Research Article - Research and Reports in Gynecology and Obstetrics (2017) Research and Reports in Gynecology and Obstetrics (Special issue 1 - 2017)
The use of hysteroscopic morcellation in the outpatient management of retained products of conception.
Rebecca Mallick* and Bronwyn MiddletonWestern Sussex Hospital NHS Foundation Trust, Chichester, UK
- *Corresponding Author:
- Dr Rebecca Mallick
Western Sussex Hospital
NHS Foundation Trust
St Richards Hospital
Chichester, UK
Tel: 07411617143
E-mail: rmallick@doctors.org.uk
Accepted Date: March 10, 2017
Citation: Mallick R, Middleton B. The use of hysteroscopic morcellation in the outpatient management of retained products of conception. Res Rep Gynaecol Obstet. 2017;1(1):17-15
Abstract
Retained products of conception (RPOC) can prove challenging to manage, particularly in cases where conventional treatment options have failed. There are well-documented risks associated with recurrent dilatation and curettage, even when done under ultrasound guidance. Hysteroscopic resection has been described in the literature as an alternative surgical treatment option, but again this is not without risks. A further alternative treatment option is the use of hysteroscopic morcellation, which is already well established and successfully used in the outpatient management of uterine pathologies, such as endometrial polyps and fibroids. Like formal hysteroscopic resection, it allows targeted removal of the retained products under direct vision, but instead uses a mechanical blade thus avoiding the use of heat energy and the potential risks of fluid overload and visceral heat injury. We present a retrospective case series of 9 cases where hysteroscopic morcellation was used to resect RPOC in the outpatient setting in cases where standard management options had failed. Hysteroscopic morcellation was found to be a safe and effective means of treating persistent RPOC with complete resection and symptom resolution in 100% of cases and no intraoperative or postoperative complications noted. The procedure was quick and well tolerated by patients in the outpatient setting with low pain scores and thus should be considered as a potential alternative surgical treatment option in the management of RPOC, particularly when other standard treatment options have failed.
Keywords
Hysteroscopic morcellation, Hysteroscopy, Submucosal fibroids, Retained products of conception
Introduction
Over the past decade there have been significant advances in hysteroscopy and a movement towards operative outpatient hysteroscopy techniques. Numerous studies have highlighted the efficacy, safety and patient acceptability of many operative outpatient procedures [1,2]. One such technique is the use of hysteroscopic morcellation devices, which allow direct visualisation of the intrauterine pathology, namely uterine polyps and sub mucosal fibroids, and allows morcellation of the tissue and complete removal under vision.
Retained products of conception (RPOC) are a relatively common occurrence and are estimated to complicate 1% of pregnancies [3]. They most commonly present following miscarriage and termination of pregnancy (TOP) and less commonly following spontaneous vaginal delivery (SVD) and caesarean sections (CS). Standard treatment options include conservative, medical and surgical management with varying documented success rates of between 13-96% [4-7]. However in cases where standard management options have failed, subsequent management of these cases of persistent RPOC can be problematic with significant short and long-term complications such as infection, adherent tissues and intra-uterine adhesion formation [8] and there is a paucity of data regarding the best management option.
Hamerlynck et al. first described the use of hysteroscopic morcellation in the management of placental remnants in 2013 [9]. The present study, although a much smaller case series, appears to be the first of its kind in the UK and also the first to be purely performed in an outpatient setting. The aims of this study were to assess the use of hysteroscopic morcellation in the outpatient setting, with regards to efficacy, safety and patient acceptability, in the management of RPOC in cases where standard management options had failed.
Methods
This retrospective study was performed over a 6-month period (January 2016-June 2016) in a district general hospital setting, which already had an established outpatient hysteroscopy setup and expertise in the use of hysteroscopic morcellation for the removal of fibroids and polyps. Inclusion criteria in offering women hysteroscopic resection included: on-going symptoms suggestive of RPOC such as persistent bleeding, previous failed conservative, medical or surgical management, a transvaginal ultrasound scan (TVS) suggestive of RPOC using standard diagnostic criteria and patient acceptability to have the procedure performed in an outpatient setting. Exclusion criteria included suspected molar pregnancies and patients unable to tolerate an outpatient procedure. Patients were fully counselled regarding the option of hysteroscopic morcellation and other treatment options available in cases of persistent RPOC such as repeat medical treatment if appropriate, dilatation and curettage under ultrasound guidance or hysteroscopic resection under general anaesthetic. Two experienced gynaecologists using the same standard hysteroscopic practice performed the procedures. The procedure was performed in the outpatient setting with each patient given a 30-minute appointment slot. All patients were advised to take oral analgesia (paracetamol and ibuprofen) unless contraindicated 2 hours before the procedure and given a standard cervical block prior to cervical dilatation. Cervical ripening agents and antibiotics were not given in any of the cases. The MyoSure intrauterine mechanical morcellator and a 6mm MyoSure hysteroscope (Hologic, Marlborough) were inserted under direct vision following dilatation of the cervical OS to hegar 6. Normal saline was used for distension of the uterine cavity and fluid balance was closely monitored using the Aquilex fluid control system (Hologic, Marlborough). Outcome measures included pain scores, intraoperative complications (uterine perforation, haemorrhage, fluid deficit greater than 2500 ml), postoperative complications (infection, admission following procedure, re-admission rates), complete visual resection and patient symptom resolution. All morcellated specimens were sent for histological assessment. The patient demographics (age, BMI, parity) and procedure details were collected and the data was analysed using SPSS (version 22). Median and range were used to describe non-normal data and mean +- standard deviation (SD) and 95% confidence intervals were used to describe normal distributed data. Ethical approval and funding were not required for this study.
Results
Over a 6-month period 9 women underwent hysteroscopic morcellation of RPOC. On-going/ irregular bleeding was the presenting complaint in all 9 patients and all had a confirmed diagnosis of RPOC made pre-operatively using TVS. RPOC was diagnosed following miscarriage in 6 cases (66.7%), SVD in 2 cases (22.2%) and CS in 1 case (11.1%).
All women opted for hysteroscopic morcellation following detailed counselling and after failure of standard management options for RPOC. 4 (44.4%) had originally opted for conservative management, 3 (33.4%) had underwent medical management and 2 (22.2%) had underwent a surgical evacuation (vacuum aspiration under general anaesthetic). The average duration between the end of pregnancy and the hysteroscopic morcellation procedure was 58 days and the size of RPOC removed was between 24-31 mm. Patient characteristics are summarised in Table 1. All procedures were performed in the outpatient setting. A deep cervical block was given to all patients accompanied with oral analgesia in 44%.
Table 1. Baseline patient characteristics.
| Variable | Value |
|---|---|
| Age (years) | 31 ± 3.68 (28.62-34.27) |
| BMI | 24.89 ±4.8 (21.19-28.58) |
| Parity | 1 (0-2) |
| Initial pregnancy | |
| Miscarriage | 6 (66.7%) |
| Spontaneous vaginal delivery | 2 (22.2%) |
| Caesarean Section | 1 (11.1%) |
| Previous treatments | |
| Failed conservative management | 4 (44.4%) |
| Failed medical management | 3 (33.4%) |
| Failed surgical management | 2 (22.2%) |
| Interval between end of pregnancy and morcellation procedure (days) | 58 ± 27.89 (36.56-79.44) |
| Ultrasound estimate of retained products of conception (mm) | 27.78 ± 4.44 (24.37-31.19) |
Data presented as mean ±SD (95%CI), median (range) or absolute number (%)
The procedure was well tolerated with average reported pain scores of 2.67 out of 10 and a mean procedure time of 5.78 minutes. No intra-operative or post-operative complications were noted in any of the procedures. Complete removal of the RPOC with restoration of a normal uterine cavity was achieved in 100% of cases with histological confirmation of RPOC made in 89% of cases. In the remaining case histology reported chronic endometritis, but no clear RPOC were seen. Symptom resolution was noted in all patients. Operative characteristics are summarised in Table 2.
Table 2. Operative characteristics.
| Variable | Value |
|---|---|
| Analgesia | |
| Cervical block alone | 5 (55.6%) |
| Cervical block and oral analgesia | 4 (44.4%) |
| Procedure time (mins) | 5.78 ± 1.48 (4.64-6.92) |
| Pain score (1-10) | 2.67 ± 1.41 (1.58-3.75) |
| Intraoperative complications | 0 |
| Postoperative complications | 0 |
| Restoration of normal cavity at end of procedure | 9 (100%) |
| Resolution of symptoms | 9 (100%) |
Data presented as mean ± SD (95%CI), median (range) or absolute number (%)
Discussion
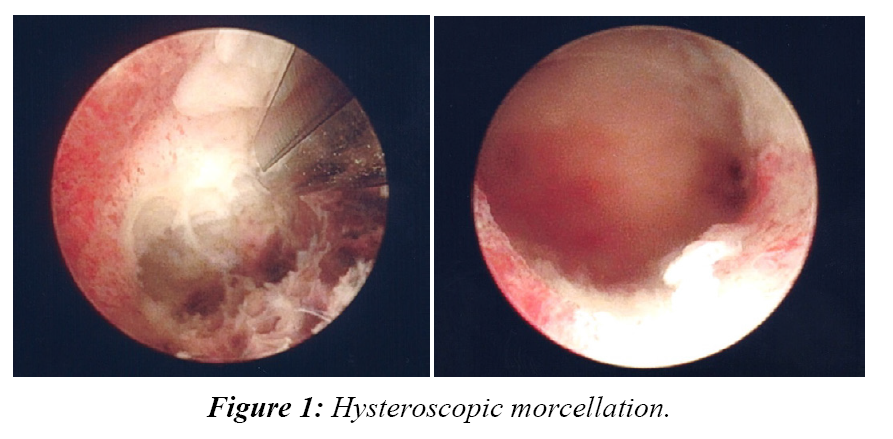
Hysteroscopic morcellation appears to be an efficacious and safe alternative surgical treatment option for the removal of RPOC, particularly in cases of persistent RPOC where initial treatments have failed, with complete removal and symptom resolution in all of our patients (Figure 1).
The standard technique for the surgical removal of RPOC is generally performed by dilatation and curettage using vacuum aspiration, often combined with the use of ultrasound guidance in cases of persistent RPOC. Although well established this procedure is associated with the potential risks of uterine perforation, incomplete removal of products and intra-uterine adhesion formation due to the blind technique and the potential for damage to the surrounding healthy endometrial tissue [3,8].
An alternative to blind curettage is direct visualisation by hysteroscopy and resection using monopolar or bipolar energy. The benefits of this, when compared to blind dilatation and curettage, have been clearly documented in the literature and include a more complete resection with better restoration of the uterine cavity [10], a reduced risk of persistent RPOC [3], less damage to surrounding endometrial tissue and hence a reduced risk of intra-uterine adhesions [11] and overall improved subsequent reproductive outcomes [12,13]. However hysteroscopic resection does have its limitations. Firstly these procedures need to be performed in a theatre setting and carry the risks of general aneasthetic as well the cost implications of theatre time and inpatient stay. Due to the size of a standard resectoscope, dilatation up to 10 mm is required and this carries the potential increased risk of cervical trauma and uterine perforation when compared to standard diagnostic hysteroscopy [14]. Although extremely rare the use of heat energy also carries a potential risk of visceral injury with reports in the literature of bowel injuries requiring exploratory laparotomy [15]. The use of monopolar energy and glycine as a distension medium also carries the well-documented risks of fluid overload and hyponatremia, occurring in approximately 0.2% of operative hysteroscopy cases [14], although this can largely be offset now with the use of bipolar technology and normal saline and in some cases hysteroscopic resection of RPOC can be performed without the use of energy using a “cold loop” technique.
Hysteroscopic morcellation confers the benefits of direct visualisation, while avoiding many of the potential risks associated with standard hysteroscopic resection. First and foremost the procedure is performed using a smaller hysteroscope with minimal dilatation and is very well tolerated by patients in the outpatient setting as highlighted by our study, with low average pain scores reported. This avoids the need for general anaesthesia and is more cost effective with regards to theatre time and inpatient stay. Our findings are in keeping with the wider literature which highlights the high patient acceptability of operative outpatient hysteroscopic procedures [2]. The procedure itself is also quick, again as highlighted by our study and in keeping with the wider literature [9].
Hysteroscopic morcellation also avoids the use of heat energy and uses a small mechanical side blade to morcellate the tissue hence avoiding the potential for visceral heat injury. In our case series no intraoperative or postoperative complications were observed and this is again in keeping with the wider literature. In a series of 255 hysteroscopic morcellation procedures reported by Arnold et al. [1], no intraoperative complications were noted. Haber et al. [16] also reported an overall low complication rate of <0.1% when reviewed over a 9 year period, which is nearly a ten-fold reduction in the complication rate of 0.95% reported in a meta-analysis of 2515 patients undergoing hysteroscopic resection [14].
The direct visualisation and use of a small mechanical blade also allows targeted removal of the RPOC and thus avoids deeper resection into the myometrium and surrounding normal endometrium, which may carry a theoretical reduced risk of subsequent intrauterine adhesions [17].
Another key benefit of the hysteroscopic morcellation technique is the clear operative view, which can be maintained throughout the whole procedure with minimal scope re-insertions. The morcellated tissue is continually suctioned out of the operative field, removing the need for multiple scope insertions and retrieval of the resected “chips” that can occur in hysteroscopic resection.
One of the fundamental limitations of this study is the small sample size and its retrospective nature, but the results in general appear to be in keeping with the larger studies of hysteroscopic morcellation undertaken in a general anaesethetic setting [1,9]. The average size of RPOC removed was 27 mm (range 24-31 mm) and no complications were encountered, however caution must be used when the RPOC are larger than this due to the potential risks of bleeding. It may be prudent therefore to carry out the procedure in cases of RPOC greater than 40 mm in the inpatient setting under general anaesthetic. With regards to cost effectiveness the initial outlay may be costly in a units where hysteroscopic morcellation is not currently used, however long term cost savings would certainly be made with regards to inpatient stay and theatre/anaesthetic time. Our results are certainly encouraging with regards to its use in an outpatient setting in the management of RPOC, however to validate these a larger prospective study or randomised controlled trial would be beneficial in adding further evidence to this field particularly with regards to patient acceptability, cost effectiveness and long term fertility effects.
Conclusion
Our series highlights that hysteroscopic morcellation is a useful alternative treatment option in the surgical removal of persistent RPOC, where standard management options have failed. It is very well tolerated by patients in the outpatient setting with minimal dilatation needed and complete resection achievable under direct vision, thus avoiding the need for general anaesthetic and formal hysteroscopic resection. It is a safe and quick procedure with no complications noted in our series. However its small numbers limits this case series and further research and evidence is needed to validate our findings particularly in the outpatient setting.
Compliance with Ethical Standards
No funding was provided for this research.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Arnold A, Ketheeswaran A, Bhatti M, et al. A prospective analysis of hysteroscopic morcellation in the management of intrauterine pathologies. J Minim Invasive Gynecol. 2016;23(3):435-41.
- Marsh FA, Rogerson LJ, Duffy SR. A randomised controlled trial comparing outpatient versus daycase endometrial polypectomy. BJOG. 2006;113(8):896-901.
- Hooker AB, Aydin H, Brolmann HA, et al. Long-term complications and reproductive outcome after the management of retained products of conception: a systematic review. Fertil Steril. 2016;105(1):156-64.
- Condous G, Okaro E, Bourne T. The conservative management of early pregnancy complications: A review of the literature. Ultrasound Obstet Gynecol. 2003;22(4):420-30
- Trinder J, Brocklehurst P, Porter R, et al. Management of miscarriage: Expectant, medical, or surgical? Results of randomised controlled trial (miscarriage treatment (MIST) trial). BMJ. 2006;332(7552):1235-40.
- Saraswat L, Ashok PW, Mathur M. Medical management of miscarriage. The Obstetrician & Gynaecologist. 2014;16(2):79-85.
- Sotiriadis A, Makrydimas G, Papatheodorou S, et al. Expectant, medical, or surgical management of first-trimester miscarriage: A meta-analysis. Obstet Gynecol. 2005;105(5):1104-13.
- Hooker AB, Lemmers M, Thurkow AL, et al. Systematic review and meta-analysis of intrauterine adhesions after miscarriage: prevalence, risk factors and long-term reproductive outcome. Hum Reprod Update. 2014;20(2):262-78.
- Hamerlynck TW, Blikkendaal MD, Schoot BC, et al. An alternative approach for removal of placental remnants: Hysteroscopic morcellation. J Minim Invasive Gynecol. 2013;20(6):796-802.
- Golan A, Dishi M, Shalev A, et al. Operative hysteroscopy to remove retained products of conception: Novel treatment of an old problem. J Minim Invasive Gynecol. 2011;18(1):100-3.
- Smorgick N, Barel O, Fuchs N, et al. Hysteroscopic management of retained products of conception: Meta-analysis and literature review. Eur J Obstet Gynecol Reprod Biol. 2014;173(1):19-22.
- Ben-Ami I, Melcer Y, Smorgick N, et al. A comparison of reproductive outcomes following hysteroscopic management versus dilatation and curettage of retained products of conception. Int J Gynaecol Obstet. 2014;127(1):86-9.
- Rein DT, Schmidt T, Hess AP, et al. Hysteroscopic management of residual trophoblastic tissue is superior to ultrasound-guided curettage. J Minim Invasive Gynecol. 2011;18(6):774-8.
- Jansen FW, Vredevoogd CB, van Ulzen K, et al. Complications of hysteroscopy: a prospective, multicenter study. Obstet Gynecol. 2000;96(2):266-70.
- Pasini A, Belloni C. Intraoperative complications of 697 consecutive operative hysteroscopies. Minerva Ginecol. 2001;53(1):13-20.
- Haber K, Hawkins E, Levie M, et al. Hysteroscopic morcellation: Review of the manufacturer and user facility device experience (MAUDE) database. J Minim Invasive Gynecol. 2015;22(1):110-4.
- Harpham M, Abbott J. Use of a hysteroscopic morcellator to resect miscarriage in a woman with recurrent Asherman's syndrome. J Minim Invasive Gynecol. 2014;21(6):1118-20.