment options, family planning, and fertility preservation strategies. Conclusion: The article concludes that cancer has a major impact on the patients even after the treatment. Different types of cancer cause premature infertility and sometimes immediate infertility in them. There are preservation techniques through which patients can be able to conceive. Patients must be aware of the procedure in order to be knowledgeable about cryopreservation before treatment begins.
Keywords
Cancer, Infertility, Treatment, Preservation, Counseling.
Introduction
Cancer affects a large proportion of the world’s population today. More than 135000 people under the age of 45 years are diagnosed with cancer every year. Infertility is the most common problem that a cancer patient or survivor faces. Number of cancer can affect the fertility in both male and female i.e. Breast cancer, Thyroid cancer, Hodgkin lymphoma, Leukemia, Ovarian cancer, Testicular cancer. Chemotherapy and radiation therapy, in addition to the high doses of medications, are used to treat cancer. These treatment are the sometimes the major cause for the infertility in male and female. These problems cause stress and cause the negative impacts on their quality of life in most of the young survivors [1]. New techniques for preserving fertility are being developed for this purpose, giving cancer patients and survivors more options for conceiving. It is more important to discuss the fertility preservations to the patients before the treatment so that the chances of their fertility can increase. Fertility is a survivor issue that must be discussed to starting therapy in order to make informed decisions about treatment options, family planning, and fertility preservation strategies.
This review has included discussion of the type of cancer that affects a person's fertility. Cancer treatment causes infertility, causing the survivor to suffer. Fertility preservation options are available for both male and female cancer patients prior to treatment [2].
Cancer affecting fertility
Breast cancer
• Mostly occurs in women, and rarely in men.
• Breast cancer most common in women rather than other malignant cancer [3].
• Most of the women who suffer from the breast cancer are younger than 45 years [4].
• It develops when some of the breast cells begin to divide abnormally; the cells divide faster than healthy cells.
• The breast cancer evaluates the gonadotropin-releasing hormone (GnRH) agonists during the breast cancer chemotherapy; the rate of premature ovarian insufficiency in the control was approximately 31%, demonstrating that premenopausal women retain ovarian function [5].
• In early stage, faces the less threat of treatment cause on fertility.
Testicular cancer
• This cancer mainly occurs in male reproductive organ.
• It is particularly injurious to the fertility in men.
• It can also cause the decrease in the sperm concentration and patient [6].
• Azoospermia may occur in men.
• Some patients' infertility is impacted by testicular cancer treatment [7].
• Testicular cancer requires high-dose pelvic irradiation, which can permanently harm testicular function and cause erectile dysfunction (ED) [8].
Thyroid cancer
• It is one of the fastest growing cancers.
• It occurs in both male and female.
• It commonly considered as a women’s problem, but onethird of hypothyroidism occur in men.
• In women the average age of menopause slightly decreases [9].
Hodgkin’s lymphoma
• The cancer occurs in both male and female.
• It is a cancer of the lymphatic cell, which harms the immune system of the body [10].
• It is found in people aged 20 to 40, as well as those over the age of 55.
• HL is caused by age, systemic therapy, and pelvic radiation exposure [11].
• In male most of the proportion in them are having normal fertility.
• In male it is less likely to be so much affective.
• Most appropriate treatment for the HL is ABVD which improves the fertility ratio.
Leukemia
• This is a cancer of blood forming tissues, includes the bone marrow which reduced the body’s ability to fight through the infection.
• It occurs in both male and female.
• Women with leukemia face a significant risk of infertility due to gonadotoxic conditions, which result in lower fertility rates in those who receive chemotherapy [12].
• The fertility ratio has been found out in lower digits (17%) in patients with AML and ALL [13].
• In males there is patients with acute leukemia have reported azoospermia in 46%.
• And most males have been reported with oligospermia [14].
Ovarian cancer
• This occurs in female genital organs.
• This cancer grows unnoticed until it spreads to the pelvic region and stomach.
• This cancer can be more difficult to treat and can be fatal.
• A women diagnosed with the ovarian cancer have a major risk of miscarriage and having infertility in them.
These are some of the most common cancers that cause infertility problems both during and after treatment.
Treatments affecting fertility
Currently, approximately 1 in 1000 young people aged 16 to 35 years has been cured of cancer in childhood or adulthood. As a result, the regimens they use have a significant impact on their future fertility prospects. Cancer treatment necessitates high-dose radiation, which includes chemotherapy. Chemotherapeutic agents damage the growing cells in mature and immature follicles in women, depending on the type of drugs used, the amount of dose, and the age of the patients, which can result in the removal of some or the entire follicle from the body. Female patients with breast cancer who have tumors larger than 1cm, cancer that has spread to the lymph nodes, or cancer with hormone receptors must undergo chemotherapy treatment [15], these patients have a greater chances of having fertility issues. The chemotherapeutic agents such as cyclophosphamide are very toxic to the ovaries particularly to the primordial follicles [16].
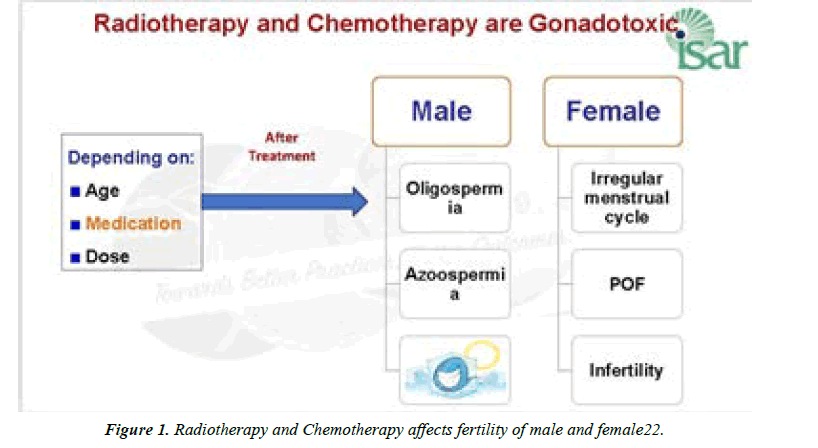
In male patients with Hodgkin's Lymphoma and Testicular cancer, it is concluded that the integrity of the sperm DNA is damaged due to the initiation of treatment. Although the treatment poses the greatest threat to male cancer survivors' fertility due to the high dosage of treatment they receive, which may affect sperm production and result in poor quality spermatozoa. Radiation and chemotherapy have cytotoxicity that affects the testicular germinal cells, including Sertoli cells, but to a lesser extent on the Leydig cells, resulting in frequent impairment of spermatozoa without hypogonadism [17]. (Figure 1)
Preservation of fertility and counseling
Many survivors want to have their biological family; many studies have shown that the desire to start a family increases during the treatment and survival of a cancer diagnosis [18]. However, this life-saving treatment, which increases the patient's survival rate, may result in immediate or the risk of infertility in patients [19]. This issue has taken a huge consideration among the clinical and the cancer survivors who faces problem during conceiving a child. In women, the loss of fertility has a greater impact and causes more stress than a cancer diagnosis [20]. The same is true for men, as the treatment causes a reduction in spermatozoa in them, making it difficult for them to conceive. In men who have testicular cancer in an advanced stage, the testicles must be amputated through surgery, resulting in immediate infertility. To address these issues, new technologies have emerged that allow young patients to preserve their fertility before beginning treatment. However, the discussion with patients about preservation is more difficult between the diagnosis and the start of cancer treatment. Therefore, it is important to discuss the preservation techniques with the patients so that they don’t face any difficulties in their further future. As a result, clinicians should be able to provide patients with accurate and up-to-date information about this issue. As a result, fertility-preserving options for young women with cancer include hormonal stimulation with cryopreservation of oocytes and embryos, as well as laparoscopic oophorectomy with tissue storage for later transplantation or in-vitro follicle maturation. However in men the best option for the preservation of the fertility is cryopreservation of sperm before treatment. Because of the relative ease of sperm banking, fertility challenges in men with cancer are less complex than those in women. Therefore, cryopreservation of human sperm for up to 28 years has been reported, with no apparent loss of fertility capacity. Because there are so many procedures involved in preservation, most patients have this discussion just before starting treatment, and they believe they don't have time to pursue a fertility consultation without delaying planned treatment. But this counseling with the patients may open their chances of conceiving a child.
Conclusion
In the past, a cancer diagnosis was almost always a death sentence. Modern medicines have increased cancer patients' chances of survival. However, after dealing with a lifethreatening diagnosis and high-dose treatment, patients develop a strong desire to start a biological family as a new life resolution. However, because of the types of cancer and treatments, which include high doses of drugs, chemotherapy, radiation therapy, and surgery, patients experience immediate and premature infertility. With the advancement of modern medicine and the development of new techniques, survivors have gained new hope for their desire to have a child. Fertility preservation is an option for patients, which includes preserving oocytes and embryos in women and human sperm in men before starting the treatment. The patients need to be counsel about the preservation before the treatment because many patients suffers from the lack of knowledge of the cryopreservation of fertility in male and female before of the lack of discussion between the clinicians and the patients. By studying all these facts about cancer affecting fertility it is concluded that even after dealing with life-threatening diagnosis patients can face fertility issues too. The cancer from patients still leaves a major impact in a patient’s life.
Conflict of Interest
Nil
Source of Funding
Nil
References
- Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Human Reprod update. 2009;15(5):587-97.
- Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: an Ethics Committee opinion. Fertility and sterility. 2018;110(3):380-6.
- Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA: a cancer journal for clinicians. 2008;58(2):71-96.
- American Cancer Society. Breast cancer facts & figures. Am Cancer Soc;2007.
- Lambertini M, Moore HC, Leonard RC, et al. Gonadotropin-releasing hormone agonists during chemotherapy for preservation of ovarian function and fertility in premenopausal patients with early breast cancer: a systematic review and meta-analysis of individual patient?level data. J Clinical Oncol. 2018;36(19):1981.
- Petersen Pm, Skakkebaek Ne, Rorth M, et al. Semen quality and reproductive hormones before and after orchiectomy in men with testicular cancer. J Urol. 1999;161(3):822-6.
- Kim C, McGlynn KA, McCorkle R, et al. Fertility among testicular cancer survivors: a case-control study in the US. J Cancer Survivorship. 2010;4(3):266-73.
- Nakayama K, Milbourne A, Schover LR, et al. Gonadal failure after treatment of hematologic malignancies: from recognition to management for health-care providers. Nat Clinical Prac Oncol. 2008;5(2):78-89.
- Ceccarelli C, Bencivelli W, Morciano D, et al. 131I therapy for differentiated thyroid cancer leads to an earlier onset of menopause: results of a retrospective study. J Clinic Endocrinol Metabol. 2001;86(8):3512-5.
- Jacobson MH, Mertens AC, Spencer JB, et al. Menses resumption after cancer treatment?induced amenorrhea occurs early or not at all. Fertility and sterility. 2016;105(3):765-72.
- Watson M, Wheatley K, Harrison GA, et al. Severe adverse impact on sexual functioning and fertility of bone marrow transplantation, either allogeneic or autologous, compared with consolidation chemotherapy alone: analysis of the MRC AML 10 trial. Cancer: Interdisciplinary Int J Am Cancer Soc. 1999;86(7):1231-9.
- Reimer T, Kempert S, Gerber B, et al. SLCO1B1* 5 polymorphism (rs4149056) is associated with chemotherapy-induced amenorrhea in premenopausal women with breast cancer: a prospective cohort study. BMC cancer. 2016;16(1):1-8.
- Hallak J, Kolettis PN, Sekhon VS, et al. Cryopreservation of sperm from patients with leukemia: is it worth the effort?. Cancer: Interdisciplinary Int J Am Cancer Soc. 1999;85(9):1973-8.
- Razzak AR, Lin NU, Winer EP. Heterogeneity of breast cancer and implications of adjuvant chemotherapy. Breast Cancer. 2008;15(1):31-4.
- Gadducci A, Cosio S, Genazzani AR. Ovarian function and childbearing issues in breast cancer survivors. Gynecological endocrinology. 2007;23(11):625-31.
- Joshi S, Savani BN, Chow EJ, et al. Clinical guide to fertility preservation in hematopoietic cell transplant recipients. Bone Marrow Transplantation. 2014;49(4):477-84.
- Edge B, Holmes D, Makin G. Sperm banking in adolescent cancer patients. Arch dis childhood. 2006;91(2):149-52.
- Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clinic Oncol. 2006;24(18):2917-31.
- Schover LR. Patient attitudes toward fertility preservation. Pediatric Blood & Cancer. 2009;53(2):281-4.
- Feldschuh J, Brassel J, Durso N, et al. Successful sperm storage for 28 years. Fertility and sterility. 2005;84(4):1017-e3.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref