Review Article - Research and Reports in Gynecology and Obstetrics (2017) Research and Reports in Gynecology and Obstetrics (Special Issue 3-2017)
The development of late FHR deceleration and analysis of controversy FHR with hypoxia index.
Kazuo Maeda*Department of Obstetrics and Gynecology, Emeritus, Tottori University Medical School, Yonago, Japan
- *Corresponding Author:
- Kazuo Maeda
3-125 Nadamachi
Yonago
Tottoriken
683-0835 Japan
Tel & Fax: 81-859-22-6856
E-mail: maedak@mocha.ocn.ne.jp
Accepted Date: July 14, 2017
Citation: Maeda K. The development of late FHR deceleration and analysis of controversy FHR with hypoxia index. Res Rep Gynaecol Obstet. 2017;1(3):1-3
Abstract
Controversy late deceleration of FHR of favorable neonatal outcome was analyzed by the developing mechanism of abnormal FHR changes and hypoxia index determined with the sum of deceleration duration and nadir heart rate.
Keywords
Fetus, Heart rate, Late deceleration, Controversy FHR, Bradycardia, Hypoxia
Introduction
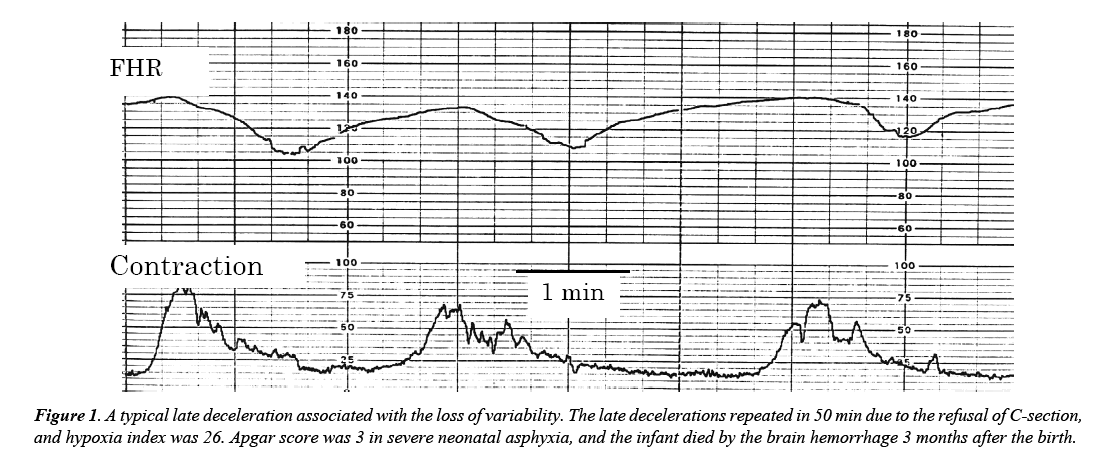
Transient FHR reduction (deceleration) was classified to U-shape variable one and V-shape periodic one, which is further divided into early deceleration (ED) and late deceleration (LD), of which lag time to uterine contraction is 20 or rmore seconds (Figure 1). LD is placental insufficiency and its outcome was ominous by Hon [1]. Caldeyro- Barcia Type I dip was ED and Type 2 was LD [2]. Controversy LD was neonatal favorable outcome after detection of fetal LD, despite it was told that LD associated ominous outcome [1].
Developing mechanism of FHR changes
Strong uterine contraction [2] and high intrauterine pressure decreases the inflow of maternal arterial blood into placenta, developing fetal hypoxia and FHR bradycardia.
Compression of large maternal blood vessels:
1. Supine hypotension: Inferior vena cava is compressed by pregnant uterus in supine posture reducing the blood return to heart developing maternal hypotension followed by fetal hypoxia.
2. Compression of pelvic large arteries with contracted pregnant uterus stops placental arterial blood supply in supine posture, developing fetal hypoxia and LD (Poseiro effect [3]).
The loss of FHR variability: Fetal outcome was ominous even in very mild LD by Hon, [1] however; mild LD was recognized in the loss of FHR variability, which was severe fetal brain damage. Early delivery is done before the loss of variability [4,5].
Lateral posture against large vessel compression
Maternal lateral posture rejects vessel compression, and the compression relaxes recovering the blood supply to the placenta. The treatment was confirmed by the LD disappearance immediately after maternal lateral posture [3]. However, staffs should further look for LD developing pathologic process, if the LD still remains after changing to lateral posture.
Tocolysis of uterine hypercontraction
It was effective to use orcinoprenaline in the past [4]. In cases of uterine hyper contraction. Modern rapid tocolysis will be terbutaliine drip infusion.
Early delivery
Severe LD case is cured by early caesarean delivery before the loss of variability preventing fetal brain damage, if intrauterine treatment was ineffective.
Actocardiogram
The neonate was vigorous when fetal acceleration duration ratio to fetal movement burst duration (A/B ratio) was more than 1 in spite of LD presence before birth, which was experienced by the author.
Hypoxia index (HI)
HI is (the sum of FHR deceleration duration (min) divided by the nadir fetal bradycrdia (bpm) × 100), which is numerical evaluation of deceleration length in hypoxia. Maeda intended to estimate fetal damage by FHR deceleration which was parallel to hypoxia, i.e., the HI was 25 and 26 in two cases of the loss of variability followed by cerebral palsy and infantile brain damage, while the HI was 24 or less in FHR changes with normal variability without fetal brain damage [5].
Hypoxia index in controversy LD
As the HI of 3 consecutive late decelerations was less than 10, while the HI of repeated LDs for 50 min was 26, controversy LD will develop in small number of LDs or in the rapid LD disappearance in maternal lateral posture, while repeated LDs for long periods are ominous, due to the summation of hypoxia in repeated bradycardia, which was closely correlated to low PaO2 in rabbit hypoxia [6]. Therefore, the case of highly increasing HI will receive intrauterine LD therapy, e.g. maternal lateral posture, terbutaline etc., or early caesarean delivery. As the numeric HI clearly indicates the threshold to fetal risk, HI will contribute to cure the fetus from fetal damage in LD.
In the future, hypoxia index must be automatically calculated using computer in fetal monitoring, alarming HI rise, where the sum of durations and the lowest FHR in the decelerations will calculate HI. Fortunately, the duration of deceleration and the nadir FHR are measured in the FHR score formation [7], incorporating in our automated FHR monitoring program [8]. All deceleration durations are summarized and the lowest heart rate is selected in the formation of FHR score calculating HI. As deceleration duration is measured by sec, it is divided by 60 to use it in HI. The FHR score and HI will be rapidly reported doctor, and displayed on screen.
Discussion
As PaO2 in the deceleration is parallel to bradycardia, the hypoxia of early small number of LD will theoretically mild and HI is lower than 10 in my case, hypoxia is too mild to damage fetus in small number of LD or quickly recovered LD after lateral posture will be hazardless, forming controversy LD. However, hypoxia, overlapped to frequently repeated LD, will be hazardous to the fetus, Fortunately, hypoxia index will express the grade of hypoxia in the damaged fetus in the loss of variability, i.e., the HI was 25 and 26, in the loss of variability, and 20-24 in the cases who were severe FHR change before the loss of variability, the threshold HI to damage fetus will be more than 24.
The hypoxic fetal brain damage will be clarified by the HI level. The HI=11 in a case of placental abruption, where bradycardia duration was 19 min, nadirFHR=90, bradycardia duration was 10 min. Normal neonate was achieved.
General concept of the time to C-delivery is less than 30 min after onset of acute bradycdia. HI is 30 min × 100/80 bpm=38, which is abnormal HI. HI is 26, if the time is 20 min. Therefore, less than 30 min is correct threshold of C-delivery in acute fetal bradycardia. HI was 26, in the case of repeated LD in 50 min and nadir FHR was 100 bpm, where the HI was abnormal. Thus, Apgar was 3, and died 3 months by brain hemorrhage. As no brain damage HI I will be 24 or less, repeated deceleration count should be 15 times, if nadir heart rate is 90 and LD duration is 1.5 min. Normal HI would be 24 or less, from these case reports.
Conclusion
Controversy normal outcome of late deceleration cases occurs in small number of late decelerations. Sudden disappearance of LD after lateral posture may be another controversy outcome of late deceleration. Fetal damage develops in cases of repeated decelerations in long periods due to the summation of hypoxia in repeated decelerations. The hypoxia index is a useful objective parameter to predict and prevent hypoxic fetal damage in cases of repeated decelerations and fetal acute bradycardia. FHR score and hypoxia index are very useful new tools in computerized objective fetal diagnosis.
References
- Hon EH. An atlas of fetal heart rate patterns (8th edn). Harty Press, New Haven, 1968.
- Caldeyro-Barcia R, Poseiro JJ, Mendez-Bauer C, et al. Effects of abnormal uterine contractions on fetal heart rate in labor. Proc ObGy Cong. 1967;9-27.
- Poseiro JJ, Mendez-Bauer C, Caldeyro-Barcia R, et al. Effect of uterine contractions on maternal blood flow through the placenta. Perinatal factors affecting human development, Paho Advisary Committee. 1969;161-71.
- Caldeyro-Barcia R, Magana JM, Poseiro JJ, et al. New approach to the treatment of acute intrapartum fetal distress. Perinatal factors affecting human development, Paho Advisary Committee. 1969;248-53.
- Maeda K. Modalities of fetal evaluation to detect fetal compromise prior to the development of significant neurological damage. JOGR. 2014;40:2089-94.
- Umezawa J. Studies on the relation between heart rate and PaO2 in hypoxic rabbit: A comparative study for fetal heart rate change during labor. Acta Obstet Gynecl Jpn. 1976;28:1203-12.
- Maeda K, Kimura S, Nakano H, et al. Pathophysiology of fetus. Fukuoka Printing, Fukuoka. 1969.
- Maeda K, Noguchi Y, Nagasawa T, et al. Quantitative fetal heart rate evaluation without pattern classification. In: Kurjak, Chervenak (ed.). Textbook of Perinatal Medicine (2nd edn). Informa, UK. 2006;1487-95.