Review Article - Biomedical Research (2022) Volume 33, Issue 3
A review on novel approach ethosome as a nanocarrier for transdermal drug delivery
Sunayana Tyagi1*, Lovely Chaurasia2, Mojahidul Islam3, Bhumika Sagar4, Anushka Tyagi5
1IIMT College of Medical Science, Meerut 250001, Uttar Pradesh, India
2Department of Pharmaceutics, IIMT College of Medical Science, Meerut 250001, Uttar Pradesh, India
3Department of Pharmaceutical Chemistry, IIMT College of Medical Science, Meerut 250001, Uttar Pradesh, India
4Department of Pharmacology, IIMT College of Medical Science, Meerut 250001, Uttar Pradesh, India
5Department of Pharmaceutics, Amity University, Noida, Uttar Pradesh, India
- Corresponding Author:
- Sunayana Tyagi
Assistant professor
IIMT College of Medical Sciences
Meerut
India
Accepted date: March 11, 2022
Abstract
The skin is one of the most broad and promptly open organs of the human Body. Perhaps the best impediment to transdermal medication conveyance is the skin's low penetrability that restricts the quantity of medications that can be conveyed thusly. Ethosomes as original vesicles in transdermal medication conveyance show critical impacts on drug infiltration through the natural layer. Present days we better known vesicles have significance in cell correspondence. Ethosomes, although ethosomes are theoretically refined, they are basic in preparation and better for use. Transdermal course is promising choice to sedate conveyance for foundational impact. An endeavor was made to plan the exceptionally effective ethosomal drug conveyance framework and enalapril meleate is utilized as model medication. Ethosomes have higher infiltration rate through the skin when contrasted with liposomes henceforth these can be utilized generally instead of liposomes. Ethosomes upgraded skin penetration, further developed medication conveyance, expanded medication entanglement proficiency and so on Ethosomes have turned into a space of examination interest, as a result of its improved skin pervasion, further developed medication conveyance, expanded medication capture productivity and so forth The motivation behind composing this survey on ethosomes drug conveyance was to incorporate the attention on the different parts of ethosomes including their instrument of entrance, arrangement, benefits, structure, portrayal, application and advertised result of ethosomes. Portrayals of ethosomes incorporate particle size, zeta potential, differential scanning calorimertry, entrapment effectiveness, surface strain movement estimation, vesicle steadiness and penetration studies.
Keywords
Transdermal drug delivery system, Ethosomes, Drug absorption.
Introduction of Skin
The largest organ in the body is skin. It does not have a uniform thickness. It is not uniformly thick. It measures approximately 5 mm thick in the area between the foot and the interscapular. The skin is thin in all other parts of the body. It is thinner around the eyelids and penis, measuring approximately 0.5 mm.
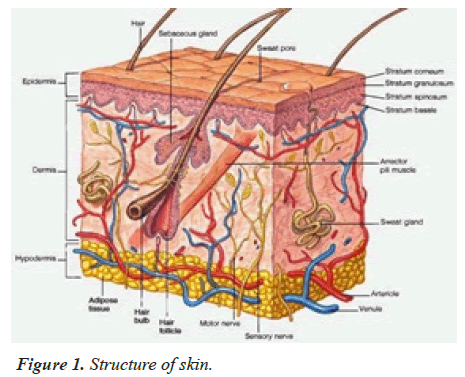
The skin is one of eminently overall and fluently smooth organs of the human body and the skin as a route of drug delivery can offer successive advantages over traditional drug delivery systems including under values change in plasma drug levels, avoidance of gastrointestinal disturbances and first-pass metabolism of the drugs, and high chumps compliance [1,2]. To regulate the permeation of drugs around the skin various mechanisms empower have being marked, including use of substitute or spiritual enhancers, for instance iontophoresis, sonophoresis, etc. A transdermal delivery of drugs and vaccines is an effective alternative to oral and parenteral routes of administration [3-6]. closely monitored intravenous infusion can provide the advantages of both direct entry of drug into the supplemental circulation and control of dispensation drug levels recently, it is necessary evident that the benefits of intravenous drug infusion conceivably closely duplicated, without its hazards, by work the skin as the port of drug the use of lipid vesicles in delivery systems for the skin healing forget attracted increasing attention recent years. However, it is generally agreed that classic liposomes are of little or no esteems as carriers for transdermal drug delivery because they do not awful penetrate the skin, but more or less remain upper layer of the stratum corneum. Only particular vesicles were shown to have the means for allow transdermal delivery ethanol is known as an efficient permeation enhancer. However, by reason of the interdigitation effect of ethanol on lipid bilayers, it was commonly noted that vesicles cannot coexist with high concentrations of ethanol. Forth with, ethanol can only be relatively low concentrations in liposome formulations (Figure 1).
Factors that affect skin penetration
Different factors affect the penetration of substances through skin.
1. Age Penetration in infants and children is higher than in adults.
2. Skin Condition More penetration occurs on damaged or abraded skin.
3. Hydration for the skin: Penetration in dry skin is greater than in hydrated skin.
4. The epidermis's fat content has little effect on penetration.
Types of vehicles
Hyperemia: Vasodilation of blood vessels in response different stimuli, either localized or generalized, increases the penetration.
a. Vasoconstriction was used for corticosteroids.
b. Vasodilation of nicotinates
c. Whealing to histamines.
d. Sweating with pilocarpine
e. Anesthesia to local anesthetics
Transport mechanism
Passive diffusion is the main process of drug absorption into the skin. The following equation shows the drug flux after passive diffusion.
J=DPAC/h
Where J is the steady state flux across the stratum corneum, D is the diffusion coefficient/diffusivity of drug molecule (cm2/sec), C is the concentration gradient across the stratum corenum (g/cm3), P is the partition coefficient of drug between skin and formulation, h is the thickness of stratum corenum (cm), A is the surface area of stratum corenum (cm2). This equation states that drug passage rates are directly proportional with drug's aqueous solubility. It is also proportional to drug formulation concentration, oil/water partition coefficient, and skin surface area. The reality is that the drug concentrations on the receiver sides are low due to the continuous blood flow. P M represents the permeability constant and C is the concentration.
Transdermal drug delivery
Transdermal drug delivery through the skin is the most efficient and convenient method of drug delivery. The skin acts as both a target and a barrier to this transdermal/ topical drug delivery. This system has many benefits, but the main obstacle is the slow diffusion rate of drugs through the stratum corneum. However, the vesicular systems penetrate the skin to exert their actions. The most effective vesicular system is the ethosomes, which can penetrate the skin well.
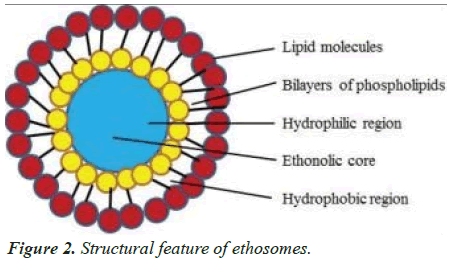
Ethosomes contain liquid vesicles that are releatively rich in alcohol (ethanol, and/or isopropyl alcohol) and phospholipids. Ethosomes can be described as soft vesicles that contain phospholipids, ethanol (in greater quantity) and water. Ethosomes can range in size from a few nanometers up to a few microns.
The skin's barrier function limits transdermal drug administration. There have been many attempts to temporarily increase drug permeation rates. There are many ways to temporarily increase the drug's permeation rate. High levels of ethanol can cause a decrease in the fluidity of lipids, which in turn increases drug penetration and permeability. It is possible that ethosomal formulations will be more effective in dermal/transdermal delivery. Ethosomes are liquid vesicles containing phospholipid, alcohol (ethanol and/or isopropyl alcohol) in releatively high concentration and water. Ethosomes are soft vesicles made of phospholipids and ethanol (in high quantity) and water. Ethosomes can range in size from a few nanometers to microns. The ethosomes are vesicular carrier comprise of hydroalcoholic or hydro/alcoholic/glycolic phospholipid in which the concentration of alcohols or their combination is releatively high. Typically, ethosomes may contain phospholipids with various chemical structures like Phosphatidylcholine (PC), hydrogeneated PC, Phosphatidic Acid (PA), Phosphatidylserine (PS), Phosphatidylethanollamine (PE), Phosphatidyglycerol (PPG), Phosphhatidylinositol (PI), hydrogeneated PC, alcohol (ethanol or isopropyl alcohol), water and propylene glycol (or other glycols).
This composition allows for high levels of active ingredients to be delivered through the skin. Modifying the Alcohol: Water or Alcohol-Polyol/Water ratio can alter drug delivery. Soya phospholipids like phospholipon 90 (PL-90) are some of the most preferred phospholipids. It is typically used in a range between 0.5%-1% w/w. The prepration can also contain cholesterol at levels between 0.1%-1%. You can use ethanol or isopropyl alcohol as examples of alcohols. Propylene glycol, Transcutol and other glycols are common. In addition, non-ionic surfactants (PEG-alkyl ethers) can be combined with the phospholipids in these preparations. Cationic lipids like coco amide, POE alkyl amines, dodecylamine, cetrimide etc. You can also add alcohol. The final product can have a concentration of alcohol between 20% and 50%. The non-aqueous phase (alcohol and glycol combination), may have a concentration between 22% and 70%.
Transdermal delivery is one of the most popular methods for delivering therapeutic substances to the skin. This means that the skin can be used for systemic effects. Percutaneous delivery is closely related. It is transport into the target tissues with an effort to avoid systemic side effects. Transdermal drug delivery systems are topically administered drugs in the form gels or patches. They deliver drugs to systemic effects at a predetermined, controlled rate.
The epidermis and dermis are the two most important layers of skin. The epidermis is the outermost layer of skin. It measures approximately 100-150 micrometers thick and has no blood flow. It also includes the stratum corneum, which is a series of layers. Because of its unique composition, this layer is crucial for transdermal delivery. It keeps water in the body and prevents foreign substances from getting out. The dermis is located beneath the epidermis and contains the capillaries that transport blood throughout your body. The drug can be absorbed into the bloodstream if it is able to penetrate the stratum creneum. Passive diffusion, which is too slow for practical use, allows normal drugs to cross this layer. This can be circumvented by making the drugs both water-soluble as well as lipid soluble. This is because "Lipid-soluble substances readily pass through the intercellular lipid bilayers of the cell membranes whereas water-soluble drugs are able to pass through the skin because of hydrated intracellular proteins". This allows for much faster and more effective drug delivery [7].
Introduction of Ethosome
The size of ethosomes is adjustable from a few microns to a few nanometers. Permeation Enhancers increase the skin's permeability so that drugs can pass through the skin easily. 7-depending on the size of the body, the dermis is between 10-40 fold thicker than the epidermis. It is composed of loose connective tissue and polysaccharides, as well as protein (collagen or elastin), and is metabolically less active than epidermis. It contains nerves and blood vessels, as well as hair follicles, sweat glands 7 and sebaceous glands 7. The dermis also contains macrophages and leukocytes as well as mast cells and macrophages. The dermis serves two functions: to nourish the epidermis, and to anchor it to subcutaneous tissue. The subcutaneous tissue is a container for fat storage and formation. It is a heat regulator as well as a shock absorber [8,9] (Figure 2).
Advantages
• GIT degrading, poor oral absorption, and bioavailability.
• It has a higher drug penetration and a greater systemic effect.
• It is made from non-toxic raw materials.
• High patient compliance.
• The ethosomal drug comes in semisolid form (gel, cream), which results in high patient compliance.
• The Ethosomal system can be immediately commercialized as it is non-invasive, passive and non-Invasive.
• Ethososomes have a higher drug entrapment efficiency, decreased side effects and constant systemic levels.
• Significant skin accumulation of the drug.
• Ethosomes allow for enhanced drug penetration through the skin, allowing transdermal or dermal delivery [10].
Disadvantage of ethosomes
• Drugs with high blood levels can't be administered. This is limited to drugs that have a potent molecule and require a daily dose of 10 mg.
• Drug should be able to dissolve in both lipophilic as well as aqueous environments.
• This will allow the drug to reach the dermal microcirculation and be absorbed percutaneously.
• May not have a low yield.
• Excipients and enhancers for drug delivery systems can cause skin irritations or dermatitis.
• The main advantage of ethosomes in comparison to liposomes is their increased drug penetration.
• Product loss during the transfer from organic to liquid media [11].
Basic components
The basic components of transdermal devices are:
• The polymer matrix (or matrices)
• Drug
• Drug permeation enhancers
• Other excipients [12]
Mechanism of drugs pentration
Two phases are required to understand the mechanism of drug absorption.
1. Ethanol effect
2. Ethosomes effects
Ethanol effect
Ethanol penetrates into intercellular Lipids and increases the fluidity of cell membrane Lipids. It also decreases the density of multilayer Lipids in cells [13].
Ethosome effect
The Ethanol of Ethosomes results in an increase in cell membrane lipid fluidity and increased skin permeability. The Ethosomes penetrate very easily into the deep skin layers, where it fuses with Skin Lipids and releases the drugs to the Deep Layer of Skin [14].
Method of Preparation
Convenient methods that are
• Cold Method
• Hot Method
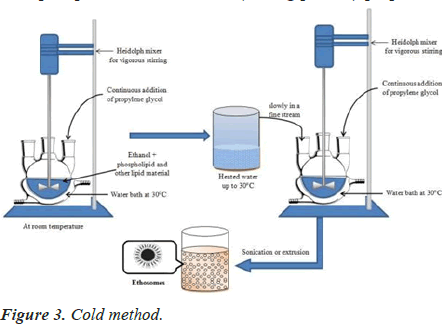
Cold method
This is the most commonly used method for the preparation of an ethosomal formulation. The mixture is heated in a water bath to 300 ºC. Add the water to the mixture in separate vessels. The mixture is stirred for 5 minutes in a covered vessel. You can reduce the size of the vesicles by using either extrusion or sonication. Final, the formulation should be stored under refrigeration [15,16] (Figure 3).
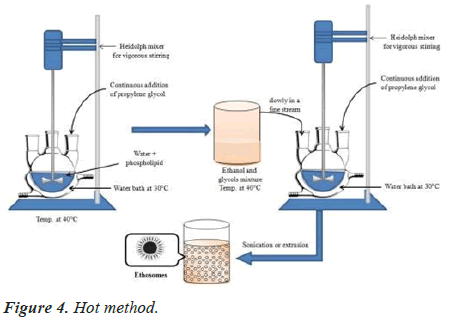
Hot method
This involves dispersing the phospholipid in water at 40ºC for a few minutes until you get a colloidal solution. Glycols and ethanol are heated to 40ºC in a separate vessel. The organic phase is added to aqueous phase as soon as the mixture reaches 40ºC. This is a very similar procedure to the cold method [17,18] (Figure 4).
Evaluation of ethosomes
Scanning electron microscopy: This studies the interaction between filter membrane vesicles and scanning electron microscopy. The procedure involves the application of vesicle suspension (0.25 mL) onto a filter membrane with a 50 nm pore size and then placing it in diffusion cells. The filter's upper surface was exposed to air while the lower surface was in contact with phosphate buffer solution (having pH 6.5) [19].
Transcellular delivery
Ethosomes were found to be a more attractive clinical option for anti-HIV treatment than the marketed formulation.
HPLC analysis
The drug concentration in the receptor compartment was determined in vitro by skin permeation experiments. MT-2 cells were also tested. HPLC assay used methanol: Distilled water: Acetonitrile (70/20:10 vol/vol) as the mobile phase.
Transdermal drug delivery of harmones
Oral administration of hormones can be problematic due to temperature. These include high first pass metabolism, low oral Bioavailability, and many dose dependent side effects. Each missed pill increases the risk of standard deviation failure [20].
Delivery of anti-arthritis
Drug Oral administration has a few problems, including low bioavailability and first pass metabolism.
Delivery of antibiotics
The epidermis is rapidly penetrated by the ethosomes, which bring an appreciable amount to the deeper layers of the skin and reduce infection at the root.
Statistical analysis
All data generated were tested for statistical significance using ANOVA and standard range tests. The confidence limit was set at P 0.05 for the interpretation of the results by PRISM (GraphPad Version 2.01, San Diego CA) [21].
Application
Ethosomes for percutaneous delivery
It has been shown that ethosomes can deliver drugs with greater proficiency than 65%. They are able to penetrate human skin remuneratively. Ethosomes have been shown to be a reliable vehicle for drug delivery into strata. They are also effective in treating many skin conditions. Comparative studies were conducted to assess the penetration of Minoxidil in vitro using either hydroethanolic, ethanolic, or phospholipid-ethanolic micella solutions of minoxidil. The excipients used in this study were water and phospholipid. The study concluded that minoxidil's permeability was increasing. Excipients used were water and phospholipid. Permeation studies in human skin showed that formulations containing ethosomes had a higher permeation rate than those containing hydroethanolic solutions. Also, the transdermal flux was greater in cases of formulations containing these ethosomes. A study was done on candidiasis patients to assess the effectiveness of ethosomes. It was encapsulated in fluconazole against liposome-loaded gel. This formulation is available on the market. The in vitro permeation experiment revealed that ethosomes permeated twice as much as liposomes, while ethosomes permeated three times more than the hydroethanolic solution. DSC study demonstrated that ethosome fluidity was significantly higher than liposomes [22].
DNA delivery
The skin is an immunologically active organ. It allows gene expression and acts as an important disputing barrier that microorganisms can pass through. It aids in DNA delivery to molecules in skin cells that have been encapsulated in protein, i.e. GTP-Cytomegalovirus, (CMV), focused by transfecting construct to ethosome for gene transcription. This is also a necessary application of ethosomes. CLSM studies have shown that drug delivery has been made easier by the use of the ethosomal formulation, which was applied to the dorsal end of CD-1 male mice for 48 hours. Thus the Green fluorescent protein-cytomegalovirusdriven transfecting construct allowed an effective gene expression into cells of skin [23].
Ethosomes in hormone delivery
The oral dosage form of hormone delivery can cause side effects such as depleted oral BA and side effects due to dose dependence. These side effects are not the only ones. The oral form of hormonal delivery also has a significant impact on patient compliance. Study on testosteroneloaded ethosomes for percutaneous delivery was done to determine if hormonal delivery could be performed on rabbit skin. This revealed that the testosterone-ethosomal formulation was 30 times more permeable than the skin. The drug deposition of the formulation containing episomes was significantly greater (P-0.05). Comparing the testoderm (18.32 ± 4.05 ug) with the testosome (130.76 ± 18.14 ug), the C max (and Area under curve (AUC), of testosterone has been increased in the case of the testosome. Improvement in permeation of skin and bioavailability of drug was observed after the in vitro and in vivo studies of testosterone loaded ethosomal formulation [24].
Transcellular delivery of ethosomes
Ethosomes are a powerful enhancer for drug delivery in the transcellular pathway. This was demonstrated by a study in which we used ethosomal efficacy for many drugs in clinical trials. We studied the transcellular delivery of molecules of 3T3 Fibroblasts in a study in which we used a large number of physicochemical properties of ethosomes and lipid carriers including ethanol. 4-(4-diethylamino) styryl-N-methylpyridinium iodide (D289), rhodamine red dihexadecanoyl glycerophosphoethanolamine and fluorescent PC were selected as probes. CLSM and FACS studies examined the penetration properties of probes fluorescently into fibroblasts and naked mice skin. CLSM micrographs showed that probes penetrated into cells by ethosomes, which produced a stronger fluorescence. However, there was no fluorescence when the probes were incorporated into liposomes or hydroethanolic solutions. After incubation for 3 minutes, intracellular presence was determined using three probes. Calcein, which is hydrophilic in nature, was used to observe improved drug penetration using ethosome as a carrier. The in vitro method was used. Franz diffusion cell was used to study the permeation of transdermal delivery in human Hypertrophic Scars (HS). The skin for 5-Fluoracilloaded ethosomes and skin for HS also participated in this permeation study. The drug's extent was determined after 24 hours of permeation. The 5-fluoracil that penetrated skin was extensive through HS (E–scar), in addition to a hydroethanolic solutions through H-Scar skin, H-Skin, and ethosomes through H- Skin (47), 48 (48). For analyzing the permeability between ethosomes and fluorescently labelled rhodamine 6 GO skin and HS, Confocal Laser Scanning Microscopy was used. Permeation was greatest in HS. The ethosomes were able to label nanoparticles, such as quantum dots, on different strata of scar tissue and deliver medicines. This study shows that ethosomes are capable of fluorescence labelling quantum dots [25].
Infection in the skin by ethosomes
The ethosomes have a very high antibiotic activity for treating skin infections. Animal models of skin infections were used to test the effectiveness of antibiotics. On a Staphylococcus aureus-infected mouse, a comparison was made between erythromycin loaded episomes and hydroethanolic erythromycin solution for treating dermal infections. The ethosomal erythromycin solution was more effective than the hydroethanolic solution for treating dermal infections. To understand the in vivo mechanism of skin permeability, a study was done using Bacitracin (FITC-Bac), i.e. ethosomes with fluorescently labeled bacitracin. Fluorescent-activated Cell Sorting (FACS) and Confocal Laser Scanning Microscopy (CLSM) experiments were used to calculate the results. The study's calculated results confirm that drug penetration through skin is enhanced by ethosomes [26].
Ethosomes to treat infections by viruses and fungi
Side effects such as low absorption of the medication in the intestine (15%-30%) and side effects related to the dose have decreased. In addition, it increases the penetration of ACV through percutaneous delivery into the outer layer. This allows for viral replication. Comparative study was done between the market-available 5% Acyclovir Cream and the 5% ethosome-loaded acyclovir preparation. This study demonstrated the efficacy and innovation of ethosomes in local delivery of hydrophilic drugs based on Supra-Vir cream [27].
Parkinsonism treatment with ethosomes
Trihexphenidyl, a cationic anti-MI drug-muscarinic drug (THP), is used to treat Parkinsonism. Parkinsonism affects 2% to 4% of the elderly. The half-life of THP is approximately 3 h. It can be taken orally three to four times per day. Parkinsonism can cause motor instabilities, neurological manifestations, and oral administration is not recommended. Older patients may have difficulty swallowing the drug. Drug delivery via THP topical route is a great way to overcome these problems. Stratum corneum, a barrier with affinity for lipids, resists restriction to molecules which are ionic in their nature. The purpose of ensuring that topical THP delivery is efficient and successful is the reason for the introduction of ethosomes. The particle size of THP containing Ethosomes was small (i.e. The particle was 109 ± 2 nm in size and the entrapment efficiency was higher (75 ± 0.5%). Percutaneous delivery of ethosomal THP in mice was compared to liposomal THP. The skin of naked mice was used for the dorsal side, which showed a THP flux that was around fifty times greater than liposomes. After 18 hours of experiment, the drug quantity in skin was significantly higher than that in ethosomes. The stability of ethosomal THP was two years or more [28].
Hairloss treatment using ethosomes laced with minoxidil
A large number of people are currently affected by hair issues such as Alopecia and Seborrhea. For treating pilosebaceous disorders, it is important to target the hair follicles. Minoxidil, a drug that has a greater affinity for lipid, is commonly applied to the scalp to treat alopecia. In vivo studies were conducted on hairless rats to determine the activity of ethosome-loaded minoxidil in their sebaceous gland. The pilosebaceous unit showed a greater delivery of minoxidil, which was more visible when ethosome was used to transport it [29].
Ethosomes to anti-arthritis and anti-inflammatory activity
Volunteers suffering from erythema caused by methylnicotinate, we examined the anti- inflammatory effects of ethosomes loaded with Ammonium Glycyrrhizinate. To understand the effects of ethosomes in erythema, we made a comparison between the hydroethanolic drug solution and the anti-inflammatory activities of ethosomes containing ammonium glutamate.
The Erythema index was calculated using a Reflectance visible Spectrophotometer. The ethosomes containing Ammonium glycol showed a decrease in the severity and duration of erythema when compared with hydroethanolic solutions. Cannabidiol, a drug used to treat rheumatic disease, has a high affinity for lipid. Side effects include poor BA due to low hepatic metabolism, gastric pH instability, and low aqueous Solubility. In vivo penetration studies were used to assess Ethosomal CBD's skin permeability. The drug was found to accumulate in the skin and tissues beneath.
Vaginal delivery with ethosomes
Metronidazole ethosomes that are pH sensitive were prepared and tested for their activity in vaginal delivery. In vitro skin permeation study was performed on Franz diffusion cells using phosphate buffer with a pH of 5.8 and a cellulose semipermeable membrane. The flux of the metronidazole ethosome-loaded with metronidazole was at its maximum value, i.e, The measured flux was 143.67 ± 2.73 Ug/cm2/h, which indicates that the metronidazole ethosomes are being delivered continuously.
Conclusion
The transdermal route offers a promising alternative to systemic drug delivery. Ethosomes is a pioneer in transdermal drug delivery research. Ethosomes can be used as drug carriers because they are malleable, soft vesicles. Ethosomes can be customized for increased skin penetration of active drugs.
They are easy to prepare, safe and effective. Ethosomes are more effective at delivering drugs to skin than liposomes and hydro-alcoholic solutions. Ethosomes can be used to encapsulate hydrophilic, cationic, proteins, and peptides. The development of new, improved therapies is possible through the use of ethomal carriers.
References
- Robert L. Polymer-controlled drug delivery systems. Acc Chem Res 1993; 26: 537-542.
- Jong-HoKim, Kyeongsoon Park, Hae Yun Nam, Seulki Lee, Kwangmeyung Kim, Ick ChanKwon. Polymers for bioimaging. Prog Poly Sci 2007; 32: 1031-1053.
- Thacharodi D, Panduranga Rao K. Development and in vitro evaluation of chitosan based transdermal drug delivery systems for the controlled delivery of propranolol hydrochloride. Biomaterials 1995; 16: 145-148.
[Crossref] [Google Scholar] [PubMed]
- Davis Stanley S, Lisbeth Illum. Drug delivery systems for challenging molecules. Int J Pharm 1998; 176: 1-8.
- Cross SE, Michael S. Roberts. Targeting local tissues by transdermal application: Understanding drug physicochemical properties that best exploit protein binding and blood flow effects. Drug Develop Res 1999; 46: 309-315.
- Finnin CB. Transdermal drug delivery-What to expect in the near future. Business Briefing: Pharma Tech 2003: 192-193.
- Kumar, Ritesh, Anil Philip. Modified transdermal technologies: Breaking the barriers of drug permeation via the skin. Tropical J Pharma Res 2007; 6: 633-644.
- Martin RJ, Stephen PD, Jonathan Hadgraft. Skin metabolism of topically applied compounds. Int J Pharm 1987; 39: 23-32.
- Denyer SP, Richard H Guy, Jonathan Hadgraft, Barry WH. The microbial degradation of topically applied drugs. Int J Pharm 1985; 26: 89-97.
- Pannatier AP, Jenner B Testa, JC Etter. The skin as a drug-metabolizing organ. Drug metabolism reviews 8, no. 2 (1978): 319-343.
[Crossref] [Google Scholar] [PubMed]
- Chien Yie W. Transdermal controlled systemic medications. Drugs and the Pharmaceutical Sciences 1987; 31: 416-440.
- Singh UV, Pandey S, Udupa N. Preparation and evaluation of flurbiprofen and diclofenac sodium transdermal films. Indian J Pharma Sci 1993; 55: 145-147.
- Garala KC, Anil JS, Pratik H Shah. Formulation and in vitro characterization of monolithic matrix transdermal systems using HPMC/Eudragit S 100 polymer blends. Int J Pharm Pharma Sci 2009; 1: 108-120.
- Gangwar S, Singh S, Garg G. Ethosomes: A novel tool for drug delivery through the skin. J Pharm Res 2010; 3,4: 688-691.
- Kumar KP, Radhika PR, Sivakumar T. Ethosomes: A priority in transdermal drug delivery. Int J Adv Pharm Sci 2010; 1: 111-121.
- Heeremans JLM, Gerristen HR, Meusen SP, Mijnheer FW, Gangaram RS, Panday G, Prevost R, Kluft C, Crommelin DJA. The preparation of tissue type Plasminogen Activator (t- PA) containing liposomes: Entrapment efficacy and ultracentrifugation damage. J Drug Targeting 1995; 3: 301.
[Crossref] [Google Scholar] [PubMed]
- Asbill CS, El-Kattan AF, Michniak B. Enhancement of transdermal drug delivery: Chemical and physical approaches. Crit Rev in Ther Drug Carrier Sys 2000; 17: 621.
[Google Scholar] [PubMed]
- Jain H, Patel J, Joshi K, Patel P, Upadhyay UM. Ethosomes: A novel drug carrier. Int J Clin Prac 2011; 7: 1:1-4.
- Upadhyay N, Mandal S, Bhatia L, Shailesh S, Chauhan P. A Review on ethosomes: An emerging approach for drug delivery through the skin. Rec Res Sci Tech 2011; 3: 19-24.
- Sivakranth M, AnjumaAra P, Krishnaveni C, Venkatesh E. Ethosomes: A novel vesicular drug delivery system. Int J Adv Pharma Res 2012; 2:16-27.
- Kumar R, Aslam MD, Tripathi A, Prasad D, Chaudhary V, Jain V, Mishra SK, Singh R. Ethosomes: Novel vesicular carriers in transdermal drug delivery. J Global Pharma Tech 2010; 2: 1-7.
- Rathore AR, Khambete H, Jain S. Preparation and characterization of repaglinide loaded ethosomal gel for the treatment of NIDDM. Int J Pharm Biol Arch 2013;4,2:385- 390.
- Shahwal V, Samnani A, Dubey B, Bhowmick M. Ethosomes: An overview. International J Biomed Adv Res 2011; 2: 161-168.
[Crossref]
- Touitou E. Drug delivery across skin. Expert Opin Biol Ther 2002; 2: 723-733.
[Crossref] [Google Scholar] [PubMed]
- Schreier H, Bovwstra J. Liposomes and niosomes as topical drug carriers: Dermal and transdermal drug delivery. J Cont Rel 1994; 30: 1-15.
- Touitou E, Dayan N, Bergelson L, Godin B, Eliaz M. Ethosomes-novel vesicular carriers for enhanced delivery: Characterization and skin penetration properties. J Cont Rel 2000; 65: 403-418.
- Tyagi LK, Kumar S. Ethosomes: Novel vesicular carrier for enhanced transdermal drug delivery system. Bulletin of Pharmaceutical Research 2013; 3: 6-13.
- Manosrai A, Jantrawut P, Khositsuntiwon N, Manosroi W, Manosroi J. Novel elastic nanovesicles for cosmeceutical and pharmaceutical applications. J Sci 2009; 36: 168-178.
- Gangwar S. Ethosomes: For drug delivery. J Pharm Res 2010; 3: 688-691.