Case Report - Ophthalmology Case Reports (2020) Volume 4, Issue 1
Annular choroidal detachment one year after argus-II retinal prosthesis implantation.
Mohsen Farvardin1,2, Mohammadkarim Johari1,2*, Mohammad Nami3,4 and Reza Farvardin51Department of Ophthalmology, Poostchi Ophthalmology Research Center, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
2Farvardin Eye Clinic, Shiraz, Iran
3Department of Neuroscience, School of Advanced Medical Sciences and Technologies, Shiraz University of Medical Sciences, Shiraz, Iran
4Neuroscience Center, INDICASAT-AIP, Panama City, Republic of Panama, Central America
5Medical student, Students' Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
- Corresponding Author:
- Mohammadkarim Johari
Department of Ophthalmology
Shiraz University of Medical Sciences
Shiraz
Iran
E-mail: mkjoharii@gmail.com
Accepted date: April 7, 2020
Citation: Farvardin M, Johari MK, Nami M, et al. Annular choroidal detachment one year after argus-II retinal prosthes is implantation. Ophthalmol Case Rep. 2020;4(1):23-25.
Abstract
Purpose: to report annular choroidal detachment one year after Argus-II retinal prosthesis implantation. Patient: A 63-year-old male patient who had a history of Argus-II retinal implantation surgery in his left eye a year ago, referred to the clinic complaining of two weeks left eye irritation, redness, and mild pain. Result: On physical examination, the intraocular pressure (IOP) was 5 mmHg (hypotonia) and his visual acuity with the system on had no change compared to the previous examination. Rubeotic vessels were seen on iris especially around the papillary margin. On B-scan sonography annular choroidal detachment was seen, so the patient underwent 23 gauge vitrectomy and silicon oil was injected.Conclusion: This is the first report on annular spontaneous choroidal detachment after Argus-II retinal prosthesis.
Keywords
Annular choroidal detachment, Argus-II implantation, Tadafinil, Safety, Post-operative complications.
Introduction
The implantation of Argus-II retinal microarray electrode chip in cases with advanced to end-stage retinitis pigmenta (RP) has become a new frontier in vitreoretinal surgery. Yet, novel approaches are expectedly subject to a set of surgical challenges. Post-operatively, patients with Argus-II retinal implants are given steroid and topical antibiotics and advised to refer for typical follow-up visits to have any possible adverse events well-monitored [1-3]. Though we have had trivial to no challenges and intra and post-operative complications in 3 out of 4 patients with advanced retinitis pigmentosa (RP) who underwent Argus-II retinal implantation, one case developed annular choroidal detachment almost a year after surgery. This concise case report depicts the challenges faced in the above condition.
Case Report
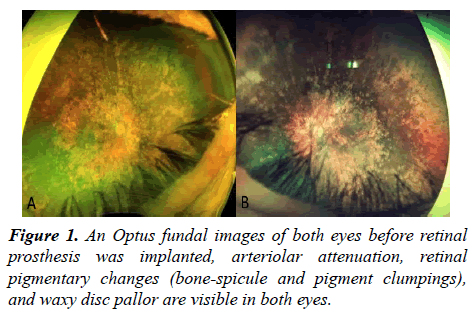
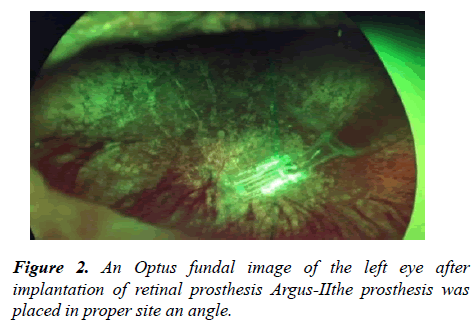
A 63 year-old male patient referred to our clinic complaining of two weeks left eye irritation, redness, and mild pain. He had a history of Argus-II retinal implantation surgery in his left eye a year before the presentation (certificate approval number: 11195211152). He has been a case of end-stage RP (Figures 1 and 2).
Before surgery, his visual acuity was no light perception (NLP) in both eyes and after prosthesis implantation, in the last rehabilitation session, his visual acuity in the left eye was increased to good hand motion perception. Of note, he obtained a grating visual acuity better than 2.9 LogMAR when the Argus-II system was on. Over the last visual rehabilitation session, all his retinal prosthesis’ electrodes (i.e. 60 out of 60) were active with acceptable impedances and thresholds.
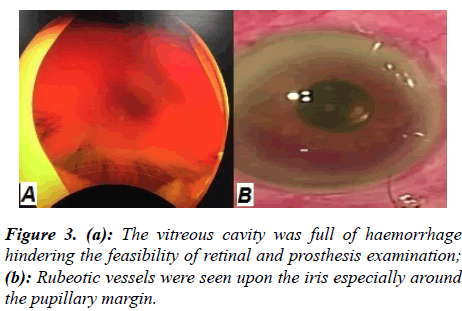
Having faced with the new complaint, the patient was precisely examined. On physical examination, the intraocular pressure (IOP) was 5 mmHg (hypotonia) and his visual acuity with the system on had no change compared to the previous examination. The globe was formed and no evidence of laceration or instrument extrusion was noted. The anterior chamber was formed, however, rubeotic vessels were seen on iris especially around the papillary margin. The intraocular lens (IOL) was properly in place. Since the vitreous cavity was full of hemorrhage, retina and prosthesis examination was not feasible (Figure 3). Upon a technical check of the Argus-II functionality, all 60 electrodes were found to be functional with mildly increased thresholds as compared to the previous examination. B-scan sonography was requested revealing annular choroidal detachment (CD) which stopped posteriorly in the margin of a retinal prosthesis. Also, some areas on CD were suspected for concurrent retinal detachment.
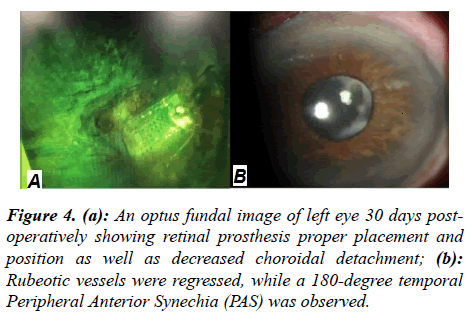
The condition was described to the patient. He was debriefed about the urgent need for surgical intervention. The patient underwent 23-gauge three-port deep vitrectomy on the same day. Upon surgery, initially, three ports were placed then the vitreous cavity was cleaned (with no observable RD) and barrier laser therapy was done over the whole retina posteriorly to the margin of a retinal prosthesis having avoided any damage to the micro-array electrode ship then the air-fluid exchange was done and Finally, the vitreous cavity was filled with silicon oil (5700) and intravitreal bevacizumab (1.25 mg) was injected. One day postoperatively, the anterior chamber was formed while a droplet of silicon oil was observed in the anterior chamber. The IOL was properly in place, the retinal prosthesis was perfectly visible and CD was decreased. Topical and systemic steroids, as well as topical antibiotics, were prescribed and tapered-off over a month.
One month after the operation, the IOP was 13 mmHg.His visual acuity remained stable and the silicon droplet was observed in the anterior chamber. The rubeotic vessels regressed and 180 degrees temporal peripheral anterior synechia (PAS) was observed. Also, the retinal prosthesis was easily visible. Though the CD was decreased, it failed to fully disappear (Figure 4).
Discussion and Conclusion
This is, to the best of our knowledge, the first report on annular spontaneous choroidal detachment after Argus-II retinal prosthesis implantation. The Argus-II retinal prosthesis (Second Sight Medical Products, Sylmar, CA, USA) is an epiretinal prosthesis approved for implantation in the patients with advanced retinitis pigmentosa [4-6]. Five-year longitudinal results of the Argus-II trials have revealed the long-term safety of the implanted device in patients with RP. A review of 30 eyes undergoing Argus-II implantation reported no related significant adverse effect in 60% of patients (18/30) [6]. Meanwhile, conjunctival erosion, hypotony, conjunctival dehiscence, presumed endophthalmitis, need for re-tacking and rhegmatogenous retinal detachment have been reported in some studies [6]. An important point in the case reported here was the history of sildenafil use for erectile dysfunction before complication. In a review of literature, there are some cases of choroidal congestion and intraocular hemorrhage following the use of phosphodiesterase inhibitors such as sildenafil and tadalafil. This has been correlated with the vasodilatory effect of such drugs on ocular vessels [7-10]. Likewise, there has been a report on tadalafil-induced subretinal and choroidal haemorrhage in a patient with unsuspected choroidal melanoma [11]. In our case, there was neither a history of trauma before complication nor any evidence favoring melanoma in ocular sonography. Our patient is stable at this time and we plan to pursue a close follow-up on his condition.
Conflict of Interest Statement
Authors declared no conflict of interest subjected to this work and no funding support received in preparation of the present report. The present case report portrays annular spontaneous choroidal detachment after Argus-II retinal prosthesis in a case of advanced retinitis pigmentosa.
References
- Dagnelie G, Christopher P, Arditi A, et al. Performance of real-world functional vision tasks by blind subjects improves after implantation with the Argus(R) II retinal prosthesis system. Clin Exp Ophthalmol. 2017;45(2): 152-59.
- Luo YH, Zhong JJ, da Cruz L. The use of Argus(R) II retinal prosthesis by blind subjects to achieve localisation and prehension of objects in 3-dimensional space. Graefes Arch Clin Exp Ophthalmol. 2015;253(11):1907-14.
- Dorn JD, Ahuja AK, Caspi A, et al. The detection of motion by blind subjects with the epiretinal 60-electrode (argus II) retinal prosthesis. JAMA Ophthalmol. 2013;131(2):183-89.
- Luo YH, da Cruz L. The argus (®) II retinal prosthesis system. Prog Retin Eye Res. 2016;50:89-107.
- Farvardin M, Afarid M, Attarzadeh A, et al. The argus-II retinal prosthesis implantation; from the global to local successful experience. Front Neurosci. 2018;12:584.
- da Cruz L, Dorn JD, Humayun MS, et al. Five-year safety and performance results from the argus II retinal prosthesis system clinical trial. Ophthalmology. 2016;123(10):2248-54.
- Roy R, Panigrahi PK, Saurabh K, et al. Central serous chorioretinopathy following oral tadalafil intake. Clin Exp Optom. 2014;97(5):473-74.
- Smal C, Lepiece G, Bonnet S. Central serous chorioretinopathy following the use of phosphodiesterase 5 inhibitors. Revue Medicale de Liege. 2017;72(11):475-77.
- Markowitz M, Rankin M, Mongy M, et al. Rehabilitation of lost functional vision with the argus II retinal prosthesis. Can J Ophthalmol. 2018;53(1):14-22.
- Moschos MM, Nitoda E. Pathophysiology of visual disorders induced by phosphodiesterase inhibitors in the treatment of erectile dysfunction. Drug Des Devel Ther. 2016;8:3407-13.
- Abramson DH, Rollins IS, Lin A, et al. Tadalafil-induced subretinal and choroidal hemorrhage in a patient with an unsuspected uveal (choroidal and ciliary body) melanoma. Arch Ophthalmol. 2006;124(7):1058-60.