Review Paper - Anesthesiology and Clinical Science Research (2023) Volume 7, Issue 1
Anaesthesia for thyrotoxic patients: Perioperative management review
Yilkal Tadesse Desta*
Department of Anaesthesia Critical care and Pain Medicine, Bahirdar University, Bahirdar, Ethiopia
- Corresponding Author:
- Yilkal Tadesse Desta
Department of Anaesthesia Critical care and Pain Medicine
Bahirdar University, Bahirdar, Ethiopia
E-mail: destayilkal999@gmail.com
Received: 27-Dec-2022, Manuscript No. AAACSR-23-84386; Editor assigned: 30-Dec-2022, PreQC No. AAACSR-23-84386(PQ); Reviewed: 13-Jan-2023, QC No. AAACSR-23-84386; Revised: 18-Jan-2023, Manuscript No. AAACSR-23-84386(R); Published: 25-Jan-2023, DOI:10.35841/aaacsr-7.1.132
Citation: Desta YT. Anaesthesia for thyrotoxic patients: Perioperative management review. Anaesthesiol Clin Sci Res. 2023;7(1):132
Abstract
The aim of this review essay is to analyses anesthesiology perioperative assessment and management of patients with thyroid disease. A special care is paid to difficult airway recognition and resolving this situation, in a patient who may also have significant co-morbidity. Moreover; it is understood that anesthetists are responsible and need to strictly involve in early recognition and management of certain perioperative catastrophic events in associated with thyroid surgery. Recent discussions on Anesthesia Case Management for thyroidectomy are discussed with special interest on the perioperative appreciation of complications and the need for urgent anesthetic interventions.
Keywords
Anesthesia, Thyroid surgery.
Introduction
An intimate knowledge of the anatomy, physiology, pathophysiology, pharmacology, and specific issues in relation to anesthesia case management for thyroidectomy is essential to provide high-quality care. Airway management may be difficult despite normal airway assessment predictions due to impingement of a thyroid mass on the laryngeal and tracheal structures. Anesthesia for thyroidectomy may also be complicated by airway problems such as retrosternal extension of the gland; therefore the anesthetists should pay particular care to preoperative airways assessment and should be able to deal with acute airway complications in the perioperative phase. Anesthetists must be prepared to use emergency life threatening airway adjuncts in case a patient cannot be ventilated or intubated with increasing hypoxemia. Thyroid diseases which have anesthetic implications include hypothyroidism, hyperthyroidism and certain malignancy conditions requiring thyroidectomy. Additionally thorough knowledge of the pathophysiology and potential complications associated with thyroidectomy is necessary as well for competent patient care [1].
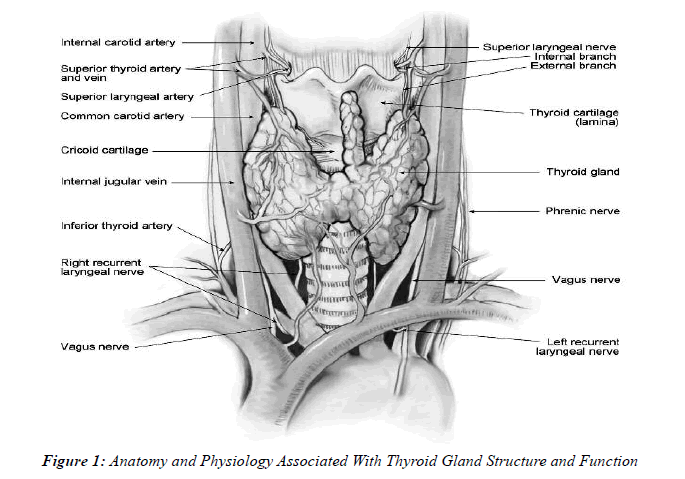
It is essential that all patients having an elective thyroidectomy should be in controlled or euthyroid state before surgery since sympathetic nervous system hyperactivity is associated with increased amounts of thyroid hormone. There is also multiple preoperative anti-thyroid medication regimen need to be taken that effectively blunt thyroid hormone hypersecretion, even though a rare event, thyroid storm should still be considered potentially to occur during the perioperative period Figure 1.
The thyroid gland is butterfly-shaped and composed of 2 lobes which are connected by a median tissue mass called the thyroid isthmus which is located on the anterior and anterolateral aspect of the trachea immediately just inferior to the larynx.
• The thyroid gland is the largest endocrine gland in the body, which weighs about 20 g in a healthy adult. The major blood supply arises from the superior thyroid arteries, which branched from the external carotid artery and inferior thyroid arteries and venous supplies are via inferior, middle, and superior thyroid veins.
• Blood flow is about 5 times the weight of the gland, and, therefore, thyroid is one of body parts with increased blood supplies per gram of tissue in the body.
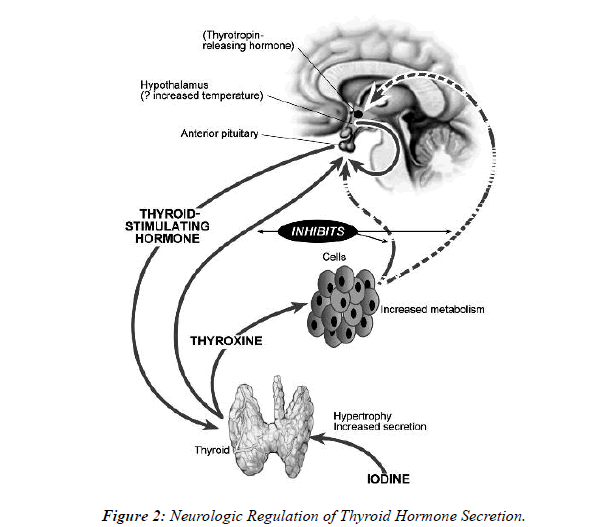
• The recurrent laryngeal nerve responds for abduction and adduction of the vocal cords by the posterior cricoarytenoid muscles and the lateral cricoarytenoid muscles, respectively Figure 2.
• Neurologic Regulation of Thyroid Hormone Secretion is by the path way that thyroid-stimulating hormone is transported to the thyroid gland, which stimulates the production of T4 and T3 by the thyroid gland.
• The homeostatic regulation of thyroid hormone production is maintained by a compensatory negative feedback loop as seen from the Figure 2.
• Thyrotropin-releasing hormone is secreted from the hypothalamus in the brain, which initiates the production of Thyroid-Stimulating Hormone (TSH) by the anterior pituitary gland. TSH is transported to the thyroid gland, which stimulates the production of T4 and T3 by the thyroid gland [2].
• And their normal serum range are Triiodothyronine/T3/ = 70-90 ng/dL, Thyroxine/T4/ = 5.0-12.0 ug/dl, and TSH = <10 μU/ml.
• T3 is less firmly bound to carrier proteins and disappears from circulation quicker and also T3 is 3-5 times as potent as T4 but is limited by its transient nature Figure 2.
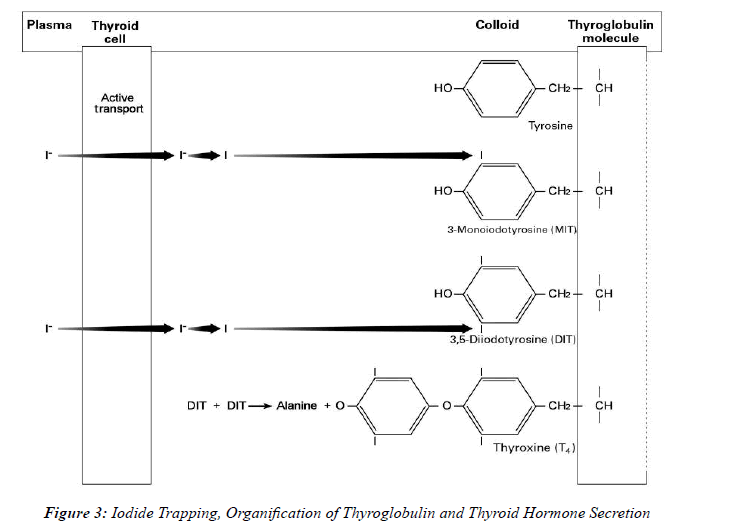
• After iodide is orally ingested and absorbed by the gastrointestinal tract into the blood, thyroid hormone synthesis starts when iodide is actively transported from the plasma into the colloid of the follicle. Once transported to inside the follicle, iodide is converted to iodine by thyroid peroxidase. This process is known as iodide trapping.
• This process implies that Iodine in pharmacologic doses (Lugol’s solution, 5% iodine, 10% potassium iodide in water) inhibits the release of T3 and T4 for a limited time (days to weeks) after which its antithyroid activity is lost Figure 3.
Thyroid Pathophysiology, Indications for Surgery and Their Anesthetic Implication
The indications for thyroid surgery include: thyroid malignancy, goitres that produce obstructive symptoms and/or are retrosternal; hyperthyroidism which are usually resistant to medical management; cosmetic and anxiety related reasons. Patients with hypothyroidism usually used to respond for thyroxine therapy and surgery is rarely indicated [3].
Malignancy
These will most commonly present as thyroid nodules and are usually minimally active biochemically (patient is euthyroid). The most common types are Papillary and Follicular carcinomas arising from the epithelium that confer a good prognosis if adhered to the gland. Medullary carcinomas arising from calcitonin producing cells are associated with Multiple Endocrine Neoplasia (MEN), which may be associated with phaeochromocytoma and primary hyperparathyroidism. Lymphomas cause diffuse swelling of the gland and carry a very poor prognosis.
• More than 90% of thyroid nodules are benign, yet identifying malignancy in a solitary thyroid nodule is a difficult and important procedure.
• Male patients and patients with history of previous radiation therapy to the head and neck have an increased risk of malignant disease in their nodules. Follicular carcinoma accounts for about 15% of thyroid carcinomas, is more aggressive, and has usually poor prognosis [4].
Hyperthyroidism
Hyperthyroidism results from excess circulating T3 and T4. The vast majority of cases are caused by intrinsic thyroid disease. Common causes include:
1. Grave’s disease: An autoimmune condition associated with diffuse enlargement and increased vascularity of the gland caused by IgG antibodies mimicking Thyroid Stimulating Hormone (TSH). It is the only cause of hyperthyroidism associated with eye signs/ exophthalmos/ and pretibial myxedema. It can be associated with other autoimmune conditions.
2. Thyroid secreting adenomas often presenting as a solitary nodule.
3. Toxic Multinodular Goitre. More common in women; a goitre develops one or two nodules with hyper secretory activity.
4. Other causes which may or may not be associated with goitre include: Exogenous iodine, Amiodarone, Post irradiation thyroiditis. In this group, medical management has proved unsatisfactory and radioiodine is not suitable [5].
• Major manifestations of hyperthyroidism are weight loss, diarrhea, and warm moist skin, weakness of large muscle groups, menstrual abnormalities, osteopenia, nervousness, alertness, and intolerance to heat, tachycardia, cardiac arrhythmias, mitral valve prolapse, and heart failure. When the thyroid is functioning abnormally, the entity most threatened is the cardiovascular system. When diarrhea is severe, dehydration should be corrected preoperatively.
• In the sever form of hyperthyroidism muscle disease usually involves the proximal muscle groups. But it has not been described on papers I reviewed to cause respiratory muscle paralysis which is most commonly seen in persons older than 60 years [6].
Hypothyroidism
May be from intrinsic thyroid disease (primary hypothyroidism) or failure of the hypothalamic-pituitary axis (secondary hypothyroidism). Those associated with goitre include:
1. Hashimoto’s thyroiditis: This is the most common cause of hypothyroidism and although initially may cause gland enlargement will later lead to thyroid atrophy due to autoantibody destruction of the follicles.
2. Iodine deficiency: A lack of iodine leads to thyroid hormone depletion, Thyroid Stimulating Hormone (TSH) stimulation and gland hypertrophy. Dietary iodine deficiency is usually found in mountainous areas [7].
• The apathy and lethargy that often accompany hypothyroidism frequently delay its diagnosis, so the perioperative period may be the first opportunity to spot many such hypothyroid patients concurrently.
• Hypothyroidism is usually subclinical, serum values of thyroid hormones are in the normal range, and only serum TSH levels are elevated. The normal range of TSH is 0.3 to 4.5 mU/L, and TSH values of 5 to 15 mU/L are characteristic of this entity. In such cases, hypothyroidism may have little or no perioperative significance.
Discussion
Preoperative Assessment and Optimization
History
The primary goals of the preoperative assessment are ensuring that the patient is in euthyroid condition, assessing the degree of end-organ complications, and determining the extent of airway involvement, it is important to establish the pathological nature, position and size of the goitre to appreciate the complexity and potential complications that may occur. A large goitre that has been present for some time may be associated with tracheomalacia postoperatively. Symptoms of dysphagia, positional breathlessness with a difficulty lying flat, change in voice or stridor may alert the anesthetists to possible difficulties with airway compromise while on induction. Evidence of other systemic disease, cardiorespiratory compromise and associated endocrine or autoimmune disorders should also be considered. For example, medullary thyroid cancer associated with phaeochromocytoma [8].
Examination
The patient should be clinically euthyroid before surgery. Tachycardia, atrial fibrillation and dysrhythmias should be excluded by assessment of the resting pulse rate. The patient should be assessed for signs of hyperthyroidism or hypothyroidism with a thorough examination of the goiter or nodule and should be performed to assess size and extent of the lesion.
A fixed hard nodule suggests malignancy with possible adhering to surrounding structures and limited movement. An inability to feel the bottom of the goitre may indicate retrosternal extension [9].
The trachea should be examined to check for any deviation or compression. Retrosternal or large goitres can compress surrounding structures and may elicit signs of Superior Vena Cava (SVC) obstruction, Horner’s Syndrome, pericardial or pleural effusions. A mandatory detailed airway examination would also include assessment of atlantoaxial flexion and extension, thyromental distance, Mallampatti, mandibular protrusion or jaw slide and incisor distance [10].
Anti-Thyroid Medication Regimens
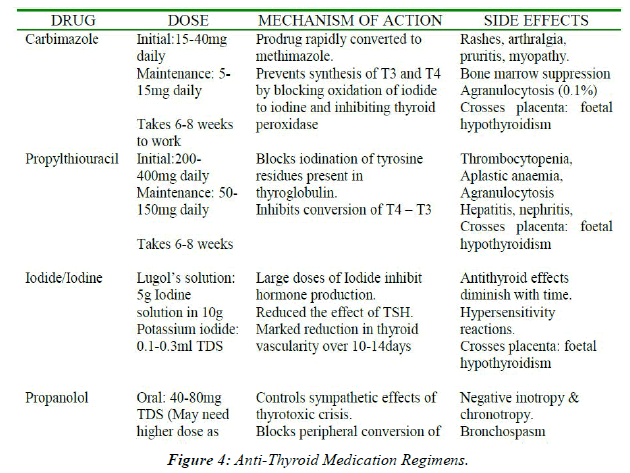
• The usual initial medical management regimens like Propylthiouracil, carbimazole, methimazole inhibit synthesis of inorganic iodide and coupling of iodothyronines.
• Graves’ disease often initially treated with anti-thyroid drugs in hope of inducing a remission or achieving euthyroidism before surgery.
• Pregnant females should be treated with propylthiouracil (of antithyroid drugs because it crosses placenta the least), minimizing the risk of goiter any hypothyroidism in fetus Figure 4.
• Intraoperative bleeding, from drug-induced thrombocytopenia or hypoprothrombinemia has been reported in patients on propylthiouracil [11].
• Hypothyroidism is a risk of antithyroid drugs so patient may receive supplemental T4.
• Beta-Adrenergic Antagonists are also useful adjunctive therapies for patients with Graves’ disease diminish some of the S/S (tachycardia, anxiety, and tremor) more rapidly than can antithyroid drugs.
• Nadolol and atenolol have a longer duration than propranolol and also these drugs do not block the synthesis and secretion of thyroid hormones Figure 4.
General Categories and Thyroid Laboratory investigations
Five General Categories
1. Direct tests of thyroid function; Thyroid Radioactive Iodine Uptake (RAIU) is measured 24 hours after administration of isotope. Normal is 10-30% of administered dose after 24 hours values but above normal indicate thyroid hyper function.
2. Tests relating to the concentration and binding of thyroid hormones in blood; by using highly specific and sensitive radioimmunoassay to measure serum T3 and T4, highly sensitive TSH assay is the most sensitive of thyroid function.
3. Metabolic indexes; Measurements of oxygen consumption in the BMR has been used as a mainstay in the diagnosis of thyroid disease, but not today [12].
4. Tests of homeostatic control of thyroid function; these are
a. Basal serum TSH concentration b. Thyrotropin-releasing hormone c. Thyroid suppression test
5. Miscellaneous tests; these tests do not assess thyroid function but are if value in defining the nature of the thyroid disorder or in planning therapy.
Routine investigations
Blood tests: A routine blood tests include Full Blood Count, electrolytes, thyroid function tests and corrected calcium levels. It is imperative to ensure the patient is euthyroid prior to surgery to avoid perioperative complications of a thyroid storm or myxedema coma. FBC is essential due to the potential for blood loss during the procedure plus to detect any serious adverse hematological effects of concurrent antithyroid medications or drug reactions.
A CXR may be useful to assess the size of goiter, detect any tracheal compression or deviation, retrosternal extension and the trachea anteroposterior diameter. If there are any concerns regarding airway compromise or DEI, a CT scan is performed to determine the extent and location of tracheal narrowing or detect tracheal invasion [13].
Some Important Surgical Considerations
Thyroidectomy is performed through a transverse incision at the base of the neck. After the thyroid gland is exposed, resection can proceed. Resection may be total, subtotal (lobe + isthmus ± partial remaining lobe), or lobar. Degree of resection depends on diagnosis and may be modified based on operative findings. During this portion of the operation, hemostasis is critical to maintain adequate visualization and the resection of a lobe usually begins with ligation of the middle thyroid veins along the bilateral aspects of the thyroid.
Special care must be taken medially along the trachealesophageal groove to prevent damage to the recurrent laryngeal nerve which is most common nerve injury from damage to abductor fibers of recurrent laryngeal which is more discussed on post op complications part of the essay. As soon as the gland is mobilized to the degree that it is only adherent to the trachea, it may be fully resected using a knife to prevent cautery injury to the trachea. The use of drains remains controversial and has not been shown to decrease the rate of hematoma formation [14].
Anesthetic technique: RA/GA
Historically thyroid surgery was performed under local anesthesia. General anesthesia is now the preferred technique but regional anesthesia can still have a place either as a sole technique with or without sedation or alongside general anesthesia to enhance analgesia.
Regional Anesthesia
Regional anesthesia for thyroid surgery is seldom used in the developed countries but it has not been successfully employed as the sole anesthetic technique particularly in areas with limited resources.
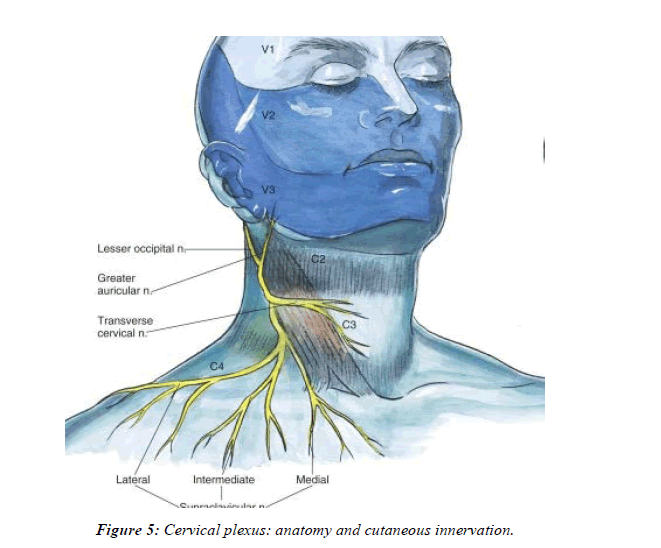
To achieve the most successful results a multidisciplinary team approach needs to be employed with appropriate patient selection, excellent patient education and modification of surgical technique. Surgical anesthesia can be achieved using deep and bilateral C2-C4 cervical plexus blocks, with or without sedation under full monitoring.
Conscious sedation can be achieved by increments of Midazolam or a Target Controlled Infusion (TCI) of Propofol. Patients who cannot communicate verbally with the surgical and anesthetic team, or who are obese, are unlikely to be good candidates for this technique. Regional anesthesia avoids the risks of a general anesthetic, allows intraoperative voice monitoring and moreover it provides excellent postoperative analgesia [15]. The technique may be suited to medically compromised patients (including complicating thyrotoxicosis), or those with obstructive symptoms secondary to large goitres to avoid the risks of a general anesthetic. However, these techniques do have a number of complications including local anesthetic toxicity, hematoma, pneumothorax, and require excellent patient cooperation.
Superficial Cervical Plexus Block
The nerves supplying the anterolateral part of the neck emerge from the posterior border of sternocleidomastoid (SCM) as the anterior rami of C2-C4, which branched into greater auricular, transverse cervical, lesser occipital and supraclavicular nerves.
To perform the superficial cervical plexus block, the patient should be positioned with their head extended to the opposite side, the midpoint of the posterior border of SCM visualized. 10-20mls of local anesthetic is injected in a superficial, wheal deep to the first fascial layer in caudad and cephalad directions along the posterior border of SCM. For thyroidectomy, bilateral blocks should be performed. A midline field block can be achieved by a subcutaneous filtration, starting from the thyroid cartilage to the suprasternal notch. This is a useful adjuvant to prevent the pain from surgical retractors on the medial aspect of the neck [16].
Bilateral deep cervical plexus blocks have a higher incidence of complications including inadvertent vertebral artery and subdural injection, and notably bilateral phrenic nerve palsy, which may not be tolerated and painful in some patients Figure 5.
General Anesthesia
Intraoperative anesthetic management should focus on the prevention of sympathetic nervous system stimulation, proper positioning, and adequate hemodynamic monitoring. And the majority of cases are straightforward even when imaging suggests significant degrees of tracheal deviation or compression.
Induction
Full pre-oxygenation (5-6 mins) should precede i.e. induction and muscle relaxation with a neuromuscular blocking drug, once manual ventilation has been demonstrated.
Normally, GETA with pre-operative superficial cervical plexus block if anatomy allows and infrequently with prior local anesthesia subcutaneous infiltration. For inadequately treated hyperthyroid patients, it is important to achieve an adequate depth of anesthesia to prevent an exaggerated sympathetic response to surgical stimulation. Standard induction for euthyroid patients. If the patient has high risk of airway compromise 2° a large thyroid goiter, consider an awake fiber optic intubation.
We need to avoid agents that stimulate the sympathetic nervous system (Example: ketamine, pancuronium even if with no significant instability, meperidine) [17]. Hypothyroidism may be associated with ↑ sensitivity to anesthetic agents and muscle relaxants.
Positioning
The patient is positioned supine with the head elevated 30° to prevent venous engorgement and the neck extended by using a roll behind the neck and shoulders (Rose position) or with the head extended and stabilized using a head ring and sandbag between the scapulae.
The arms are tucked at patient’s sides with the ulnar nerves padded and protected, hyperextension of the neck should also be avoided in patients with atlantoaxial joint instability and in patients with limited range of motion. Due to the limited access to the face, special care should be taken to protect the eyes from injury, especially in patients with exophthalmos.
Difficult Tracheal Intubation in Thyroid Surgery
The anesthetists should expect that about 6% of tracheal intubations for thyroid surgery will probably be difficult. Some of the studies I tried to review conclude that a large goitre is not associated with a more frequent DEI. However, the presence of a cancerous goitre is a major factor predicting DEI caused by tracheal invasion and tissue infiltration by the carcinoma associated with fibrosis that may reduce the mobility of laryngeal structures and make the laryngoscope view more difficult. Whenever supposing that the airway will be lost if anesthesia is induced and anticipation of DEI, awake fibreoptic intubation is the method of choice.
If preoperative assessment has increased concerns regarding the airway, the following options should be considered:
1. Inhalational /gaseous/ induction.
2. An awake fibreoptic intubation may be used. This technique should be avoided in those patients with marked symptoms of airway obstruction as complete obstruction may be provoked.
3. If either of these options is not suitable, a tracheostomy under local anesthetic by the surgeons may be appropriate.
4. Ventilation through a rigid bronchoscope can be used if attempts at passing an endotracheal tube fail or if there is subglottic tracheal compression.
5. The Laryngeal Mask Airway (LMA) can be used for thyroid surgery but should be avoided in those with airway compromise or distorted anatomy [18].
Maintenance
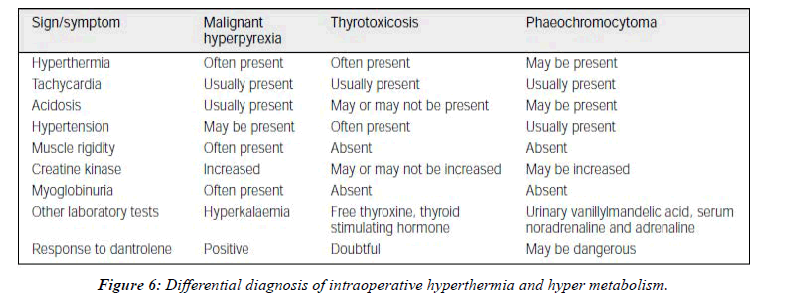
The patient should be constantly monitored for an increase in core body temperature and a homodynamic response. All sympathomimetic agents should be avoided, if hypotension occurs, it is best treated with a direct acting vasopressor. Isoflurane, desflurane, sevoflurane, are good as they offset adverse sympathetic nervous system responses to surgical stimulation, but do not sensitize the heart to catecholamine. Hypercarbia and hypoxia are potent stimulators of the sympatho-adrenal axis; therefore, adequate inspired oxygen concentration ratio and minute ventilations should be maintained. Figure 6.
Management of Thyroid Storm
Thyroid storm is characterized by hyperpyrexia, tachycardia, altered consciousness and hypotension this is a medical emergency which can occur intraop but is more likely to occur 16-18 hours postoperatively. Although less commonly seen now as patients are rendered euthyroid prior to surgery it can still occur in patients with hyperthyroidism when they sustain a reflex acute stress response such as surgery or infection. Management is usually supportive with active cooling, hydration, beta blockers and anti-thyroid drugs. Dantrolene 1mg/kg has also been successfully used in the treatment of thyroid storm. Propranolol does not prevent thyroid storm.
Analgesia
Multi modal analgesia or regular paracetamol, non-steroidal anti-inflammatories (NSAIDs) plus weak opioids are usually adequate to ensure the patient is comfortable preoperatively. Local anesthetic with adrenaline infiltration subcutaneously prior to incision is also recommended for having some analgesic effect into the postoperative period. Bilateral superficial cervical plexus blocks can significantly reduce pain and opioid requirements in the postoperative period. Administration of antiemetic’s prophylaxis is important as these patients are at high risk of postoperative nausea and vomiting. A combination of ondansetron and/or cyclizine with dexamethasone, which may also help reduce postoperative airway edema, can be used.
Postoperative Complications and Management
The most common postoperative complications include hypocalcemia, RLN damage, and hematoma at the surgical site in addition the potential postoperative complications associated with thyroidectomy include.
Hemorrhage
Postoperative bleeding can cause respiratory compression and rapid airway obstruction. Signs of swelling or hematoma formation which is compromising the patient’s airway should be immediately decompressed by removal of surgical clips. Clip removers or forceps should be kept by the patient’s bedside. If there is time to return to theatre, reintubation should also be performed early.
Laryngeal oedema
This can cause of postoperative respiratory obstruction. It may occur as a result of traumatic tracheal intubation or in those who develop a hematoma that can cause obstruction to venous drainage. It can usually be managed with steroids, humidified oxygen and re intubation if necessary.
Recurrent Laryngeal Nerve (RLN) Palsy
Trauma to the recurrent laryngeal nerve can be caused by ischemia, traction, entrapment or transaction of the nerve during surgery and may be unilateral or bilateral; the cords can collapse together, producing total airway obstruction during inspiration.
Unilateral vocal cord palsy will present with respiratory difficulty, hoarse voice or difficulty in phonation whilst bilateral palsy will result in complete adduction of the cords and stridor. Bilateral RLN palsy requires immediate reintubation and the patient may subsequently need a tracheostomy, Selective injury of adductor fibers of recurrent laryngeal nerves leaves the adductor fibers unopposed and pulmonary aspiration a hazard.
Hypocalcaemia
Unintended trauma to the parathyroid glands may result in temporary hypocalcaemia, if this occurs, hypocalcemia typically develops 24 to 72 hours postop, but may manifest as early as 1-3 hours postop. Laryngeal muscles sensitive to hypocalcemia may go from inspiratory stridor progressing to laryngospasm, but permanent hypocalcaemia is rare. Signs of hypocalcaemia may include confusion, twitching and tetany. This can be elicited in Trousseau’s (carpopedal spasm precipitated by cuff inflation) or Chvostek’s sign (facial twitch on tapping parotid gland), IV Calcium replacement should be instituted immediately since hypocalcaemia can precipitate laryngospasm, cardiac irritability, QT segment prolongation and subsequent arrhythmias.
Tracheomalacia
The possibility of tracheomalacia should be considered in those patients who have had sustained tracheal compression by large goitres or tumors, airway obstruction that occurs soon after tracheal extubating, despite normal vocal cord function, as so these signs highly suggest tracheomalacia. And this phenomenon reflects a weakening of tracheal rings by chronic pressure of a goiter, a cuff leak test just prior to extubating is reassuring but equipment should be available for immediate reintubation if it occurs.
Perioperative Management of Thyrotoxic Patients for Non-thyroid or Emergency Surgery
Thyrotoxic patients may require non-thyroid surgery for other medical reasons which are not related to their thyroid disease. These are more likely to be urgent or emergent surgeries in patients who either have already been treated for their thyroid condition but not yet become euthyroid or who have not yet been diagnosed or treated before the development of another urgent medical complication. Elective surgery should always be postponed until the patient has become clinically and biochemically euthyroid and stable. Perioperative control of thyrotoxicosis may prove challenging in acutely ill patients, usually requiring combined therapy or less than optimal control.
Rapid preparation
Rapid preoperative preparation usually within one hour may be needed for patients requiring urgent or emergent surgery. Truly emergent cases still may benefit from the initiation of Safe and effective oral therapy with a combination of b-blockers (propranolol 40 mg every 8 hours) or Esmolol 100-300 mcg/kg/min IV if available until heart rate<100/ min, and high dose glucocorticoids (betamethasone 0.5 mg or dexamethasone 4mg in our set up every 6 hours).
Conclusion
The primary goals of the preoperative assessment are ensuring that the patient is in euthyroid condition, assessing the degree of end-organ complications, and determining the extent of airway involvement, it is important to establish the pathological nature, position and size of the goitre to appreciate the complexity and potential complications that may occur. A large goitre that has been present for some time may be associated with tracheomalacia postoperatively. Symptoms of dysphagia, positional breathlessness with a difficulty lying flat, change in voice or stridor may alert the anesthetists to possible difficulties with airway compromise while on induction. Evidence of other systemic disease, cardiorespiratory compromise and associated endocrine or autoimmune disorders should also be considered. For example, medullary thyroid cancer associated with phaeochromocytoma. The patient should be clinically euthyroid before surgery. Tachycardia, atrial fibrillation and dysrhythmias should be excluded by assessment of the resting pulse rate. The patient should be assessed for signs of hyperthyroidism or hypothyroidism with a thorough examination of the goiter or nodule and should be performed to assess size and extent of the lesion.
The trachea should be examined to check for any deviation or compression retrosternal or large goitres can compress surrounding structures and may elicit signs of superior vena cava (SVC) obstruction, Horner’s Syndrome, pericardial or pleural effusions, a fixed hard nodule suggests malignancy with possible adhering to surrounding structures and limited movement. An inability to feel the bottom of the goitre may indicate retrosternal extension. A mandatory detailed airway examination would also include assessment of atlantoaxial flexion and extension, thyromental distance, Mallampatti, mandibular protrusion or jaw slide and incisor distance. The patient should be constantly monitored for an increase in core body temperature and a homodynamic response, all sympathomimetic agents and other physiologic alterations which have potential of stimulating of the sympathoadrenal axis should be better to be avoided. In addition to multi modal analgesia or up to that of level III on WHO ladder by adding opioids, bilateral superficial cervical plexus blocks can significantly reduce pain and strong opioid requirements in the postoperative period. Administration of antiemetic’s prophylaxis is important as these patients are at high risk of postoperative nausea and vomiting. Finally good postoperative full information handover, even routine follow up by we ourselves, and early recognition of those common postoperative complications discussed before are the corner stone of post-operative quality management to intervene acute life threatening conditions and avoiding further exacerbation of the event.
References
- Hall JE, Guyton AC. Thyroid metabolic hormones. Textbook of medical physiology. 2016;951-63.
- Kiefer JE, Mythen MO, Roizen MF, et al. Anesthetic implications of concurrent diseases. Miller's Anesthesia. 2020; 9th ed. Philadelphia, PA: Elsevier.
- Karlet MC, Fort DM. The endocrine system and anesthesia. Nagelhout J, Plaus K. Nurse Anesthesia. 5th ed. St. Louis, MO: Elsevier. 2014; 840-79.
- Eriksson M, Rubenfeld S, Garber AJ, et al. Propranolol does not prevent thyroid storm. N Engl J Med. 1977; 296(5):263-4.
- Bilezikian JP, Loeb JN. The influence of hyperthyroidism and hypothyroidism on α and β-adrenergic receptor systems and adrenergic responsiveness. Endocrine reviews. 1983; 4(4):378-88.
- Malhotra S, Sodhi V. Anaesthesia for thyroid and parathyroid surgery. Continuing Education in Anaesthesia, Critical Care and Pain. 2007; 7(2):55-8.
- Spanknebel K, Chabot JA, DiGiorgi M, et al. Thyroidectomy using local anesthesia: a report of 1,025 cases over 16 years. J Am Coll Surg. 2005; 201(3):375-85.
- Aunac S, Carlier M, Singelyn F, et al. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg. 2002; 95(3):746-50.
- Weglinski MR, Wedel DJ. Differential diagnosis of hyperthermia during anesthesia and clinical import. Anesthesiology Clinics of North America. 1994; 12(3):475-89.
- Sessler DI. Malignant Hyperthermia—Update. West J Med. 1988; 149(1):76.
- Stoelting RK, Dierdorf SF. Anesthesia and co-existing disease. 2002.
- Kerridge R, Lee A, Latchford E, et al. The perioperative system: a new approach to managing elective surgery. Anaesth. 1995; 23(5):591-6.
- Ingbar SH. IX. Thyrotoxic storm. N Engl J Med. 1966; 274(22):1252-4.
- Stehling LC. Anesthetic management of the patient with hyperthyroidism. The Journal of the American Society of Anesthesiologists. 1974; 41(6):585-95.
- Jaffe RA, Schmiesing CA, Golianu B. Anesthesiologist's manual of surgical procedures. Lippincott Williams & Wilkins; 2014.
- Jameson JL. Disorders of the thyroid gland. Harrison's principles of internal medicine. 2005; 2104-13.
- Fewins J, Simpson CB, Miller FR. Complications of thyroid and parathyroid surgery. Otolaryngol Clin North Am. 2003; 36(1):189-206.
- Farling PA. Thyroid disease. Br J Anaesth. 2000; 85(1):15-28.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref