Research Article - Biomedical Research (2018) Volume 29, Issue 4
Two-factor analysis of blood loss in total knee arthroplasty
Shixiong Zheng1,2, Qiang Li1, Hailun Zhu1, Yong Hu1, Zhanjun Shi1* and Jun Xiao1*
1Department of Orthopaedic Surgery, Nanfang Hospital, Southern Medical University. No. 1838 Guangzhou North Road, Guangzhou, Guangdong, PR China
2Department of Orthopaedic Surgery, the Second Hospital of FuZhou Affiliated to Xiamen University, PR China
- *Corresponding Authors:
- Jun Xiao
Department of Orthopaedic Surgery
Nanfang Hospital
Southern Medical University, PR China
Zhanjun Shi
Department of Orthopaedic Surgery
Nanfang Hospital
Southern Medical University, PR China
Accepted date: November 21, 2017
DOI: 10.4066/biomedicalresearch.29-17-3464
Visit for more related articles at Biomedical ResearchAbstract
Purpose: The effect of the intercondylar osteotomy and location hole plugging on blood loss during Total Knee Arthroplasty (TKA) was investigated.
Material and Methods: A retrospective-controlled study was performed by including 304 cases of knee replacement in our hospital. The clinical data were recorded and blood loss was calculated. Theoretical blood loss was calculated at different times. The Gross equation was used in all original data. The cases were divided into two groups according to mode of intercondylar osteotomy. Meanwhile, three classifications were obtained on the basis of the mode location hole plugging. SPSS17.0 software was used for the analysis and comparison in different groups.
Results: The groups were compared after TKA, and the results showed that femoral intercondylar osteotomy group lost more blood than non-intercondylar osteotomy group a day after the operation, but no statistical difference was observed on the third and fifth day. On the first and third day after the operation, the bone-plugging group (on the location hole) lost less blood than the cement-plugging group, which showed no significant difference with the no-plugging group. Moreover, five days after the operation, the no-plugging group experienced more bleeding than the no-plugging. Meanwhile, the cement-plugging group had the most blood loss among the experimental groups.
Conclusions: Relative to blood loss, the performance of non-osteotomy prosthesis was superior to osteotomy prosthesis in TKA. Bone plugging for femoral location holes can reduce blood loss, although no significant value was obtained in cement plugging.
Keywords
Total knee arthroplasty, Amount of blood loss, Intercondylar osteotomy of femur, Plugging of femoral location holes, Statistical difference
Introduction
The effect of Total Knee Arthroplasty (TKA) surgery is definite in the treatment of severe knee osteoarthritis and other diseases [1]; joint pain can be relieved, and corresponding function can be rebuilt in about 90% of patients with severe knee osteoarthritis by TKA [2,3]. However, TKA is limited by many factors, such as blood loss, which is the most severe of all these factors. Some scholars estimated that the average amount of blood loss can reach 1471 m in the first replacement surgery [4]. Meanwhile, the risk of allogenic blood transfusion in perioperative period can be as high as 15%-62% because of blood loss [5,6]. The risk of allogeneic blood transfusion has the same rate [7-11]. If the amount of blood loss can be reduced to a minimum, the popularization of surgery will be greatly promoted.
Many scholars have been attempting to explore the influence of various factors on blood loss. The roles of these factors have been repeatedly demonstrated, and some have reached agreement. For example, several researchers studied the application of tourniquet in the early days and confirmed that tourniquet use can reduce the amount of bleeding in TKA [12-15]. In addition, a large number of clinical studies regarding the application of tranexamic acid are reported. Tranexamic acid reduces the amount of intraoperative bleeding without increasing the risk of DVT; therefore, this chemical can be regarded as a safe and effective measure in the perioperative period [16-18]. However, research on the reduction of perioperative blood loss in TKA remains lacking.
In this study, the clinical data from 304 patients that underwent TKA were studied in Nanfang Hospital of Southern Medical University were investigated. Gross equation was used for the calculation of postoperative blood loss. The patients were grouped according to mode of location hole plugging and intercondylar osteotomy. Differences in the amount of blood loss among the groups were obtained and analysed. Kruskal- Wallis test was performed on SPSS17.0 software. These two factors were found to have some impact on blood loss, which in turn contribute to the exploration of their influence on reducing the blood loss caused by surgery.
Materials and Methods
Patients
From January 2011 to June 2016, patients with final diagnosis of osteoarthritis and accepted TKA were included in the study. Patients with the following disease were excluded from the study: knee joint advanced diseases of Rheumatoid Arthritis (RA) and Ankylosing Spondylitis (AS), Kashin Beck disease, infection and sequelae of infection, cancer, severe cardiovascular and cerebrovascular diseases, liver diseases and severe liver dysfunction, blood system diseases such as coagulation disorders (such as hemophilia), thrombocytopenia, etc. In addition, patients with long-term use of anticoagulants were also excluded. For patients with hypertension, blood pressure should be reduced to 140/90 mmHg. Finally, 304 patients were included in the study, including 61 males and 243 females, aged from 42 to 80 y, with an average age of 56.8 y. The general data of 304 patients were shown in Table 1. The study was approved by the ethics committee of the hospital, and all the patients signed of the informed consent.
| Classification | Cases |
|---|---|
| Bone plugging | 82 |
| No plugging | 124 |
| Cement plugging | 98 |
| Intercondylar osteotomy | 204 |
| Non-intercondylar osteotomy | 100 |
| Total | 304 |
Table 1. General information.
Surgical indication, technique, and perioperative management
The indications of the operation for all patients included: pain or dysfunction caused by severe osteoarthritis of the knee, ineffective conservative treatment and influence in the daily life, joint space stenosis shown in X-ray plain film, cystic changes, osteosclerosis and osteophyte formation observed in the subchondral bone of the knee.
All surgical procedures were standardized (Median knee incision, and the incision length ranged from 10 to 15 cm) and performed by an experienced team in the supine position of the patient. Anesthesia was performed under general anesthesia or under spinal anesthesia. Postoperative cephalosporins were routinely administered for 24 h to prevent infection. Patients were not allowed to choose any weight or sex before the operation.
There were two kinds of intercondylar treatment before femoral prosthesis installation, osteotomy or non-osteotomy, which was determined by the type of prosthesis. Osteotomy was not selected before the operation, and it was completely randomized. The location holes used in femoral intramedullary fixation were processed in 3 different ways after the positioning was completed, one for no treatment, the second was that the cement (Polymethyl methacrylate) was packed into the location hole when the femoral prosthesis was installed during the operation, and the third was that the cancellous bone fragments after the osteotomy were tapered into the location holes, and the columns were tightened to fill the holes. Various processing methods were selected completely randomly and free of any other factors.
Collection data
General information of age, gender, diagnosis, surgeon, height, weight, Hemoglobin (Hb) and Hematocrit (Hct) before operation and on the 1st, 3rd, and 5th days after operation (The results before operation were those indexes detected within 2 d preoperatively, and the results after operation were the results of blood drawing around 7 a.m. on the 1st, 3rd, and 5th d after operation), as well as the amount of blood loss, blood transfusion and auto-transfusion were recorded. Meanwhile, whether the prosthesis needed osteotomy or not, and the location of the hole during the operation were recorded respectively.
Calculation of blood loss
Firstly, the calculation of blood loss using hidden blood loss was calculated according to the Gross equation improved by Gross JB [19].According to Hct, the theoretical blood loss was calculated by calculating the total amount of blood loss, then subtracting the total amount of auto-transfusion and the total amount of allogeneic blood transfusion. Concrete calculation method of Gross equation was: theoretical total blood loss=Preoperative Blood Volume (PBV) × 2 × (Preoperative Hct-Postoperative Hct)/(Preoperative Hct+Postoperative Hct). Among them, PBV=k1 × height (m)3+k2 × body weight (kg) +k3. Male k1=0.3669, k2=0.0329, k3=0.6041; female k1=0.3561, k2=0.033 08, k=0.1833. The total amount of blood loss was calculated on the 1st, 3rd, and 5th d after operation, followed by the measurement of the amount of blood loss increased in 1-3 d, and the amount of blood loss increased in 3-5 d.
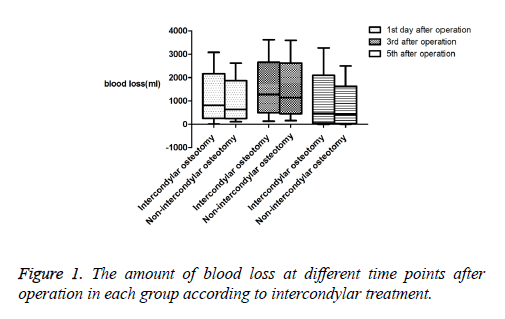
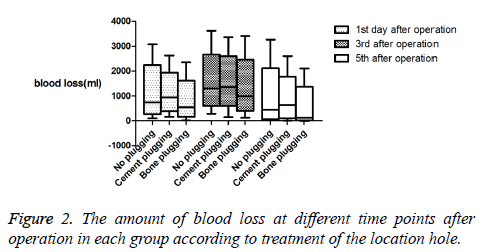
Statistical analysis
After the calculation of the total amount of blood loss on the 1st, 3rd, and 5th d after operation, two groups of intercondylar osteotomy group and non-intercondylar osteotomy group were divided according to the operation of intercondylar osteotomy, meanwhile, three groups of no plugging group, cement plugging group and bone plugging group were classified based on the plugging of the location hole. SPSS17.0 software was used to calculate the median and quartile values of each group according to the treatment of osteotomy (Table 2), box plot was then figured out (Figure 1), Kruskal-Wallis test was used to compare the differences between groups, and the significant difference between groups was obtained (Table 3); Furthermore, the median and quartile values were also measured by SPSS17.0 software in each group based on the plugging of the location hole (Table 4), and box plot was constructed (Figure 2), Kruskal-Wallis test compared the difference between groups, followed by the calculation of the significant difference between groups (Table 5).
| Grouping based on intercondylar treatment | Total blood loss in the 1st d | Total blood loss in the 3rd d | Total blood loss in the 5th d | ||
|---|---|---|---|---|---|
| Intercondylar osteotomy | Cases | 204 | 204 | 204 | |
| Minimum value | 10 | 131 | -4 | ||
| Maximum value | 3077 | 3620 | 3269 | ||
| Percentile | 25 | 474 | 108 | ||
| 50 | 817 | 469 | |||
| 75 | 1242 | 922 | |||
| Non-intercondylar osteotomy | Cases | 100 | 100 | 100 | |
| Minimum value | 115 | 150 | -3 | ||
| Maximum value | 2619 | 3591 | 2495 | ||
| Percentile | 25 | 366 | 66 | ||
| 50 | 632 | 428 | |||
| 75 | 112 | 744 | |||
Table 2. The amount of blood loss in each group according to intercondylar osteotomy.
| Grouping time | 1st d after operation | 3rd d after operation | 5th d after operation |
|---|---|---|---|
| Intercondylar osteotomy/non-intercondylar osteotomy | 0.024 | 0.105 | 0.126 |
Table 3. Statistical differences of blood loss in each group according to intercondylar osteotomy (The value of 0.05 meant that the difference was statistically significant).
| Plugging | Total blood loss in the 1st d | Total blood loss in the 3rd d | Total blood loss in the 5th d | ||
|---|---|---|---|---|---|
| No plugging | Cases | 124 | 124 | 124 | |
| Minimum value | 99 | ||||
| Maximum value | 3077 | ||||
| Percentile | 25 | 428 | 902 | ||
| 50 | 744 | 1293 | 454 | ||
| 75 | 1395 | 1697 | 964 | ||
| Cement plugging | Cases | 98 | 98 | 98 | |
| Minimum value | 166 | ||||
| Maximum value | 2625 | ||||
| Percentile | 619 | 1034 | |||
| 50 | 934 | 1351 | 633 | ||
| 75 | 1253 | 1844 | 942 | ||
| Bone plugging | Cases | 82 | 82 | 82 | |
| Minimum value | 10 | ||||
| Maximum value | 2356 | ||||
| Percentile | 308 | 669 | |||
| 50 | 545 | 989 | 128 | ||
| 75 | 867 | 1533 | 634 | ||
Table 4. Mean and standard deviation of blood loss in each group according to the plugging of the location hole.
| Grouping time | 1st d after operation | 3rd d after operation | 5th d after operation |
|---|---|---|---|
| Cement plugging/no plugging | 0.079 | 0.482 | 0.088 |
| Cement plugging/bone plugging | 0 | 0.001 | 0 |
| Bone plugging/no plugging | 0.001 | 0.007 | 0 |
| Total difference between groups | 0 | 0.002 | 0 |
Table 5. Statistical differences of blood loss in each group according to the plugging of the location hole (The value of 0.05 meant that the difference was statistically significant).
Results
As shown in Tables 2 and 3 and Figure 1, the mean blood loss of the intercondylar osteotomy prosthesis group was greater than that of the non-osteotomy prosthesis on the first day after the operation, and the difference between the groups was statistically significant. No statistical difference was observed on the third and fifth day.
Among the groups obtained on the basis of the mode of femoral location hole plugging, significant differences were observed on the first, third and fifth day after the operation (Tables 4 and 5 and Figure 2). On the first and third day after the operation, the amount of blood loss in the bone-plugging group was less than that of the cement-plugging group and noplugging group, and no statistical difference in the amount of blood loss was observed between the cement-plugging and noplugging groups. In particular, no plugging group=cement plugging group>bone plugging group relative to the amount of blood loss. On the fifth day, the amount of blood loss in the bone-plugging group was significantly less than that in the cement-plugging and no-plugging groups, and the amount of blood loss in the cement-plugging group was significantly greater than that in the no-plugging group. The sequencing for blood loss can be expressed as: cement plugging group>no plugging group>bone plugging group.
Discussion
Blood loss after TKA is the most serious problem that hinders the progress of surgery. So far, this action has been widely recognised and became a common concern and has long been confirmed [20]. For the correction of preventive measures for blood loss reduction, various influencing factors of blood loss should be clarified in the perioperative period of TKA.
During TKA, intercondylar osteotomy prosthesis and the nonosteotomy prosthesis can both be selected, although intercondylar osteotomy is not an essential step for TKA. Some scholars, such as Zhang [21], analysed and compared these two types of prosthesis and found that each has its own advantages and can achieve a satisfactory curative effect, although the amount of blood loss and postoperative Hb level of the nonosteotomy prosthesis were better than those of the osteotomy prosthesis. Moreover, reports on the relationship between blood loss and the need for osteotomy in prosthesis are few.
In the present study, the two prostheses were compared between groups. Statistical differences were observed on the first day after operation (intercondylar osteotomy group: 817 ml vs. non-intercondylar osteotomy group: 612 ml). Nevertheless, no obvious statistical difference in the amount of blood loss was found on the third day (intercondylar osteotomy group: 1279 ml vs. non-intercondylar osteotomy group: 1140 ml) and fifth day (intercondylar osteotomy group: 469 ml vs. non-intercondylar osteotomy group: 428 ml). Overall, these findings suggest that the amount of blood loss in the intercondylar osteotomy prosthesis was higher than that of the non-osteotomy prosthesis. Thus, using intercondylar osteotomy-free prosthesis for blood loss reduction is favorable. However, no significant difference in blood loss was observed on the third and fifth day after the operation, suggesting that the effect of this factor on blood loss was not obvious after three days. Two treatments can be considered comprehensively.
The effect of intramedullary and extramedullary localization on the amount of blood loss during operation and the influence of different location holes on blood loss after intramedullary positioning operation were not reported locally and abroad. At present, all kinds of existing femoral side manipulation tools are positioned intramedullary. During TKA, the incision of the skin, patellar bursa and turn of the patella should be performed 5 mm above the point of the cruciate ligament; the intramedullary fixation rod should be inserted into the femoral medullary cavity and the osteotomy of the distal femur, anterior condylar condyle, and anterior and posterior oblique planes should be performed sequentially. After the completion of osteotomy, the location hole had no other effect until the end of the operation. However, intraoperative positioning of the hole can be applied for hemostatic treatment through bone plugging or cement plugging. According to plugging condition, the location hole was subdivided into the no-plugging, cementplugging and bone-plugging groups. No other binding factors were involved in the three treatments such that instances of blood loss due to other causes were excluded.
In the no-plugging group, significant differences were observed among the findings on the first, third and fifth day after the operation. Therefore, the treatment of location hole had a certain influence on the total amount of blood loss. Although several procedural steps were present after the operation on the location hole, each step may affect rate of bleeding during the operation. Meanwhile, a uniform standard for the treatment of the location hole remains unavailable. Given that different modes of treatment for the location hole results in varying degrees of blood loss, a careful and attentive performance is recommended.
The effect of bone plugging can be affirmed, and the least amount of blood loss in the bone-plugging group was manifested on the first, third and fifth day after the operation. Furthermore, statistical differences were observed on the first day after operation (bone-plugging group: 545 ml vs. cementplugging group: 612 ml vs. no-plugging group: 744 ml), the third day (bone-plugging group: 989 ml vs. cement-plugging group: 1351 ml vs. no-plugging group: 1293 ml) and the fifth day (bone-plugging group: 128 ml vs. cement-plugging group: 633 ml vs. no-plugging group: 454 ml). The location hole continued to bleed after the positioning operation, and the total amount of blood loss was reduced. In other words, bone plugging actually reduced blood loss, relative to that of noplugging and cement-plugging set-ups. Therefore, bone plugging is most favorable among the methods. However, no statistical difference between the cement-plugging and noplugging groups was observed, and this finding requires further investigation. After the operation of the location hole, bone cement was inserted into the location hole during the installation of the femoral prosthesis. Bleeding seemed to be blocked through cement plugging, although the statistical results showed that bleeding volumes on the first, third and fifth days after operation were non-significantly different from those in the no-plugging group, suggesting that cement plugging did not stop the bleeding.
A number of scholars, such as Woolson [22], compared blood loss volumes between cement and non-cement prosthesis replacement in TKA and in total hip arthroplasty. The results revealed that the blood loss of cement prosthesis was significantly smaller than that of the non-cement type. Bone cement seemed to play a role in hemostasis, although this role was not indicated by the results of this study. According to statistical difference, the amount of blood loss in this study had the following order: bone plugging group<no plugging group=bone plugging group. The rate of blood loss is not reduced after bone cement (polymethyl methacrylate) plugging at the location hole, and the reason for this condition remains unknown, although it might be correlated with the compatibility between bone cement and bone tissues [23]. After the plugging of cancellous bone to the location hole, cement was inserted into the surrounding cancellous bone for the formation of a compact protection that prevents the outflow of blood from the medullary cavity. By contrast, bone cement did not belong to autologous tissues that cannot be plugged in the location hole, and bone cement on the surface of hemorrhagic cancellous bone cannot play a sealing role similar to bone wax.
Therefore, bone plugging is an effective hemostatic method for femoral location hole, and the amount of blood loss in the cement-plugging group was higher than that in the no-plugging group. Therefore, bone plugging should be selected for location holes during surgery because this method can effectively reduce bleeding.
Conclusions
Non-osteotomy prosthesis was better than osteotomy prosthesis in TKA relative to blood loss, except in the third day after operation. The choice of the two prostheses can be comprehensively considered. The performance levels of location holes are indispensable in TKA, and bone plugging in the femoral location hole can result in the reduction of blood loss during surgery. No significant difference between cement plugging and bone plugging was observed with respect to their performance levels.
References
- Kurata K. Assessment of thermal damage in total knee arthroplasty using an osteocyte injury model. J Orthop Res 2017.
- Xiang S, Bie Z, Jiang H. A wireless image acquisition system for artificial knee implant surgeries. Circuits and Systems (MWSCAS) IEEE 2017.
- Schotanus MG, Pilot P, Vos R. No difference in joint awareness after mobile- and fixed-bearing total knee arthroplasty: 3-year follow-up of a randomized controlled trial. Eur J Orthop Surg Traumatol 2017; 1-5.
- Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee 2000; 7: 151-155.
- Cankaya D, Craig JDV. Blood loss and transfusion rates in the revision of unicompartmental knee arthroplasty to total knee arthroplasty are similar to those of primary total knee arthroplasty but are lower compared with the revision total knee arthroplasty. J Arthroplast 2016; 31: 339-341.
- Karam JA, Bloomfield MR, Diiorio TM. Evaluation of the efficacy and safety of tranexamic acid for reducing blood loss in bilateral total knee arthroplasty. J Arthroplast 2014; 29: 501-503.
- Bierbaum BE, Callaghan JJ, Galante JO. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am 1999; 81: 2-10.
- Frisch NB, Wessell NM, Charters MA. Predictors and complications of blood transfusion in total hip and knee arthroplasty. J Arthroplasty 2014; 29: 189-192.
- Hart A, Khalil JA, Carli A. Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors, and thirty-day complication rates. J Bone Joint Surg Am 2014; 96: 1945-1951.
- Newman ET, Watters TS, Lewis JS. Impact of perioperative allogeneic and autologous blood transfusion on acute wound infection following total knee and total hip arthroplasty. J Bone Joint Surg Am 2014; 96: 279-284.
- Milne T. Improved recovery with tranexamic acid: up and walking and rarely talking about blood transfusion. J Peri Anesth Nurs 2017; 32: 9.
- Abdel-Salam A, Eyres KS. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. Bone Joint J 1995; 77: 250-253.
- Zhang Y, Li D, Liu P. Effects of different methods of using pneumatic tourniquet in patients undergoing total knee arthroplasty: a randomized control trial. Irish J Med Sci 2017; 1-7.
- Wang K, Ni S, Li Z. The effects of tourniquet use in total knee arthroplasty: a randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc 2016.
- Papalia R, Zampogna B, Franceschi F. Tourniquet in knee surgery. Br Med Bull 2014; 111: 63-76.
- Cornelius B. Air medical administration of tranexamic acid. J Nurs Off J Soc Trauma Nurses 2017; 24: 30.
- Nawabi DH. Topical tranexamic acid was noninferior to intravenous tranexamic Acid in controlling blood loss during total knee arthroplasty. J Bone Joint Surg 2015; 97: 343.
- Wang H, Shen B, Zeng Y. Blood loss and transfusion after topical tranexamic acid administration in primary total knee arthroplasty. Orthopedics 2015; 38: 1007-1016.
- Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiol 1983; 58: 277-280.
- Pattison E, Protheroe K, Pringle RM. Reduction in haemoglobin after knee joint surgery. Ann Rheum Dis 1973; 32: 582-584.
- Zhang J, Liang W, Wang Y. Early clinical observation of TKA with MB/CR or FB/PS prosthesis. Chinese Orthop J Clin Basic Res 2015.
- Woolson ST. Perioperative blood loss associated with total knee arthroplasty. A comparison of procedures performed with and without cement. J Bone Joint Surg Am 1991; 73: 1574.
- Zhang WQ, Yi HP. Blood compatibility of calcium phosphate cement in repairing bone defects. J Clin Rehab Tissue Eng Res 2009; 13: 545-548.