- Biomedical Research (2013) Volume 24, Issue 3
The use of vacuum-assisted wound closure system for management of difficult wounds.
Cengiz Tavusbay, Haldun Kar, Necat Cin, Erdinc Kamer, Hayri Aksut, Onder Karahalli, Kemal Atahan, Mehmet HaciyanliIzmir Katip Celebi University, Ataturk Research and Training Hospital, Basinsitesi, 35360 Izmir, Turkey
- Corresponding Author:
- Cengiz Tavusbay
Erzene Mah. Sehit Taha Carim Cad. Özveri Sitesi No: 3/1
B Kat:3, Da: 5, Bornova 35050 Izmir, Turkey.
Accepted Date: May 05 2013
Citation: Cengiz Tavusbay, Haldun Kar, Necat Cin, Erdinc Kamer, Hayri Aksut, Onder Karahalli, Kemal Atahan, Mehmet Haciyanli. The use of vacuum-assisted wound closure system for management of difficult wounds.Biomedical Research 2013; 24 (3): 329-336.
Abstract
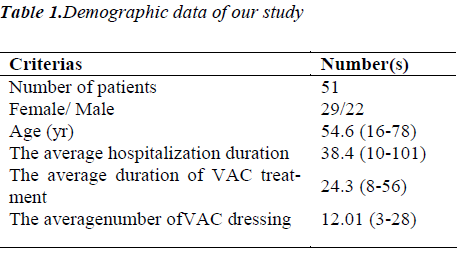
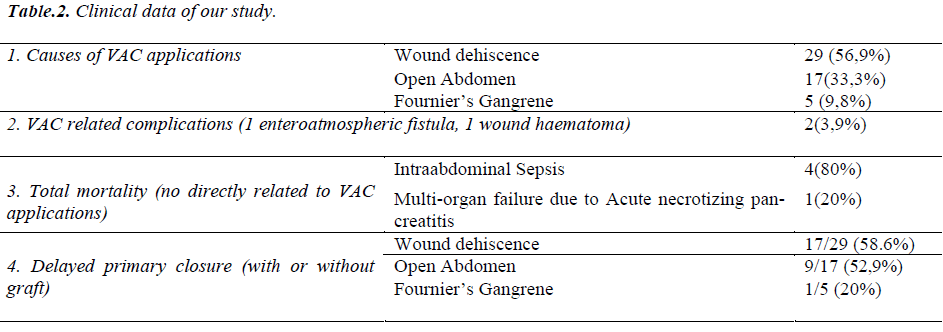
We aimed to present the results of our different clinical practise experience about the treatment and management of extremely difficult wounds using the vacuum-assisted closure system (VAC). In this retrospective study, we analysed the records of 51 consecutive patients who were applied VAC for different clinical practise between 2008 and 2012 at the Izmir Katip Celebi University, Ataturk Education and Training Hospital. There were 51 patients in our study with an average age of 54.6(16-78) years and 22(43.1%) were male, and 29(56.9%) were females. We used VAC system to manage the wound in 29(56.9%) patients with wound dehiscence (with or without fascial necrosis), in 17(33.3%) patients with open abdomen, and in 5(9.8%) patients with Fournier gangrene. The average hospital stay was38.4 days (10-101). The average duration of VAC application was 24.3 (8-56) days. The average number the application of VAC dressingswas 12.01 (3 to 28).Directly VAC related complications (enteroatmospheric fistula and wound haematoma) were seen in two patients (3.9%). A total of 27(52.9%) patients underwent delayed primary or graft closure. In the remaining 19(37.2%) patients, the wound was left to granulate and heal by secondary intention.5 (9.8%) patients died because of complications related to primary disease while on VAC application.We concluded that VAC is an important tool in the armamentarium of the surgeons managing in patients with complex and difficult wounds, particularly, in cases of open abdomen.
Keywords
Fournier’s gangrene, Open abdomen, wound dehiscence, Vacuum assisted closure therapy.
Introduction
During the past decade, technologic advances have a major contribution to the management of acute or chronic wounds. One such treatment modality is the Vacuum- Assisted Closure Therapy System (KCI USA, Inc. San Antonio, Texas). The VAC system has been proved to be effective in evacuating wound fluid, increasing tissue blood flow and tissue oxygen tension, decreasing bacterial contamination, and stimulating granulation tissue formation [1-4]. Therefore, it promotes to more rapid wound healing compared to conventional methods. Recently, this system is widely used to manage for patients with chronic, acute, traumatic, subacute, and dehisced wounds; partial-thickness burns; ulcers (such as diabetic, venous and arterial ulcers or pressure); flaps; and meshed grafts and donor flap sites, and other wounds [5-7]. Additionally, it has been shown to be useful in the patients with enteroatmospheric fistulas, severe abdominal trauma, abdominal compartment syndrome, or complex septic intraabdominal complications (8-10).
Particularly, the open abdomen is often associated by serious clinical problems and management of these wounds can often be challenging. Thus, a temporary dressing for the open abdomen is essential to maintain patient’s stabilization before definitive closure can be achieved safely. VAC has been used for treatment of the open abdomen. The main advantages of the system are simple and easy application, low system-related morbidity, earlier discharge from the intensive care unit and a high rate of primary fascial closure [4,8-10]. In recent years, popularity and indications for use of VAC are constantly increased in various clinical applications.
In this study, we analysed the efficiency and treatment results of VAC system in a total of 51 patients on whom vacuum assisted closure systems were used at the clinic due to various reasons.
Material and Method
Between January 2008 and January 2012, 51 consequtive patients who were treated with vacuum assisted wound closure procedure due to various reasons in our hospital and their charts were retrospectively examined. Demographic characteristics, primary diseases, American Society of Anasthesiology (ASA) scores, definitive surgical operations performed, micro-organisms multiplying in wound culture, hospitalization durations, numbers and durations of vacuum assisted wound closure drapes application, VAC complications and prognosis details of the patients were recorded. Some of these patients were evaluated by calling for examination again at outpatient clinic. Some were contacted by phone and information was obtained.
Technique
Firstly, the basic wound care principles were performed to all wounds prior to the application of VAC therapy. Any devitalized tissue was removed from the wound as soon as possible to prevent any potential source for bacterial growth. Although, additional minor wound debridements were made in the clinic without any analgesic agent in most of our patients, but also, if needed, extended debridement in some patients was made under anaesthesia in the operating room. All debridements were done until a healthy bleeding tissue was encountered.Systemic appropriate antibiotic regimes were administered in all patients.
A VAC system has several essential elements which contains sterile polyethylene sheet and polyurethane sponge, plastic egress tubes, collection reservoirs and an adjustable suction pump capable of intermittent or continuous negatives pressures ranging from -50 mm Hg to -200 mm Hg.
The prepared wound surface was with covered an appropriately- sized polyurethane or polyvinyl alcohol sponge material were used as filling material. Then, the wound is sealed with a transparent self adhesive semi-permeable drape. Connections were inserted through a hole of 2 cm in diameter was cut into the film in the middle of the foam and a TRAC pad was embedded over the hole and attached to an adjustable vacuum pump by means of a suction tube and the system was started. A collection reservoir is changed weekly or upon filling capacity. The pump pressure adjusted between 75-200 mm Hg depending on patient's level of tolerance. As a standard, the responsible surgeon determined the amount of negative pressure and evaluated the progression for the wound every two to three days.
In open abdomen cases, the most important components of VAC system are polyethylene sheet and polyurethane sponge. Firstly, the polyethylene sheet with the foam was cut into appropriate size. The sheet was tucked between the parietal peritoneum and the bowel, thus preventing the formation of adhesions between the abdominal wall and the bowel. After polyurethane sponge was then placed moderately smaller than the fascial dehiscence to ensure adequate traction on the fascial and wound edges. The foam, including the surrounding skin, was then covered with the adhesive tapes to ensure complete sealing. A 2- cm hole was cut in the middle of the foam to position the TRAC pad suction device. After connection to the canister of the vacuum pump, a continuous negative pressure between 50 and 175 mm Hg was established. Closure of the fascia was performed when feasible. In some of the open abdomen cases included in our series, VAC application was performed immediately after surgical operation.
Results
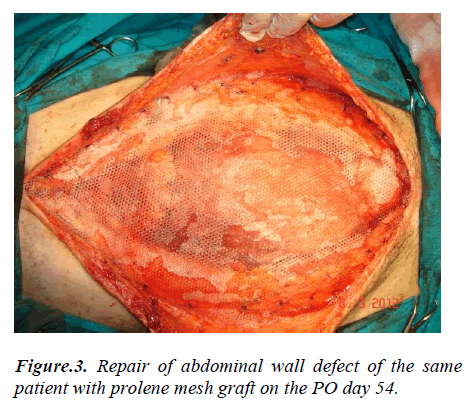
Demographic data of our patients are summarized in Table 1. Of the patients, 29 (56.9%) were female, and 22 (43.1%) were male and mean age was 54.6 (16–78). Mean hospitalization duration time was 38.4 (10-101) days, mean VAC application period was 24.3 days (8-56) and mean numbers of VAC application were 12.01 (3- 28). VAC was used in 29 cases (56.9%) for severe wound dehiscence developing after abdominal operations, in 17 cases (33.3%) open abdomen due to various reasons, in 5 cases (9.8%) for Fournier gangrene (Table 2).
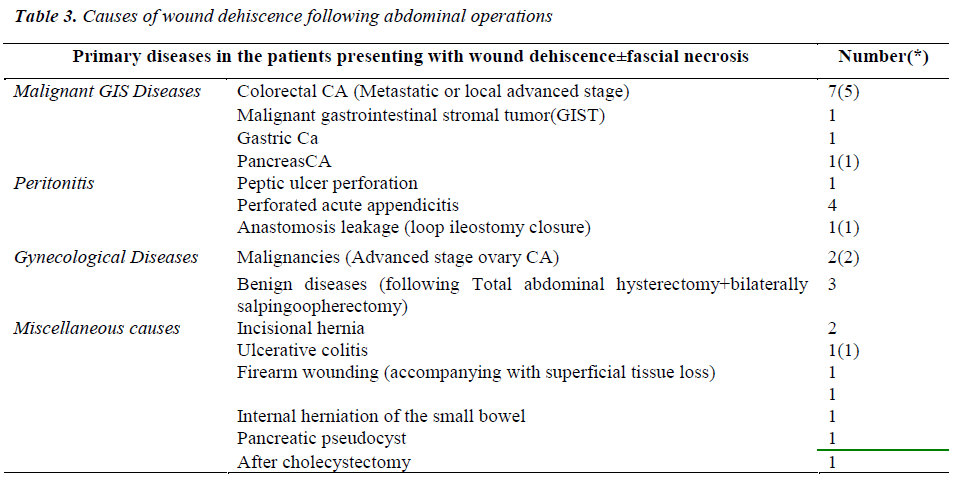
10 of 29 patients with wound dehiscence were operated due to malignant gastrointestinal disease, and 6 patients due to localized or generalized peritonitis arising from different causes, 5 patients due to gynaecological diseases, and 8 patients due to various other reasons. 10 of these patients (34.4%) also had fascial necrosis developing subsequent to abdominal procedure (Table 3).
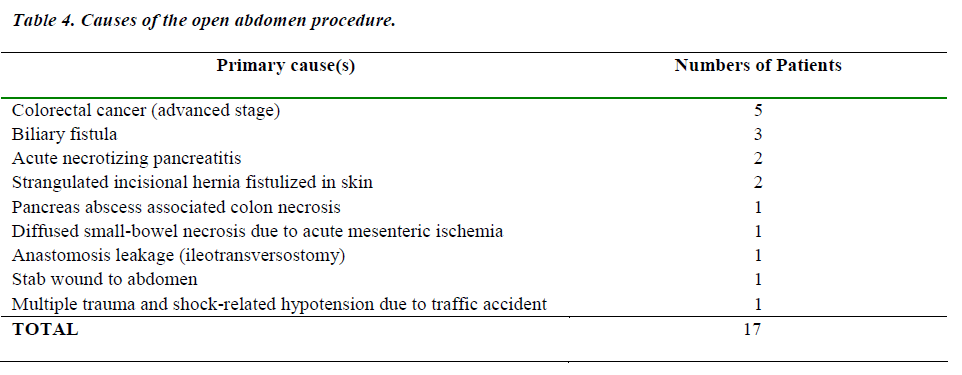
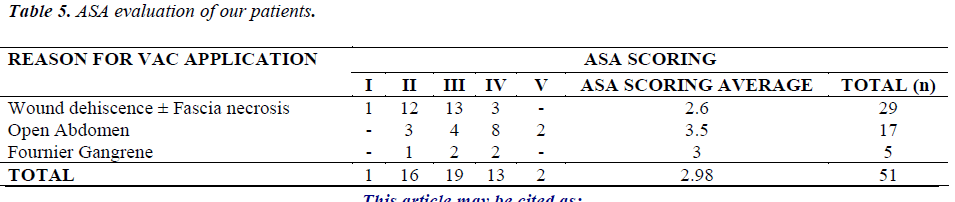
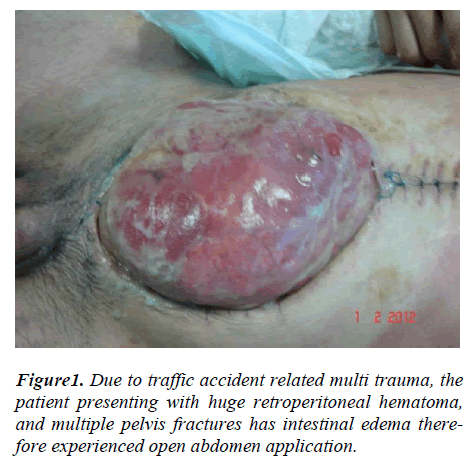
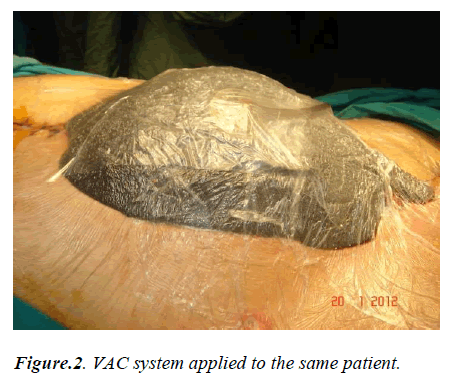
Open abdomen procedure was performed in total 15 patients with or without intraabdominal infection with sepsis due to various causes, in 1 patient due to stab wound injury and in 1 patient with multiple traumas due to severe traffic accident (table 4). All the patients subjected to open abdomen are critical patients that must be followed in intensive care unit most of whom had additional adherent comorbidity factors such as advanced age and systemic disease. The youngest patient (16 years old) of the series had severe multiple fractures at pelvis and giant retroperitoneal hematoma due to trauma and operated in a severe shock condition and remained in intensive care unit for several days. In this patient severe intestinal edema was observed at post-operative period and open abdomen was performed due to the fact that abdomen could not completely be closed. Another trauma patient who had multiple organ damage related to stab wound and had both preoperative and per-operative severe hemorrhagic shock status. It was possible to make repair successfully with graft at both cases after few months.
Mean ASA score in our series was 2.98 (1-5) (Table 5). ASA score was determined to be higher in patients undergoing open abdomen in particular (3.5).
17 of 29 patients (58.6%) with wound dehiscence underwent delayed primary or graft closure operation following wound shrinking. Wounds of other patients spontaneously closed.
In 9 of 17 patients (52.9%) undergoing open abdomen, VAC application was continued until the wound became ready for definitive surgical operation. In these patients, defect in abdominal wall was closed primarily or by using graft. In three patients (17.6%), wound was spontaneously closed. In five patients with Fournier gangrene, wounds were closed primarily (one patient) or by leaving to secondary recuperation (Table 2).
Results of culture and antibiogram conducted according to status of primary disease and/or wound were evaluated and patients were administered wide spectrum antibiotics. The most frequently seen micro-organisms in the culture were staphylococci (including MRSA), streptococci, gram negative enterobacteria, E. coli and pseudomonas, respectively.
In 2 of 51 patients (3.9%) VAC associated complication occurred. One patient had bleeding wound and hematoma was developed, despite local treatment, it did not recover and VAC was ceased. In our series, VAC system was applied in 5 patients with Fournier gangrene cases. 5 patients had type 2 diabetes mellitus. One of the patients had additional immune system disease and another patient had chronic obstructive pulmonary disease (COPD) history. In 2 of the patients colostomy was required additionally. In these patients, wound debridements were generally performed under general anaesthesia and no grafts were required for wound closure.
In another patient, secondary to VAC application, fine intestinal fistula was observed. That patient was operated urgently and primary anastomosis after resection was performed. None of the patients had severe pain that would lead to ceasing VAC application.
In 5 (29.4%) out of 17 patients undergoing open abdomen application due to primary diseases independent from VAC application, mortality occurred. Mortality causes were intraabdominal sepsis developing in four patients who were operated due to various diseases in postoperative period and in one case acute necrotizing pancreatitis related multi organ failure.
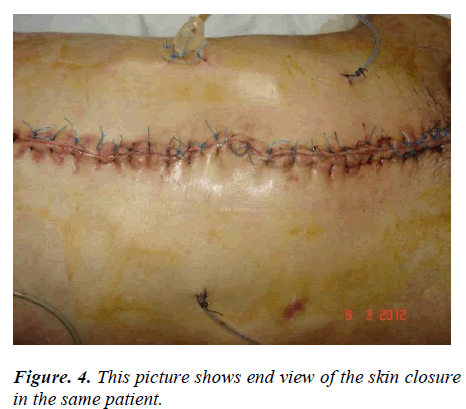
When generally evaluated, with VAC application in patients included in our series considerable shrinking at wound sites of patients with wound dehiscence and Fournier gangrene in particular, acceleration in the granulation tissue development and reduction in wound secretion were observed. Additionally, in open abdomen cases, there was substantial contribution for management of abdominal wound depending on primary disease and gaining time for delayed primary repair (Figure 1-4).
Discussion
It was suggested that vacuum assisted wound closure led to changes in physiological and chemical medium of wound, thereby accelerating the recovery of acute and chronic wounds with various mechanisms [1-4,11]. Morykwas et al reported that sub-atmospheric pressures of 125 mm Hg resulted in a fourfold increase in blood flow using an excisional wound model in pigs [1]. With mechanic stress formed in the cells of wound surface, cellular proliferation increases in tissue, various cytokines (tumour necrotizing factor and metalloprotease) and cytochemical modifications occur, as a result, tissue migration, granulation tissue formation and wound recovery are accelerated. Additionally, it was reported that proteases inhibiting wound recovery were absorbed and removed, numbers of bacteria were reduced in the infected tissue and local edema in the interstitial tissue is decreased [1-3,10-15].
VAC wound system reduces nurse and physician care in patients particularly with excessive discharge from wound site and / or severe wounds with challenging treatment. Since VAC system replacement is every 48-72 hours, it facilitates wound care, and malodor at wound site are precluded. Facilitation of wound care and reducing frequency of dressing is of great importance in patients (such as those patients with Fournier gangrene, diabetic and obesity) who need replacement of their dressing several times in a day, which is very difficult to replace. Elimination of malodor arising from necrotic tissues and it’s being a closed system provided significant comfort for both patients and the team responsible for patient care. Thanks to miniature vacuum device recently developed, a patient can be mobilized more comfortably. Other than those patients remaining in intensive care unit at the clinic or patients immobilized at bed due to various reasons, whom VAC system was applied were supported to be mobilized and it was substantially realized. Another important point observed in our study is that wound shrunk and controlled with application of this system and vacuum impact. Particularly in patients with intact fascia, it was observed that wound recovered faster under pressures between 100-150 mm Hg. Subjectively when our experience increased in wound care, we found out that pressure over 130 mmHg in average is more effective in patients with intact fascia who had wound dehiscence.
When demographic characteristics of our study are evaluated, it draws attention that wound complications were developed particularly in older patients with systemic disease who underwent major abdominal surgical opera-tion. Although an appropriate surgical operation complying with meticulous surgical procedures was performed on patient population in question, there is still probability of development of severe wound complications and it was observed that VAC provides serious contributions against wound complications occurring at such patients.
During VAC applications, applying dressing on wound site fully is rather important. Because, air flow on wound site arising from lack of appropriate negative pressure causes necrotic eschar thereby prevents the exudate drainage and wound contraction. As a result, infection develops and this delays wound recovery.
Wound dehiscence occurring in most of the patients participating in this study is a common scenerio, relatively frequently encountered at clinics where major abdominal surgical operations are performed. When we examined demographical characteristics of a total of 29 patients included in this group of our series, mean ASA score was 2.98 and mean age was 54.6. Of these patients included in this group, 14 patients were operated on due to malignancies. Consequently, as expected, wound dehiscence is observed specifically in old patients with weak immunological defence mechanisms and/or comorbidity.
The second largest group of our series consists of open abdomen cases. Management of the open abdomen which is done in critical ill patients with intra-abdominal hypertension (IAH) and/or abdominal compartment syndrome (ACS) can often be significant challenging in surgical clinics. A temporary dressing for the open abdomen is essential for a variable period before definitive closure can be done safely. Although, it can be used the ‘‘Bogota bag,’’ saline-soaked gauze dressings or towel pack, absorbable or permanent (polytetrafluoroethylene) mesh, or other synthetic materials these methods have a lot of disadvantages (e.g., increased infection risk, intensive nursing, time consuming dressing changes, delayed definitive closure) [16]. In our study, open abdomen technique was performed in 15 cases for intraabdominal infection and/or intraabdominal sepsis due to various reasons and in 2 patients due to severe multi-trauma. Berker et al has published their results over the last 15 years of using the VAC method and reported a 68% delayed primary fascial closure and a 5% fistula rate [17]. In our series, the ratio of delayed primary fascia closure was 52.9% and fistula development ratio was 1.9%.
Although VAC system has many advantages as told above and data obtained at our series, there exists probability of complication development. However, VACspecific morbidity was rather low. The most common is mild skin irritation from contact with the foam (18). In our study, we didn't observe this complication in any of our patients.
The most severe complication is enteroatmospheric fistula development. In the literature, the frequency of enteroatmospheric fistula development ranged from 0 to 20 percent [16,19,20]. The rate of fistulation might be higher in patients with abdominal sepsis compared with trauma patients. Rao et al reported an enterocutaneous fistula rate of 20% in a group of patients with predominantly abdominal sepsis. As a result, they concluded that VAC system should be used with caution in the patients with abdominal sepsis [18]. In our series, we observed development of enteroatmospheric fistula in one patient. This patient had severe cardiac and lung disease besides advanced stage sigmoid colon cancer. In our opinion, rather than VAC application of enteroatmospheric fistula development in this case, small intestine wall which became rather fragile easily perforated depending on tissue oxygenation and malnutrition in addition to adjuvant systemic diseases in addition to patient’s primary malign disease, keeping VAC pressure relatively high and not adequate formation of granulation disuse.
Other VAC-related complications reported included pain, bleeding, progressing of infection, generalized edema (anasarca), necrosis at the fascial edges, blister under the adhesive tape, and prolapsing small bowel between the VAC edge and the fascial/skin edge, bad odour from wound [21]. To prevent these complications, eligible patient selection, close follow up of the patient by surgeon in charge and good planning of the treatment are important. While applying first negative pressure on wound, gradual increase of pressure might prevent pain. In our series, although first pressure application varied from case to case, generally we started low and in subsequent dressings vacuum pressure was adjusted by physician in charge by considering the patient tolerance and wound status. Local hemorrhage which may be formed during dressing replacement, observed more frequently during cases when granulation tissue develops fast, can generally be taken under control with tamp by changing dressings frequently. In the series submitted out of these complications only hemorrhage in one patient was observed, upon failure to manage it despite all precautions, VAC treatment was ceased.
Although in the literature it is reported as one of important disadvantages of this method is needing 1-2 hour period of time for system setup, during recent applications this duration was 10-15 minutes at system changes performed by technicians trained under responsibility of specialist physicians.
In the literature, it has been reported that the VAC therapy has several contraindications. The VAC system should not be applied in wounds associated with malignancies, since it has possibility to increase blood flow and stimulate cellular proliferation within the wound. It can be hazardous VAC dressings near arteries or veins for risk of extensive blood loss. Similarly, VAC can be caused bleeding in patients with coagulation abnormalities or patients or/with active bleeding [22,23].
When our series is evaluated together with literature, another aspect attracting attention is length of hospitalization due to primary diseases and/or wound complications of the patients. Mean hospitalization was 38.4 (10-101) days. As stated above, a great majority of these patients were old and that they had serious additional systemic diseases and they spent most of their hospitalization in intensive care unit. A small number of patients included in the series are complicated cases with developed very severe wound complications even if their primary diseases are benign. For example, in a young patient with morbid obesity and operated due to gangrenous perforated appendicitis had wound dehiscence and subcutaneous infection could not be controlled for days despite classical wound care and antibiotherapy applied. In this patient, wound was taken under control within a short time later with VAC application.
There is no certain data about optimal duration of VAC application. This duration varies from patient to patient and wound status as understood from our series. Mean VAC application duration in our series was 24.3 days (8- 56) and mean number of VAC application was 12.01 (3- 28). With increasing experiences, we found out that VAC system is used more.
As a matter of fact, number of VAC applications progressively increased since it started, and this number reached to top number during last year.
We concluded that VAC therapy is an important tool in the armamentarium of surgeons to manage patients with complex and difficult wounds, particularly, in cases of open abdomen. VAC application should individually be evaluated for each case. As our experience related to VAC use in connection with wound care increases, outcomes are delivered, borders of VAC application and its advantages, results will be understood better.
References
- Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997;38:553-562.
- BanwellPE, Musgrave M. Topical negative pressure therapy: mechanisms and indications. Int Wound J 2004;1:95–106.
- Morykwas MJ. Faler BJ, Pearce DJ, Argenta LC. Effects of varying levels of subatmospheric pressure on the rate of granulation tissue formation in experimental wounds in swine. Ann Plast Surg. 2001;47:547-551.
- Scheufler O, Peek A, KaniaNM, Exner K. Problemadapted application of vacuum occlusion dressings: case report and clinical experience. Eur J Plast Surg 2000;23:386-390.
- Willy C, Voelker HU, Engelhardt M. Literature on the subject of vacuum therapy review and update. Eur J Trauma Emerg Surg 2007;1:33-39.
- Scherer LA, Shiver S, Chang M, Meredith JW, Owings JT. The vacuum assisted closure device: a method of securing skin grafts and improving graft survival. Arch Surg. 2002;137:930-933.
- Subramonia S, Pankhurst S, Rowlands BJ, Lobo DN. Vacuum-assisted closure of postoperative abdominal wounds: a prospective study. World J Surg. 2009;33:931-937.
- Teixeira PG, Salim A, Inaba K, Brown C, Browder T, Margulies D, Demetriades D. A prospective look at the current state of open abdomens. Am Surg 2008;74:891-897.
- Marinis A, Gkiokas G, Anastasopoulos G, Fragulidis G, Theodosopoulos T, Kotsis T, Mastorakos D, Polymeneas G, Voros D Surgical techniques for the management of enteroatmospheric fistulae. Surg Infect. 2009;10:47-52.
- Miller PR, Meredith JW, Johnson JC, Chang MC. Prospective evaluation of vacuum-assisted fascial closure after open abdomen: planned ventral hernia rate is substantially reduced. Ann Surg 2004;239:608-614.
- Antony S, Terrazas S. A retrospective study: clinical experience using vacuum-assisted closure in the treatment of wounds. J Natl Med Assoc. 2004;968:1073-1077.
- Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg. 2005;29:219-226.
- Greene AK, Puder M, Roy R, Arsenault D, Kwei S, Moses MA, Orgill DP. Microdeformational wound therapy: effects on angiogenesis and matrix metalloproteinases in chronic wounds of 3 debilitated patients. Ann Plast Surg 2006;56:418-422.
- Kamolz LP, Andel H, Haslik W, Winter W, Meissl G, Frey M. Use of subatmospheric pressure therapy to prevent burn wound progression in human: first experiences. Burns 2004;30:253-258.
- Obdeijn MC, de Lange MY, Lichtendahl DH, de Boer WJ. Vacuum-assisted closure in the treatment of poststernotomy mediastinitis. Ann Thorac Surg 1999;68:2358-2360.
- De Franzo AJ, Marks MW, Argenta LC, Genecov DG. Vacuum-assisted closure for the treatment of degloving injuries. Plast Reconstr Surg. 1999;104:2145-2148.
- Barker DE, Green JM, Maxwell RA, Smith PW, Mejia VA, Dart BW, Cofer JB, Roe SM, Burns RP. Experience with vacuum pack temporary abdominal wound closure in 258 trauma and general and vascular surgical patients. J Am Coll Surg. 2007;204:784-793.
- Rao M, Burke D, Finan PJ, Sagar PM. The use of vacuum assisted closure of abdominal wounds: a word of caution. Colorectal Dis 2007;9:266-268.
- Labler L, Zwingmann J, Mayer D, Stocker R, Trentz O, Keel M. V.A.C. abdominal dressing system. Eur J Trauma 2005;5:488-494.
- Starr-Marshall K. Vacuum-assisted closure of abdominal wounds and entero-cutaneous fistulae: the St Marks experience. Colorectal Dis 2007;9:573.
- Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg. 2005;29:219-26.
- Webb LX. New techniques in wound management: vacuum-assisted wound closure. J Am Acad Orthop Surg. 2002;10:303-11.
- Argenta LC, Morykwas MJ, Marks MW, De Franzo AJ, Molnar JA, David LR. Vacuum-assisted closure: state of clinic art. Plast Reconstr Surg. 2006;117(7 Suppl):127S-142S.