Research Article - Journal of Cardiovascular Medicine and Therapeutics (2018) Volume 2, Issue 2
Young acute coronary syndrome outcomes in heterogenous Asians.
- *Corresponding Author:
- Nicholas Chua Yul Chye
Department of Cardiology Medical Department
of UniversityTechnology MARA (UiTM) Sungai Buloh
Hospital, Malaysia
Tel: +60 3-6126 5000
E-mail: yulchye@gmail.com
Accepted date: March 22, 2018
Citation: Chye NCY, Khir RN, Wen LC, et al. Young acute coronary syndrome outcomes in heterogenous Asians. J Cardiovasc Med Ther. 2018;2(1):1-5.
Abstract
Background: Recently, more patients are presenting at a younger age with acute coronary syndrome (ACS). Objective: Identify the demographics, risk factors and outcomes of young ACS North of Kuala Lumpur, Malaysia. Materials and Methods: This was a prospective, observational study conducted in Sungai Buloh Hospital, North of Kuala Lumpur, Malaysia. Patients were enrolled during 2014 and 2015. Results: There was 1479 ACS, with a mean age of 56 ± 12. 10.6% (n=158) were below 40, with a mean age of 34 with the youngest at 17. Meanwhile 15.8% (n=25) were female. Ethnicity breakdown revealed 62% Malays, 24.1% Indians, 1.2% Chinese and 12.7% of other races. ACS subtypes showed 56.9% unstable angina (UA), 22.2% non-ST elevation myocardial infarction (NSTEMI) and 20.9% ST elevation myocardial infarction (STEMI). Cardiovascular risk factor assessment revealed 46.2% hypertension, 43.0% smokers, 6.3% ex-smokers, 29.7% known ischemic heart disease (IHD), 24.7% diabetes mellitus, 22.8% dyslipidemia, 19.0% positive family history of IHD and 10.8% alcohol consumption. Biochemical analysis showed fasting glucose level of 7.2 ± 3.5 mmol/L and serum creatinine 84.0 ± 23.5 μmol/L. Lipid profile revealed mean total cholesterol of 4.9 ± 1.4 mmol/L, triglyceride 2.2 ± 1.3 mmol/L, HDL 0.9 ± 0.4 mmol/L, and LDL of 3.3 ± 1.1 mmol/L. 30-day mortality was 3.2% while 90-day mortality was 4.5%. Conclusion: Majority of young ACS were male with positive risk factors such as hypertension and cigarette smoking.
Young acute coronary syndrome, Risk factors, Mortality outcomes, Heterogenous Asians, Malaysia.
Introduction
The notion of acute coronary syndrome (ACS) first began in 1772, when William Heberden first described crescendo angina [1] Many decades later, in 1858 Rudolph Virchow proposed that injury to coronary endothelium is possibly due to fat, which might lead to inflammation and secondary plaque formation [2]. Centuries later, coronary artery disease (CAD) is still the global leading cause of mortality [3].
Traditionally, the perception of coronary artery disease is a disease of the elderly. The mean age of ACS was 66 in the expanded Global Registry of Acute Coronary Events (GRACE) [4]. Meanwhile, our Malaysian National Cardiovascular Disease (NCVD) registry demonstrated a younger mean age of 59 [5]. In the Northern part of Kuala Lumpur, the mean age of ACS presenting to Sungai Buloh Hospital was 56 [6]. The National Health and Morbidity Survey illustrated that cardiovascular disease is the leading cause of mortality in Malaysia, contributing to 25.4% of hospital mortalities in 2010 [7].
Key pathophysiology in regional acute myocardial infarction is attributed to thrombosis of a culprit coronary atherosclerotic plaque [8]. Thrombosis occurs from endothelial erosion or plaque rupture [9]. Clinically, this thrombosis is manifested as acute coronary syndrome (ACS), which comprises of unstable angina (UA), non-ST segment elevation myocardial infarction (NSTEMI) with micro-necrosis and transmural ST-elevation myocardial infarction (STEMI).
73% of total deaths in Malaysia are attributed to noncommunicable disease. Most of these deaths are from acute coronary syndrome and strokes. Approximately 35% of deaths occur in those below 60 years of age, which are mainly the working population. The national health and morbidity survey (NHMS) showed a high proportion of Malaysians with undiagnosed non-communicable disease (NCD) risk factors. This leads to late diagnosis, complications, costly in-hospital management and more mortality and morbidity.
We aim to illustrate the demographics, risk factors, biochemical parameters, treatment modalities, mortality and morbidity outcomes of acute coronary syndrome in the young (<40 years).
Methodology and Study Design
This retrospective study was conducted at Sungai Buloh Hospital Malaysia, which is a non-cardiac catheterization centre. The trial was coordinated by the Cardiology Unit of the Medical Faculty of Universiti Teknologi MARA. Using ICD-10 classification, all patients who had unstable angina (UA), non-ST elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI) were identified. All ward admissions were seen by an attending physician. Relevant information were then extracted and statistically analysed. Mortality outcomes were ascertained from the National Death Registry of Malaysia. The study was approved by all appropriate national regulatory authorities and the ethics committee. All authors vouch for the accuracy and completeness of the data and the analyses.
Results
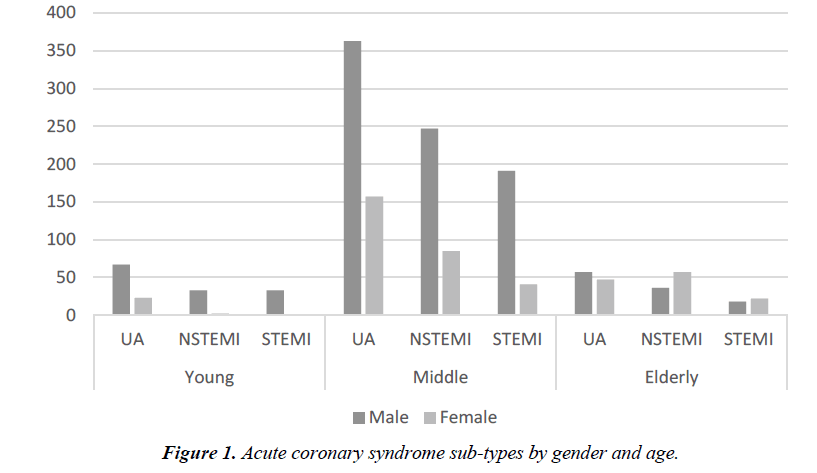
There were 1479 patients with acute coronary syndrome admitted to Sungai Buloh Hospital from 1st January till 31st December 2015. The mean age was 56 ± 12 and 29.3% (n=434) were female. Mean hospital stay was 4 ± 2 days (Figure 1).
The young ACS cohort was comprised of 158 (10.6%) patients under 40-year-old and 25 (15.8%) were women. The mean age was 34-year-old with the youngest being 17. Ethnicity breakdown revealed 62% Malays, 24.1% Indians, 12.7% other ethnicity and 1.3% Chinese. The ACS subtypes were 57% unstable angina (UA), 22% non-ST segment elevation myocardial infarction (NSTEMI) and 21% ST-elevation myocardial infarction (STEMI). Comparing the three different age groups, there is a notable trend in gender difference. There were very few women (15.8%) in the young ACS compared to the middle (26.1%) and elderly (53.2%) age groups (Figure 2).
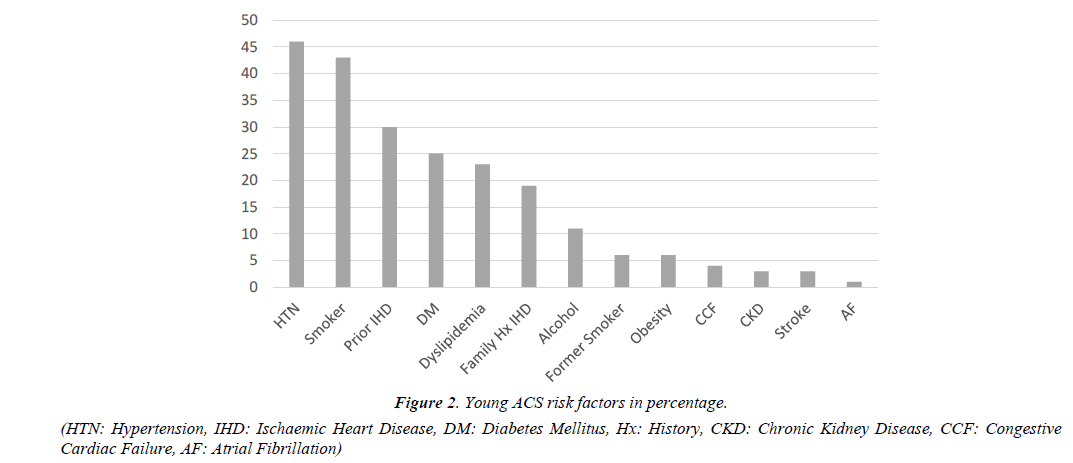
The prevailing cardiovascular risk factor seen in almost half the cohort were hypertension (46.2%, n=73) and tobacco smoking (43%, n=68). There were 10 (6.3%) former tobacco smokers. Comparing the three age groups, young ACS cohort had fewer patients with hypertension, diabetes mellitus, chronic kidney disease, prior stroke, congestive cardiac failure and atrial fibrillation. Conversely, the young ACS cohort had more tobacco smokers, family history of ischemic heart disease and obesity.
Looking at the differences in biochemical analysis of laboratory results, there is a notable trend among the three cohorts. Estimated glomerular filtration rate shows worsening renal function as age advances, with mean of 63.2 mL/min/1.73 m2 in the elderly, compared to 84.0 mL/ min/1.73 m2 in the young. Conversely, the younger cohort illustrates significant lower high-density lipoprotein (HDL) of 0.9 mmol/L (p=0.02), while having higher total cholesterol (TC) of 4.9 mmol/L (p=0.002) and triglyceride (TG) of 2.2 mmol/L (p=0.042). Additionally, peak cardiac enzymes were more elevated in the young (Table 1).
| Parameters | Young (≤ 40) | Middle-aged | Elderly (≥ 70) |
|---|---|---|---|
| Number of patients | 158 | 1084 | 237 |
| Mean age (years) | 34 ± 4 | 55 ± 8 | 76 ± 4 |
| Male | 84.2% | 73.9% | 46.8% |
| Female | 15.8% | 26.1% | 53.2% |
| Mean hospital stay (days) | 4 ± 2 | 4 ± 3 | 4 ± 3 |
| Malay | 62% | 58.1% | 64.6% |
| Indian | 24.1% | 27.7% | 17.7% |
| Chinese | 1.2% | 9.8% | 15.2% |
| Other ethnicities | 12.7% | 4.4% | 2.5% |
| UA | 56.9% | 48.0% | 43.9% |
| NSTEMI | 22.2% | 30.6% | 39.2% |
| STEMI | 20.9% | 21.4% | 16.9% |
| Hypertension | 46.2% | 65.7% | 80.6% |
| Smoker | 43.0% | 30.3% | 9.3% |
| Former Smoker | 6.3% | 11.7% | 10.1% |
| Prior Ischaemic Heart Disease | 29.7% | 42.5% | 48.5% |
| Diabetes Mellitus | 24.7% | 49.0% | 45.1% |
| Dyslipidaemia | 22.8% | 29.8% | 33.3% |
| Family History of IHD | 19.0% | 12.0% | 3.0% |
| Alcohol | 10.8% | 5.0% | 2.5% |
| Obesity | 5.7% | 2.2% | 0.0% |
| Chronic kidney disease | 2.5% | 9.7% | 18.6% |
| Prior Stroke | 3.2% | 5.5% | 10.5% |
| Congestive Cardiac Failure | 4.4% | 7.9% | 15.2% |
| Atrial fibrillation | 1.3% | 2.3% | 9.3% |
| Glycated Haemoglobin (HbA1c %) | 7.4 ± 2.5 | 7.7 ± 2.3 | 7.2 ± 2.0 |
| Fasting Blood Sugar (mmol/L) | 7.2 ± 3.5 | 7.7 ± 3.7 | 7.4 ± 3.3 |
| Estimated Glomerular Filtration Rate (mL/min/1.73 m2) | 75.7 ± 42.9 | 64.5 ± 36.3 | 63.2 ± 138.0 |
| Serum Creatinine (µmol/L) | 84.0 ± 23.5 | 104.6 ± 62.1 | 124.6 ± 77.3 |
| Total Cholesterol (mmol/L) | 4.9 ± 1.4 | 4.9 ± 1.4 | 4.3 ± 1.3 |
| Triglyceride (mmol/L) | 2.2 ± 1.3 | 1.9 ± 1.2 | 1.5 ± 0.7 |
| High Density Lipoprotein (mmol/L) | 0.9 ± 0.4 | 1.0 ± 0.4 | 1.0 ± 0.3 |
| Low Density Lipoprotein (mmol/L) | 3.3 ± 1.1 | 3.2 ± 1.2 | 2.9 ± 1.1 |
| Peak Trop I (ng/mL) | 18.7 ± 77.8 | 44.8 ± 1009.8 | 3.3 ± 13.4 |
| Peak Creatine Kinase (IU/L) | 685.1 ± 1420.5 | 525.3 ± 1136.7 | 396.5 ± 907.6 |
| 30-day mortality | 3.2% (n=5) | 5.6% (n=61) | 15.2% (n=36) |
| 90-day mortality | 4.5% (n=7) | 7.5% (n=81) | 17.3% (n=41) |
Table 1. Comparing baseline characteristics and mortality outcomes of different groups of ACS.
Across the three age groups, significant 30-day mortality risks were seen in those with deranged fasting blood sugar (p=0.004), elevated estimated glomerular filtration rate (p=0.001), elevated serum creatinine (p=0.001), peak Troponin I (p=0.042) and creatine kinase (p=0.001). Increasing age also showed significant mortality predictor (p<0.01), where the 30-day mortality in the elderly cohort (15.2%) was much higher than the young cohort (3.2%) (Table 2).
| Mean Biochemical Parameters | Alive | Dead | P value |
|---|---|---|---|
| Glycated Haemoglobin (HbA1c) | 7.51 | 7.09 | 0.693 |
| Fasting Blood Sugar (mmol/L) | 7.69 | 8.98 | 0.004 |
| Estimated Glomerular Filtration Rate (mL/min/1.73m2) | 73.02 | 47.61 | 0.001 |
| Serum creatinine (umol/L) | 113.49 | 253.12 | 0.001 |
| Total Cholesterol (mmol/L) | 5.12 | 4.63 | 0.345 |
| Triglyceride (mmol/L) | 1.85 | 1.61 | 0.962 |
| High Density Lipoprotein (mmol/L) | 1.00 | 0.92 | 0.178 |
| Low Density Lipoprotein (mmol/L) | 3.28 | 2.99 | 0.805 |
| Peak Troponin I (ng/mL) | 8.36 | 35.60 | 0.042 |
| Peak Creatine Kinase (IU/L) | 570.55 | 2199.87 | 0.001 |
Table 1. Comparing baseline characteristics and mortality outcomes of different groups of ACS.
Discussion
According to the multinational Global Registry of Acute Coronary Events (GRACE) registry which studied patients in 14 countries excluding Africa and Asia, large differences exist in management practice by hospital type and geographic location despite comparable use of antiplatelet and anticoagulants. Greatest survival at 6 months was associated with timely coronary artery bypass graft (CABG), percutaneous coronary intervention (PCI), use of clopidogrel and statins [10].
In the Malaysian NCVD-ACS registry, fibrinolysis use was relatively high (>70%) and use of invasive procedures were low (13-17%) compared to other registries. 30-day in-hospital mortality was higher amongst the Malay (7%) compared to other ethnic groups (4-6%) and rates from other Asian registries [11-14]. Geography, education towards chest pain awareness, lack of healthcare insurance and government medical infrastructures are several challenges in the local setting. Advantages from optimal acute and post-discharge treatment are supported by other registries, such as the SNAPSHOT ACS study and the Genesis Heart Care Group Registry (GHCGR). Both were able to illustrate the variability in resources and in-hospital major adverse cardiac event (MACE) rates across different healthcare jurisdictions [15,16].
The Asia-Pacific Real world evidence on Outcome and Treatment of ACS (APRICOT) made several key strategic recommendations to improve ACS outcomes in the Asia- Pacific region: longer-term patient surveillance, better patient education, overcoming geographical challenges to pre-hospital and post-discharge care, and adoption of value-based over costbased health care systems [17]. Greater emphasis is made to improve long-term outcomes in ACS 17.
Implementation of post-hospital coaching programmes, such as the coaching patients on achieving cardiovascular health (COACH) programme in Australia has been proven to be effective in improving both short-term and long-term outcomes [18]. Medical treatment cost is a major barrier to patients in most countries in the Asia-Pacific region. In Australia, clopidogrel administered in-hospital is reimbursed and subsidized postdischarge. Despite of that, adherence up to 12 months is only 60-70% [19,20]. In China, less than 40% of patients remain compliant to medications at 12 months post-discharge, mostly due to patient refusal [21]. Improvement of patient education is required regarding acute coronary syndrome, especially in reducing time-to-treatment and improving pharmacological adherence. Possible patient engagement is through community talks, dissemination of knowledge on various multimedia platforms and ultimate importance of prevention and health screenings.
Tobacco smoking prevalence in Malaysia is at 22.8% [22]. It was estimated that nearly five million Malaysians aged 15 years and above smoked. The prevalence of exposure to second-hand smoke at home was 37.1% [23,24]. Previous studied have demonstrated that tobacco smoking produces more atherosclerosis [25]. This is mainly attributed by changed in cholesterol levels, platelet aggregation and damage to endothelium [26]. Exposure to tobacco smoking increases risk of acute coronary syndrome by 25% for a non-smoker compared with the unexposed [27,28].
The National Health and Morbidity Survey (NHMS, 2015), highlighted that prevalence of hypertension among adults 18 years old and above is 30.5%. The prevalence of hypertension in the 18-19 years age group was at 6%. It is estimated that 6.4 million individuals are hypertensive in Malaysia. Hypertension is associated with development of atherosclerosis and vulnerable plaques. Hypertension is linked with other factors such a genetic risk, insulin resistance, sympathetic hyperactivity, and vasoactive substances [29]. In the SYMPHONY trial, prevalence of hypertension in STEMI was more than 50% [30].
Conclusion
The paradigm shift of younger patients presenting with acute coronary syndrome is alarming. With the ever increasing burden of non-communicable disease, ACS related mortality and morbidity will only increase and present at a much earlier age. There are multiple barriers that require attention to further improve outcomes in our local setting.
References
- Heberden W. Some account of a disorder of the breast. Med Trans Coll Physicians Lond 1772;2:59.
- Simmons J. Rudolph Virchow and the cell doctrine. The Scientific 100—A Ranking of the Most Influential Scientists, Past and Present. Secaucus, Carol Publishing Group, NJ, USA. 1996;88–92.
- World Health Organization, Global Health Observation Data, 2015.
- Goodman SG, Huang W, Yan AT, et al. Expanded Global Registry of Acute Coronary Events (GRACE2) Investigators. The expanded Global Registry of Acute Coronary Events: baseline characteristics, management practices, and hospital outcomes of patients with acute coronary syndromes. Am Heart J. 2009;158(2):193.
- Ahmad WA, Sim KH. Annual Report of the NCVD-ACS Registry, 2009 & 2010. Kuala Lumpur, Malaysia: National Cardiovascular Disease Database. 2013.
- Chua N, Khir RN, Chong PF, et al. Under-optimized prior statin therapy in acute coronary syndrome. Int. J. Cardiol. 2017;349:S35-S36
- Institute for Public Health (IPH). National Health and Morbidity Survey 2015 (NHMS 2015). Vol. II: Non-communicable diseases, Risk Factors & Other Health Problems. 2015.
- Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med 2007; 357:2482-494
- The pathophysiology of acute coronary syndromes. Heart. 2000;83:361-66
- Fox KA, Goodman SG, Klein W, et al., Management of acute coronary syndromes. Variations in practice and outcome; findings from the Global Registry of Acute Coronary Events (GRACE). Eur. Heart J. 2002;23:1177–189.
- Lu HT, Nordin RB. Ethnic differences in the occurrence of acute coronary syndrome: results of the Malaysian National Cardiovascular Disease. Cardiovasc. Disord. 2013;13:97.
- Ahmad WA, Ali RM, Khanom M, et al. The journey of Malaysian NCVD-PCI (National Cardiovascular Disease Database-Percutaneous Coronary Intervention) Registry: a summary of three years report. Int J Cardiol. 2013;165:161–64.
- Peterson ED, Dai D, De-Long ER, et al. Contemporary mortality risk prediction for percutaneous coronary intervention: results from 588,398 procedures in the National Cardiovascular Data Registry. J Am Coll Cardiol. 2010;55:1923–932.
- Yan BP, Clark DJ, Buxton B, et al. Clinical characteristics and early mortality of patients undergoing coronary artery bypass grafting compared to percutaneous coronary intervention: insights from the Australasian Society of Cardiac and Thoracic Surgeons (ASCTS) and the Melbourne Interventional Group (MIG) Registries. Heart Lung Circ. 2009;18:184–90.
- Chew DP, French J, Briffa TG, et al. Acute coronary syndrome care across Australia and New Zealand: the SNAPSHOT ACS study. Med J Aust. 2013;199:185–91.
- Eccleston D, Horrigan M, Rafter T, et al. Long-term outcomes after percutaneous coronary intervention in Australian private hospitals; Results from a National Registry. Circ. Cardiovasc Qual Outcomes. 2013;6:A35.
- Mark CY, Du X, Eccleston D, et al. Acute coronary syndrome in the Asia-Pacific region. Int. J. Cardiol. 2016;202:861-69.
- Vale MJ, Jelinek MV, Best JD, et al. Coaching patients on achieving cardiovascular health (COACH): A multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003;163:2775–783.
- Cole JA, Brennan AL, Ajani AE, et al. Cardiovascular medication use following percutaneous coronary intervention: the Australian experience, Cardiovasc. Ther. 2014;32(2):47-51.
- Nelson MR, Reid CM, Ryan P, et al. Self-reported adherence with medication and cardiovascular disease outcomes in the Second Australian National Blood Pressure Study (ANBP2). Med J Aust. 2006;185:487–89.
- Bi Y, Gao R, Patel A, et al. Evidence-based medication use among Chinese patients with acute coronary syndromes at the time of hospital discharge and 1 year after hospitalization: results from the Clinical Pathways for Acute Coronary Syndromes in China (CPACS) study. Am Heart J. 2009;157:509–16.
- Institute for Public Health (IPH). Report of the Global Adult Tobacco Survey (GATS) Malaysia, Ministry of Health Malaysia. 2012.
- Disease Control Division, Ministry of Health: Clinical Practice Guidelines. Treatment of Tobacco smoking and dependence. 2003.
- Institute for Public Health. Second Malaysia Burden of Disease and injury study, Institute for Public Health, Kuala Lumpur, Malaysia. 2012.
- Roberts KA, Rezai AA, Pinkerton KE, et al. Effect of environmental tobacco smoke on LDL accumulation in the artery wall. Circulation. 1996;94:2248–53.
- Davies J, Shelton L, Watanabe I, et al. Passive smoking affects endothelium and platelets. Arch Intern Med. 1989;149:386–9.
- Kritz H, Schmid P, Sinzinger H. Passive smoking and cardiovascular risk. Arch Intern Med. 1995;155:1942–8.
- Dobson AJ, Alexander HM, Heller RF, et al. Passive smoking and the risk of heart attack or coronary death. Med J Aust. 1991;154:793–7.
- Picariello C, Lazzeri C, Attanà P, et al. The impact of hypertension on patients with acute coronary syndromes. Int J Hypertens. 2011;563:657.
- Frazier CG, Shah SH, Armstrong PW, et al. Prevalence and management of hypertension in acute coronary syndrome patients varies by sex: Observations from the Sibrafiban versus aspirin to Yield Maximum Protection from ischemic Heart events post acute coronary syndromes (SYMPHONY) randomized clinical trials. Am Heart J. 2005;150(6):1260–267.