- Biomedical Research (2013) Volume 24, Issue 1
Surgical treatment of hydrosalpinx improves the expressions of estrogen receptor and progesterone receptor in the endometrium in implantation window.
Yiping Zhong1#, Jin Li2#, Haitao Wu1, Ying Ying1, Yafeng Liu1, Canquan Zhou1*, Yanwen Xu1,Xiaoting Shen1, Quan Qi11Reproductive Medicine Center, The First Affiliated Hospital, Sun Yat-Sun University, Key Laboratory of Reproductive Medicine of Guangdong Province, Guangzhou 510080, China.
2Guangdong No.2 Provincial People’s Hospital, Guangzhou 510000, China.
- *Corresponding Author:
- Canquan Zhou
Reproductive Medicine Center
The First Affiliated Hospital of Sun Yat-sen University
Guangzhou 510080
China
Email: zhoucanquan@hotmail.com
Accepted date: December 13 2012
Abstract
To investigate the effect of surgical treatment of hydrosalpinx on the expressions of estrogen receptor (ER) and progesterone receptor (PR) in the endometrium in implantation window, a total of 60 patients with hydrosalpinx and 30 patients with fallopian tube obstruction were recruited. In the implantation window, immnohistochemistry was carried out to detect the expressions of ER and PR in the endometrium of the hydrosalpinx patients before and after surgery and of patients with fallopian tube obstruction. In the implantation window, the expressions of ER and PR in the endometrium of hydrosalpinx patients before surgery were significantly lower than those in patients with fallopian tube obstruction (P<0.05). However, there were no significant differences in the expressions of ER and PR in the implantation window between hydrosalpinx patients after surgical intervention and fallopian tube obstruction patients (P>0.05). Furthermore, for patients with hydrosalpinx, the expressions of ER and PR in the implantation window were dramatically increased after surgery (P<0.05). Hydrosalpinx reduces the expressions of ER and PR in the endometrium in the implantation window, which can be improved by surgical intervention.
Keywords
Hydrosalpinx, estrogen receptor; progesterone receptor, endometrium in implantation window
Introduction
Under the influence of steroid from the ovaries, the endometrium undergoes periodical changes. Embryos can implant in the endometrium only in proper phase [1]. The blastocyst implantation is shared by all mammals in nature and usually occurs between 3 days and 6 days after fertilization, which is corresponding to the days 21~24 or 5~8 days after the LH peak. The embryos enter the uterus in the implantation window. The embryos and endometrium secret some related proteins and cytokines in a strictly spatial-temporal sequence. These proteins and cytokines recognize each other and cooperate leading to the implantation [2]. The endometrial receptivity refers to the maximal acceptance of the implantation of embryos by the endometrium in the implantation window. The implantation is characterized by a series of cellular and molecular events occurring in sequence, which are regulated by some cytokines and/or proteins and mediate the interaction between cells and cells as well as between cells and matrix. These bioactive cytokines and proteins can be used to evaluate the acceptance of embryo implantation by endometrium and thus become markers of the endometrial receptivity. The endometrial receptivity is regulated by the steroids (estrogen and progesterone) secreted by ovaries. The binding of steroids to the corresponding receptors then initiates the synthesis of down-stream molecules.
Tubal factors are the main causes of female infertility and account for about 40% of all causes. Furthermore, the hydrosalpinx accounts for 10~30% of the tubal factors causing infertility. In vitro fertilization-embryo transfer (IVF-ET) was initially applied in women with tubal factor infertility. However, numerous studies show the hydrosalpinx can reduce the implantation rate and pregnancy rate [3]. The mechanisms underlying the impact of hydrosalpinx on the IVF-ET are poorly understood. There is evidence that the influence of hydrosalpinx on the endometrial receptivity is one of the mechanisms [4]. In the present study, the expressions of estrogen receptor (ER) and progesterone receptor (PR) in the endometrium in the implantation window were compared between hydrosalpinx patients and those with fallopian tube obstruction and the expressions of ER and PR in the endometrium in the implantation window in hydrosalpinx patients were also compared before and after surgery. Our results may be helpful to elucidate the cause of poor outcome of hydrosalpinx patients following IVF-ET.
Materials and Methods
Patients
A total of 60 patients with hydrosalpinx and 30 patients with fallopian tube obstruction were recruited from April 2010 to December 2010 from the Center of Reproductive Medicine of the Affiliated First Hospital of Sun Yat-sen University.
All patients were aged < 40 years and had regular menstrual cycle. Endocrine examinations revealed normal and the basal body temperature was biphasic. Hormones were not administered within 6 months before study. Endometriosis, uterine fibroids, polycystic ovary syndrome, ovarian cancer, infertility of unknown causes, immune infertility, chronic systemic disease, sexually transmitted disease, trophoblastic disease, smoking and drinking as well as male infertility were excluded before study.
Diagnosis
Hydrosalpinx: The bilateral or unilateral hydrosalpinx was diagnosed by hysterosalpingography (HSG) or laparoscopy (LAP) and untrasonography.
Fallopian tube obstruction: The fallopian tube obstruction was diagnosed by HSG or LAP, and ultrasonography was performed to exclude the presence of hydrosalpinx.
Surgical intervention of hydrosalpinx
Vaginal ultrasound-guided hydrosalpinx aspiration, laparoscopic salpingostomy, laparoscopic proximal tubal ligation or laparoscopic salpingectomy was performed.
Sample collection and processing
The LH peak was measured by using LH strip since the 10th day of menstrual cycle. In addition, transvaginal ultrasonography and test of serum sex hormones were also performed. At days 7~8 after ovulation, the endometrium was collected at the bottom of uterus by using a curette and washed in normal saline to remove the blood. Samples were fixed in fixation solution, embedded in paraffin and sectioned. Pathological examination was carried out to confirm that the endometrium was in the secretory phase. For patients with hydrosalpinx, the endometrium was collected in the implantation window before and after surgery, but collection of endometrium was done once in patients with fallopian tube obstruction.
Immunohistochemistry
Mouse anti-human ER monoclonal antibody (DAKO) (1:50) and mouse anti-human PR monoclonal antibody (DAKO) (1:50) were used for immunohistochemistry which was performed according to the manufacturer’s instructions.
Determination of findings
Five fields were randomly selected from each section at a magnification of 4000, and the proportion of positive cells was calculated.
Statistical analysis
Data were expressed as mean ± standard deviation (x±s). Statistical analysis was performed with SPSS version 13.0. A value of two-tailed P < 0.05 was considered statistically significant.
Results
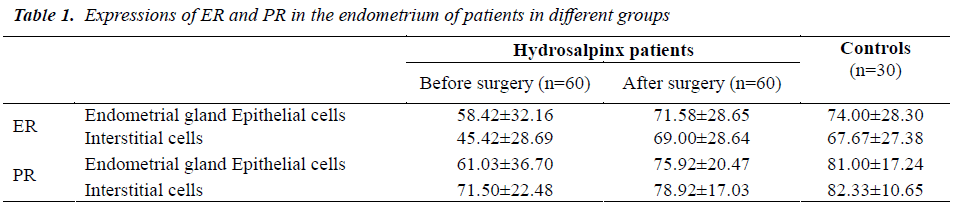
Under light microscope, the expressions of ER and PR were noted in the endometrial gland epithelial cells and interstitium. There were significant differences in the expressions of ER and PR in hydrosalpinx patients between before and after surgery (P< 0.05). Marked differences n the expressions of ER and PR were also noted between hydrosalpinx patients and control patients before surgery (P< 0.05). However, the expressions of ER and PR in the endometrium were comparable between two groups (P>0.05) (Table 1).
Discussion
The dysfunction of any organ in the female reproductive system or the abnormalities in the central nervous system controlling the ovarian function may inevitably lead to the changes in the endometrium resulting in infertility. Therefore, the histological examination of endometrium is a reliable method to understand the functions of estrogen and progesterone and the ovulation. In addition, this method is also helpful to identify the organic disease in the endometrium. Studies reveal the dysplasia of endometrium can cause the absence of ER and PR in the endometrium and under this condition the endometrium is non-responsive to steroids of ovary [5]. In 1966, a protein was identified in the cytoplasm by the sucrose density gradient ultra-centrifugation and its sedimentation coefficient was 19.84×104 U. This protein was later called ER. Afterwards, researchers also find the PR.
Molecular structures of ER and PR
The ER gene locates in the chromosome 6, and its mRNA is 6322 bp in length and encodes 595 amino acids. ER is a glycoprotein with the molecular weight of 66 KD. ER is highly specific and has a high affinity to estrogen but has low binding capacity. The ER is biologically unstable and susceptible to damage by heat, but the ER-estradiol complex is relatively stable. ER is a nuclear receptor of steroid hormone family and widely expressed in the central nervous system, cardiovascular system, genitourinary system, bone, kidney, lung and uterine [6].
PR gene locates in chromosome 11, and its cDNA is 3014 bp in length and encodes 933 amino acids. PR is a protein with the molecular weight of 20~110 kD. PR is highly specific and has high affinity to progesterone. The synthesis of PR is regulated by estrogen. The binding of ER to estrogen may lead to the expression of PR.
Types of ER and PR
There are two different forms of the estrogen receptor, usually referred to as α and β [7]. ER gene has 8 extrons and the encoded protein has 6 domains (A-F). The A/B domain in the N-terminal is mainly the AF-1 functional domain which is highly variable, can bind to the antibody against ER and involves in the transcriptional activation of target genes. The C domain is a DNA binding domain (DBD) and is a conservative cysteine-rich domain in the nuclear receptor family. This domain mediates the binding of receptor to DNA. In addition, the D domain can bind to the heat shock proteins and can generate nuclear localization signals and stabilize the DNA binding. The E/F domain in the C terminal consists of hormone binding domain or ligand binding domain (LBD) (E domain) and functional AF-2 domain (F domain). ERα and ERβ are encoded by 8 extrons individually but both genes locate in different chromosomes. ERα gene locates in 6q25.1, consists of 140 kb base, encodes 595 amino acids and has the molecular weight of 66 kD. ERβ gene locates in 14q22-24, consists of 40 kb base, encodes 530 amino acids and has the molecular weight of 59.2 kD.
PR has two different functional isoforms: PR-A and PR-B [8], which are encoded by the same gene in the 11q-13. However, this gene is regulated by two different promoters: promoters A and B and thus transcribed into two mRNAs with different bases which encode 796 amino acids and 933 amino acids, respectively. The relative molecular weight of PR-A is 90 ku and that of PR-B is 120 ku. The unique difference between PR-A and PR-B is additional 164 amino acids in the N terminal of PR-B which have two specific transactivation domains: AF1 and AF2 mediating the regulation of progesterone [9]. Under the majority of conditions, the PR-A has potent activity which is absent in PR-B. We speculate that the PR-A might non-competitively bind to the transcriptional factors specific to PR and ER.
Biological features of ER and PR
In the absence of estrogen, ER is related to the heat shock protein. When the ER binds to the estrogen, ER is separated from heat shock protein followed by the phosphorylation of serine and threonine. Then, the ER binds to another ER forming homodimers which can activate the EER complex and promotes the binding of this complex to the specific DNA (estrogen response element (ERE) in the promoter of the target genes) resulting in the activation of transcription of proliferation and differentiation related genes. The distribution of ERα and ERβ is different in tissues, which determines the different physiological functions of ERα and ERβ. ERα is predominantly expressed in the prostate, bladder, lung, ovary, central nervous system, colon, stomach, heart and blood vessels. In special tissues, different receptors are distributed in different types of cells. For example, ovary has the expressions of both ERα and ERβ. There is evidence showing that ERβ expression is confined to the granular cells and ERα to the theca cells. These findings also demonstrate ERα and ERβ possess different functions in the ovary. Zvonic et al and Kimber showed the ERβ expression in the normal human breast was higher than the ERα expression [10,11]. John et al found that the ERβ expression remained unchanged in ERα knockout animals. Although the ERα and ERβ have 55% homology, the distribution of ERα and ERβ is different resulting in the selectivity of their functions [12].
Arnett-Mansfield et al speculated that the PR of two isoforms was evenly distributed in the nucleus of the normal endometrium in the proliferative phase. In the secretory phase, the distribution of PR in the nucleus is significantly increased, especially the PR-B. The changes in the hormones may alter the distribution of PR isoforms in the nucleus [13]. Mote et al postulated that the PR-A was predominantly expressed in the interstitium of endometrium in the whole menstrual cycle [14]. The estrogen can alter the expression levels of PR-A and PR-B and induce the mRNA and protein expressions of PR in the majority of target cells [15].
Changes in the ER and PR
The expressions of ER and PR are influenced by the in vivo hormone levels. In different phases of menstrual cycle, the expressions of ER and PR are also different. The endometrium is affected by the estrogen resulting in the alteration between proliferative phase and secretory phase. The expressions of ER and PR are first maintained in a specific level in the influence of estrogen, then peak with the increase of estrogen level (days 14~15 of menstrual cycle). Following subsequent decrease of ER and PR expressions, the expressions of both protein increase again with the elevation of estrogen level, but this increase is lower than that before which may be attributed the suppressive effect of high progesterone level on the synthesis and function of ER and PR. Therefore, the changes in the expressions of ER and PR in the menstrual cycle are closely associated with the in vivo estrogen and progesterone and usually periodic.
Effect of hydrosalpinx on the expressions of ER and PR in the endometrium
Our results showed the expressions of ER and PR in the endometrial gland epithelial cells and the endometrial interstitium of hydrosalpinx patients before and after surgery and in fallopian tube obstruction patients. In the hydrosalpinx patients, the expressions of ER and PR in the endometrium in the implantation window before surgery were lower than in the controls. After surgery, the expressions of ER and PR were comparable between two groups. In addition, the expressions of ER and PR were also different in hydrosalpinx patients between before and after surgery. These findings suggest hydrosalpinx influences the expressions of ER and PR in the endometrium in the implantation window, which increased after surgical intervention.
According to the findings in previous studies on chronic inflammation, in the hydrosalpinx patients, the contents of toxic substances including cytokines in the lesions are very high (16). These toxic substances can enter the uterus. Following the local infiltration of inflammatory cells and production of inflammatory cytokines, the sensitivity of endometrium to hormones from ovary is reduced and the expressions of ER and PR are also decreased. After surgical intervention for hydrosalpinx, the inflammation is improved and the expressions of ER and PR are also increased when compared with those before surgery but not different from those in the controls.
Before the endometrial receptivity is established and after the endometrial receptivity disappears, the expressions of ER and PR in the endometrium have a decreasing tendency which is dependent on the P. The failure of P regulation may significantly affect the endometrial receptivity [17]. At the site of uterus where the embryos implant in, a series of cytokines are expressed and form a network, which can regulate the expressions of some factors mediating the endometrial receptivity. Thus, the endometrium can achieve the receptivity at the designed time. A lot of studies report that hydrosalpinx can decrease the expressions of endometrial receptivity related markers, which affects the molecular network at the site where the embryos implant in and impacts the balance of endometrial receptivity and the regulation of estrogen and progesterone in the endometrium. However, the specific mechanisms are required to be further elucidated.
The fluctuation of in vivo hormones and the changes in the endometrium in the menstrual cycle are large, thus more multicenter, prospective, randomized studies with large sample size are needed to clarify the effect of hydrosalpinx on the expressions of ER and PR in the endometrium.
Acknowledgment
This study was funded by Guangdong Science and Technology Program (No. 2009B030801155) and Guangdong Population and Family Planning Project (No. 2010243).
References
- Lessey BA. Endometrial integrins and the establishment of uterine receptivity. Hum Reprod 1998; 13: 247-258.
- Taylor E, Gomel V. The uterus and fertility. Fertil Steril 2008; 89: 1-16.
- Mijatovic V, Veersema S, Emanuel MH, Schats R,Hompes PG. Essure hysteroscopic tubal occlusion device for the treatment of hydrosalpinx prior to in vitro fertilization-embryo transfer in patients with a contraindication for laparoscopy. Fertil Steril 2010; 93: 1338-1342.
- Seli E, Kayisli UA, Cakmak H, Bukulmez O,Bildirici I, Guzeloglu-Kayisli O, Arici A. Removal of hydrosalpinges increases endometrial leukaemia inhibitory factor (LIF) expression at the time of the implantation window. Hum Reprod 2005; 20: 3012- 3017.
- Levy C, Robel P, Gautray JP, De Brux J, Verma U, Descomps B, Baulieu EE. Estradiol and progesterone receptors in human endometrium, normal and abnormal menstrual cycle and early pregnancy. Am J Obstet Gynecol 1980; 136:646-51.
- Enmark E, Pelto-Huikko M, Grandien K, Lagercrantz S, Lagercrantz J, Fried G, Nordenskjöld M, Gustafsson JA. Human estrogen receptor β-gene structure, chromosomal, localization, and expression pattern. J Clin Endocrinol Metab 1997; 82: 4258-4265.
- Hyder SM, Chiappetta C, Standel GM. Interaction of human estrogen receptor α and β with the same naturally occurring estrogen response element. J Biochem Pharmacol 1999; 57: 597-601.
- Graham JD, Clarke CL. Expression and transcriptional activity of progesterone receptor A and proges terone receptor B in mammalian cells. Breast Cancer Res 2002; 4: 187-190.
- Kastner P, Krust A, Turcotte B, Stropp U, Tora L, Gronemeyer H, Chambon P. Two distinct trogenregulated promoters generate transcripts encoding the two functionally different human progesterone receptor forms A and B. Embo J 1999; 9: 1603-1614.
- Zvonic S, Baugh JE Jr, Arbour-Reily P, Mynatt RL, Stephens JM. Cross-talk among gp130 Cytokines in adipocytes. J Biol Chem 2005; 280:33856-33863.
- Kimber SJ. Leukemia inhibitory factor in implantation and uterine biology. Reproduction 2005;130:131-145.
- Couse JF, Lindzey J, Grandien K, Gustafsson JA, Korach KS. Tissue distribution and quantitative analysis of estrogen receptorαand estrogen receptorβmessenger ribonucleic and in the wide-type and ERαknockout mouse. Endoceinology 1997; 138: 4613-4621.
- Arnett-Mansfield RL, DeFazio A, Mote PA, Clarke CL. Subnuclear Distribution of Progesterone Receptors A and B in Normal and Malignant Endometrium. J Clin Endocrinol Metab 2004; 89: 1429-1442.
- Mote PA, Balleine RL, McGowan EM, Clarke CL. Colocalisation of progesterone receptors A and B by dual immunofluorescent histochemistry in human endometrium during the menstrual cycle. J Clin Endocrinol Metab 1999; 84: 2963-2971.
- Tseng L, Zhu HH. Regulation of progesterone receptor messenger ribonoucleic acid by progestin in human endometrial stromal cells. Biol Reprod 2000; 57: 1360-1366.
- Strandell A, Thorburn J, Wallin A. The presence of cytokines and growth factors in hydrosalpingeal fluid. J Assist Reprod Genet 2004; 21:241-247.
- Petersen A, Bentin-Ley U, Ravn V, Qvortrup K, Sørensen S, Islin H, Sjögren A, Mosselmann S, amberger L. The antiprogesterone Org31710 inhibits human blastocyst- endometrial Interactions in vitro. Fertil Steril 2005; 83:1255- 1263.