Original Article - Annals of Cardiovascular and Thoracic Surgery (2018) Volume 1, Issue 3
Surgery of extensive defects of the anterior wall of the trachea and soft tissues of the neck after laryngo-tracheostomy
Eshonhodjaev Otabek Djuraevich, Khudaybergenov Shukhrat Nurmatovich, Hayaliev Rustem Yakubovich*, Tuhtaev Denis, Mirsidikov Mirabbos and Egamov Faruh
Tashkent Medical Academy, Tashkent, Uzbekistan
- *Corresponding Author:
- Hayaliev Rustem Yakubovich
Thoracic Surgeon
Candidate of Medical Sciences
Associate Professor
Tashkent Medical Academy
Tashkent, Uzbekistan
Tel: +998909178716
E-mail: rustemmed@rambler.ru
Accepted date: October 03, 2018
Citation: Eshonhodjaev O, Khudaybergenov S, Hayaliev R, et al. Surgery of extensive defects of the anterior wall of the trachea and soft tissues of the neck after laryngo-tracheostomy. Ann Cardiovasc Thorac Surg. 2018;1(3):63-70.
DOI: 10.35841/cardiovascular-surgery.1.3.63-70
Visit for more related articles at Annals of Cardiovascular and Thoracic SurgeryAbstract
The authors present the results of treatment of 103 patients with extensive defects of the trachea and soft tissues of the neck after laringo-tracheostomy or tracheostomy. The article shows a differentiated approach to the plastic of the anterior wall of the trachea depending on the size of the defect. The efficiency of two-stage reconstructive plastic surgery with the installation of T-stent in the stenosis zone with exposure of 6 months to 8 months is proved. Microsurgical aid was needed for patients who had previously undergone multiple interventions on the trachea in other hospitals.
Keywords
Trachea, Extensive defects, Tracheostomy, T-shaped stent, Skin-muscle plasty, Auto-rib cartilage, Reconstructive operations, Delta-pectoral flaps
Introduction
In modern conditions, the treatment of patients with Extensive Defects of the Trachea (EDT) should be performed in specialized departments of thoracic surgery. At the same time, many issues of early diagnosis, treatment, prevention of postoperative complications and postoperative rehabilitation of this category of patients are still far from being resolved.
First of all, it concerns the detection of this group of patients in the early stages of the disease with mass preventive examinations and the primary treatment of patients in the clinic, the volume of their examination and treatment in a specialized surgical department. The optimal sequence of conservative therapy and surgical treatment has not been developed.
In order to restore the airway patency in critical and decompensated stenosis of the larynx and trachea in some patients, tracheostomy with the introduction of cannula in the tracheal lumen below the level of stenosis is used. In some cases, the surgical correction of stenosis is performed wide laryngotracheostomy with excision of tissues around the stenotic zone, followed by the introduction in the lumen of the respiratory tract of tubular dilators for a long time. After forming a stable laryngotracheotomy there is the question of the closure of the defects without violating the patency of trachea and restenosis. Often post-traumatic stenoses, complicated by suppuration in the area of neck injury, are combined with defects of the tracheal wall [1,2]. A large number of possible tissues and materials, as well as options for operations aimed at eliminating defects in this area are proposed [3-6]. The main requirements are formed clearly: they must be of sufficient size, provide a frame function and the possibility of evacuation of the secret, as well as be resistant to infection [7,8].
Tatur AA, et al. [9] give indications and contraindications for use, technique of various methods of local plasty of tracheal defects. In their material the local tracheoplasty taking into account the size of defects, the safety of the side walls, the severity of the tracheomalacia was performed in 26 of patients with cicatricial stenosis. The use of local plasty with the use of musculocutaneous and muscle with autorib flaps allowed to obtain good and satisfactory results in 95% of patients. Stageby- Stage Tracheal Reconstruction (SSTR) is used in 26%-55% of patients with cicatricial tracheal stenosis [10,11]. With SSTR, it is impossible to radically eliminate the pathological substrate in the tracheal wall, and its lumen should be formed for a long time on a silicone T-shaped stent-protector. They are low-traumatic, easily tolerated by patients, simplify, in contrast to the endoprosthesis, control of endotracheal processes and allow today to rehabilitate 85%-90% of patients who can not undergo a radical operation because of the high risk of complications [12-16]. The main disadvantages of SSTR are the duration of treatment and the need for plastic closure of the tracheal defect [12,13,15,17,18]. In the process of SSTR, limited and extensive defects of the anterior, posterior and lateral walls of the trachea are formed.
Defects of the trachea in the treatment of cicatrical stenosis of trachea can communicate with the lumen of the esophagus with formation of tracheoesophageal fistula or brachiocephalic trunk with forming tracheoinnominate fistula. The formation of internal tracheal fistulas is rare and requires special surgical tactics [7,9,12]. EDT complicate the course of cervical injuries and purulent-destructive processes, combined treatment of tumors of the larynx and thyroid gland, but can occur in SSRT, and as a result of the lack of seams of intertracheal anastomosis after Circular Tracheal Resection (CTR) [1,10,12,14]. To close the limited DT different options of local skin-muscle plastics are used. In case of a defect of the anterior wall of the trachea with a length of more than 3 cm to 4 cm, in the absence or deficiency of its lateral walls, plastic is used with auto-and allogeneic cartilage or bone tissue, pre-fabricated free, on the vascular leg and displaced revascularized flaps. Implantation of various artificial materials, as well as tracheal prostheses, does not lead to epithelialization of the surface and, as a rule, ends with the development of hypergranulations, infection and rejection [14,15,17]. In contrast to the use of autologous bone (sternum, hyoid, radiation) use of autocartilage is considered the "gold standard" in plastic surgery of head and neck, including the trachea. Depending on the volume of tracheoplasty, specialization and traditions of the clinic advantage has autocartilage from the ear, the nasal septum or costal, which, unlike homokonservants, better take root, less likely to undergo resorption and reliably recreate the tracheal frame [3,5,7,10,11,17].
The problem of plastic closure of EDT can be solved by creating a combined flap, which should have a sufficient size, epidermal or epithelial lining, to ensure the framework of the lumen and be resistant to infection. Stiffening of the tracheal frame is necessary to prevent flotation of its walls during breathing and coughing. The use of the cheek or nose mucosa in complex flaps is problematic due to its frequent displacement into the tracheal lumen, scarring and rejection of the entire "sandwich flap" [9,12,17]. The use of various combined flaps with their microsurgical revascularization on the neck for plastic surgery is promoted by some authors and reasonably criticized by others, due to the high complexity and traumatic nature of the technique. Probably, this plastic should be used in patients where simple methods cannot reliably recover the tracheal lumen [2,4,7,8]. Despite the many proposed methods, the problem of closure of extensive laryngotracheal defects is relevant and continues to be the subject of research and discussion of microsurgeons, otolaryngologists and thoracic surgeons [3,8,11,14,15].
Materials and Methods
In the department of surgery of lungs and mediastinum RSCPMCS named after acad. V. Vakhidov in the period from 2008 to 2018 there were 103 patients with EDT in subglottic division of the larynx and soft tissues of the neck after laryngo-tracheostomy or tracheostomy. Among them, 33 patients were sent from other medical institutions of the Republic, 70 patients were hospitalized for the final stage of the combined stage treatment of scar posttraheostomy and postintubation tracheal stenosis. Previously in our department, these patients underwent the stages of endoscopic coagulation, bougienage of tracheal stenosis with the subsequent plasty of the trachea with the formation of the lumen by the T-shaped stent. After the planned examination, including endoscopy, chest MSCT with cervical region capture and general clinical methods of diagnosis, the patients underwent surgical treatment.
In patients with persistent extensive defects of the anterior wall of the trachea and soft tissues of the neck, with a defect size not exceeding 2 cm in width and up to 4 cm in length, a three-layer skin-muscle plastic was carried out with a one-time elimination of the defect by local tissues.
11 patients had extensive defects of the anterior-lateral walls of the cervical trachea and subglottic division of the larynx, as well as a deficit in the soft tissues of the neck around the stoma. In addition, the presence of large defect after laryngotracheostomy was complicated by the violation of the vertical axis of the lumen of the respiratory tract, in this case, the back wall of the trachea protruded forward in the area of the defect. The complexity of the plastics was the absence of soft tissues around the defect, absence of cartilage and skin-muscle frame and the bend of the vertical axis of the trachea in the anterior-posterior direction, which required the creation of a transplant on a rigid frame, of sufficient size, with a mucous lining inside with the possibility of creating a sealed lumen.
Results and Discussion
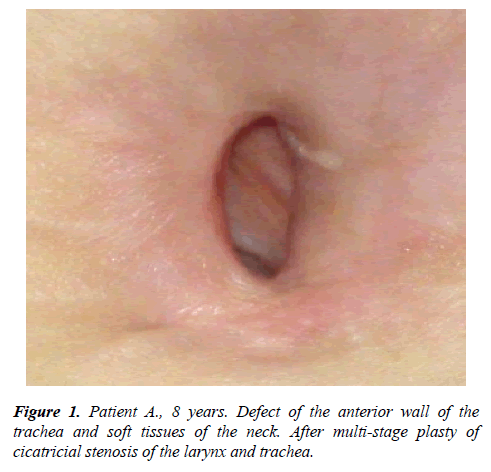
Local three-layer or four-layer skin-muscle plastic operations were performed in patients (n=92) with posttraheostomy defects of the anterior wall of the trachea and soft tissues with defect sizes from 1.0 cm to 2.0 cm wide and from 2.0 cm to 4.0 cm long (Figure 1), with a defect depth of more than 8 mm, i.e. anterior-posterior size of the tracheal lumen and a stable formed lumen of the respiratory tract in the zone of plastics without the presence of a protector (T-shaped stent or tracheostomy cannula).
The essence of the technique is to perform the cut, bordering the defect with scarred skin retreating from the edges of 0.7 cm to 0.9 cm and a depth of an average of 0.8 cm to 1.0 cm, depending on the size of the defect to be eliminated. At the same time, on the one hand, the cutting out skin flaps, i.e. their mobilization should be as sufficient as necessary to prevent tension of the created first layer. On the other hand excessive mobilization of the cut scraps can lead to flotation of the sewn edges that is fraught with the lack of frame-based structures of the respiratory tract in this zone after the plastic while breathing, phonation and coughing.
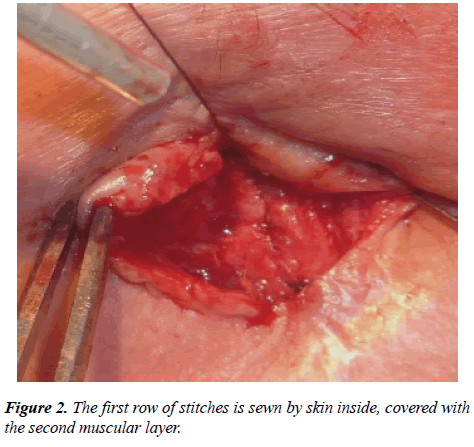
The created first layer, sutured with an atraumatic resorbable thread (Vicryl 3/0), is drawn inside by the epidermis. At the same time, it is mandatory to conduct submucosal sutures, which excludes further adhesion of bronchial secretion to the thread due to the absence of suture material in the tracheal lumen (Figure 2).
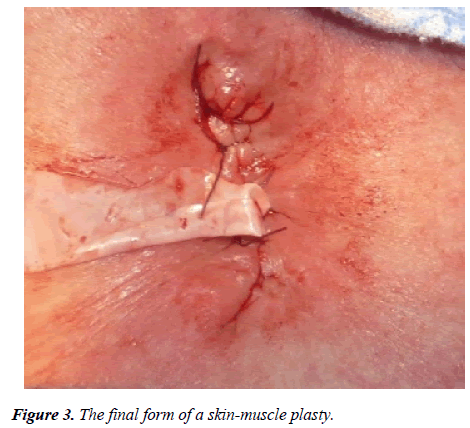
The second layer sutured adjacent muscles (m. sternocleidomastoideus, m. sternothyroideus, m. sternohyoideus) by capturing in the seam and the converge over the first layer. Third layer-skin, nodular atraumatic threads pull together and eliminate formed skin defect with leaving rubber drainage (Figure 3).
When applying each subsequent seam, the wall of the lower one was captured in the seamin order to further strengthen the wall, to exclude flotation of the layers in case of cough, and to avoid the formation of cavities between the layers.
After plasty of the defect we performed intraoperative bronchoscopy through the endotracheal tube by pulling it in subglottic division of the larynx for visual inspection of the sutured defect. At the same time, the tightness of the created front wall in the form of a skin insert, the mapping of layers, the presence or absence of deformation and/or contraction of the trachea in the plastic zone were investigated.
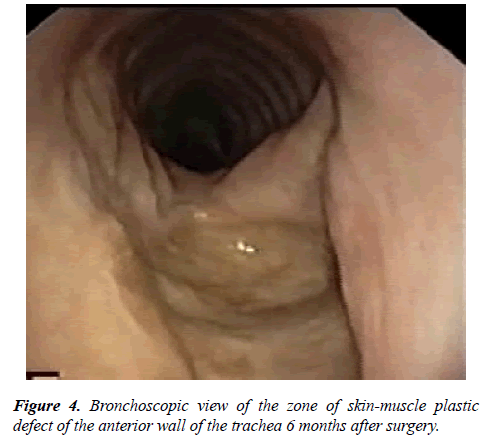
Control bronchoscopic examinations were performed on the 5th day after the operation. Then 1 month, 3 months, 6 months and a year after the operation (Figure 4). In 4 patients, there was a point insufficiency of sutures of skin-muscle plastics with the formation of skin-tracheal fistula 2 mm to 3 mm in size, which were closed independently without surgery by conservative therapy with the imposition of aseptic ointment bandages.
Eleven patients with extensive defects of the anterior-lateral walls of the trachea and distal larynx underwent complex reconstructive operations using microsurgical techniques.
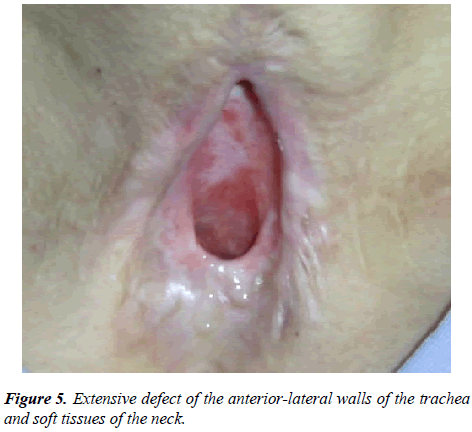
In 1 case, the patient was operated with the diagnosis: extensive defect of soft tissues of the neck and anterior-lateral walls of the cervical trachea and distal larynx. Posttracheostomic and postoperative cicatricial stenosis of the trachea. State after circular resection of the trachea. Scarparalytic stenosis of the larynx. Complete extended scar obliteration of the distal larynx and cervical trachea. State after laser recanalization of tracheal stenosis. Condition after laryngotracheoplasty on T-shaped stent (Figure 5).
In connection with the presence of extensive defect of the anterior wall of the trachea and soft tissues of the anterior surface of the neck microsurgical plastic with prefabricating deltopectoral auto-rib flap and autodermoplasty was performed. Defect size was 3 × 5 cm, depth was 1.2 cm. Axis of the airway was broken, with the distal division of the larynx and upper third of the trachea in the projection of the defect had the direction of the axis from behind forward in the sagittal direction, and the middle third of the trachea in a retrosternal region had the direction of the axis from front to back in the sagittal direction.
Plastics of EDT involves the restoration of not only soft tissue defect, but also the restoration of the mucous lining and tracheal skeleton function. To restore the defects of the trachea, a sufficient supply of full-fledged, hairless skin in the reconstruction zone is necessary. The absence of such areas in the neighborhood (sharp dystrophic or scar changes) requires the use of tissues with skin taken from other areas of the patient's body (the formation of the Filat stem, the movement of skin-fascial flaps on the vascular leg, autotransplantation of complex flaps on microvascular anastomoses).
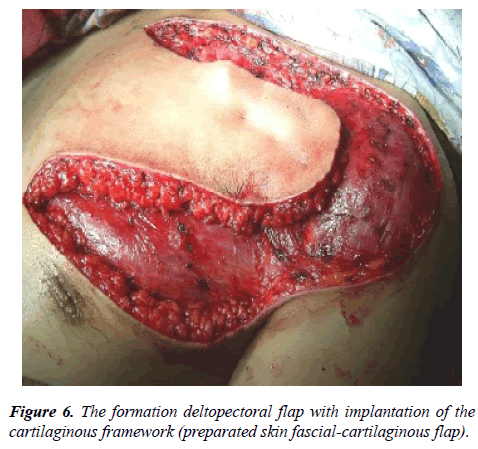
We have improved the method of forming a prefab flap. As a reference tissue in this case had used autorib cartilaginous skeletonimplanted in the flap. Depending on the parameters of the tracheal defect, a part of the cartilage was taken in the region of the connection of the VI and VII ribs, according to the conventional method in plastic surgery. Subsequently formed cartilage framework implanted subfacial in the distal portion of the delto-pektoral flap.
Stages of operation
Stage 1: The formation prefabricating deltopectoral flap with implantation of auto-rib cartilaginous skeleton in the distal part of the flap (Figure 6).
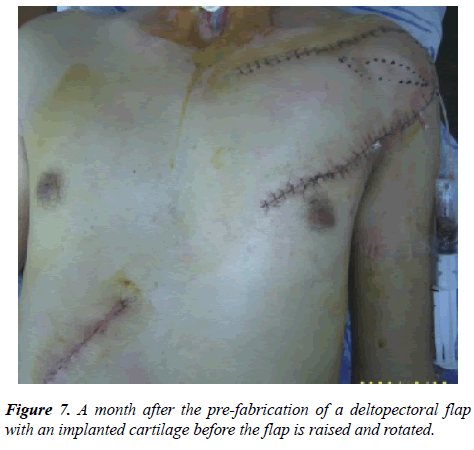
Stage 2: Raising pre-fabricated flap with the formation of a round stem. The substitution of the defect of the trachea with the restoration of the mucosal lining (leather flap) and cartilage skeleton (due to implanted auto-rib cartilage). Closure of the donor zone and the fascial part of the flap with split skin (Figure 7).
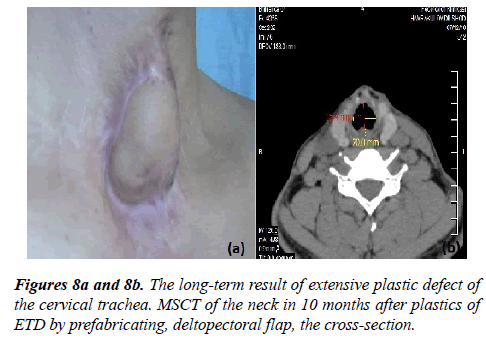
Stage 3: Cutting off the flap leg and the final plastic of the tracheal defect (Figure 8a). As a result of the reconstruction, the phonation and patency of the trachea were restored (Figure 8b).
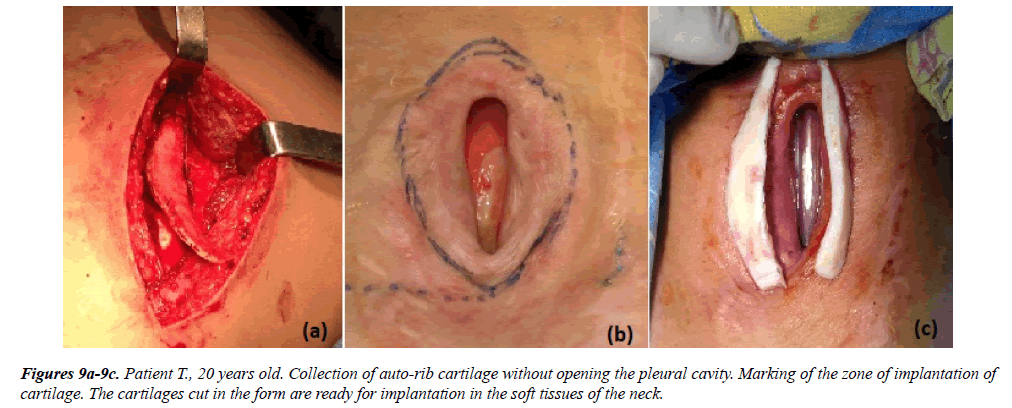
In 6 cases the patients underwent plastic operations of extensive defects by prefabricated auto-rib cartilage. The essence of the technique is a two-stage closure of the extensive defect of the trachea of the anterior-lateral walls of the trachea. At the same time, at the first stage, the preparing of auto-rib cartilage was performed without opening the pleural cavity (Figure 9a).
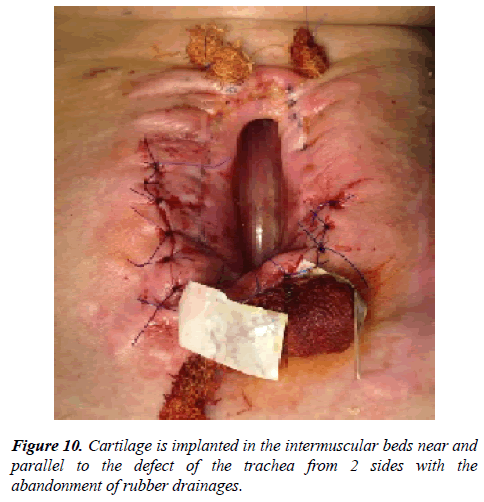
Then, two implants of the same shape were made from autocartilage in dimensions longer then the length of the defect on 1.5 cm (Figures 9b and 9c). Two incisions were made parallel to the vertical axis of the defect, cartilage implants were placed in the formed intermuscular bed. Soft tissue over the implants was stitching with biodegradable thread. Skin incisions were sutured with leaving rubber drainages with the imposition of aseptic betadine bandage (Figure 10).
The second stage was performed after 40 days, in order to engraftment of implants (auto-rib cartilages) with the possibility of forming encasement around them. Viability assessment of auto-rib cartilage was carried out by palpation. Thus in the dynamics after surgery rigidity and elasticity of implanted autocartilages in the side walls of the stomawas maintained, which was confirmed by the absence of lysis and suitability to perform the final stage of an extensive defect plasty of the trachea.
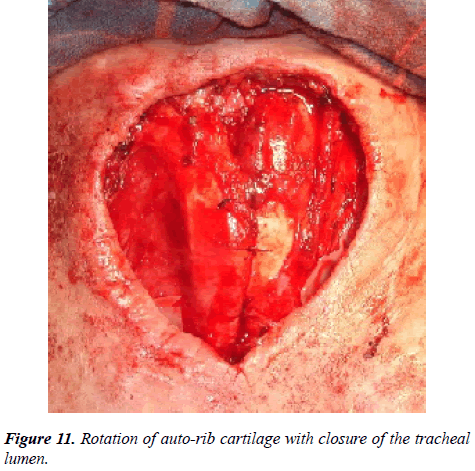
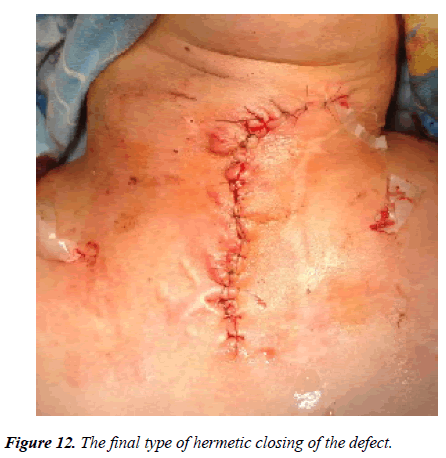
Under general intubation anesthesia, cuts were made on the right and left parallel to the walls of the stoma, previously implanted cartilages were mobilized with preservation of the leg (the lower wall of the formed encasement), cartilages were rotated with movement into the projection over the defect and implants were fixed with by absorbable atraumatic suture material (vicryl 4.0 or biosin 4.0) (Figure 11). The separated lateral flaps of skin with subcutaneous fat covered the surface of rotated autocartilages with rubber drainages (Figure 12).
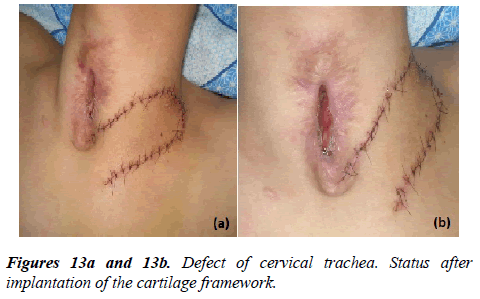
Below we give the following clinical example, where there was a need for several operations. Patient B., 18 years. An open traumatic brain injury of heavy st. Acute epidural hematoma in the left parietal-temporal region. Left temporal bone fracture with a transition to the base of the cranium. Craniotomy was performed in the left parietal-temporal region with removal of acute epidural hematoma (29.07.2013). Later on (05.08.2013) he was transferred to the neurosurgery center. On 07.08.2013 lower tracheostomy was performed. He received symptomatic, antibacterial, nootropic therapy. On 16.08.2013 the patient was discharged in a relatively satisfactory condition. On 03.09.2013, retracheostomy was made with the setting the T-shaped stent, 29.10.2013, laryngofissure, 24.01.2014, coagulation of granulations. On 11.03.2014, was an attempt to decannulation, unsuccessfully. He received outpatient therapy with a temporary positive effect. The patient was sent to the RSCPMCS, where TBFS was performed (17.06.2015): larynx is mobile, folds are symmetrical. 1.5 cm from the folds there is a tracheostomy zone with a defect along the front wall in length of 3.5 cm to 4.0 cm, with deformation and contraction of the back wall due to scars and granulation. Diameter 7 mm to 8 mm (5 hours after removing the T-tube). The trachea in the middle and lower third is not changed, 6.5 cm to carina. 26.11.2015 the operation was performed-plasty of trachea on T-shaped stent. In a satisfactory condition he was discharged for further observation. During the observation period, the granulation on the lateral walls of the trachea appeared again, so the patient was recommended to be hospitalized for surgical treatment - closing the anterior wall of the trachea with auto-rib cartilage. On 01.03.2016, plasty of defect of the anterior wall of the trachea by auto-rib cartilage. In the postoperative period on the 3rd day, the patient had stridorous breathing, at times a feeling of lack of air, a hysterical state. The patient underwent steroid and oxygen therapy with a temporary positive effect. TBFS (09.03.2016), larynx and folds mobile, symmetrical. In subglottic part of the larynx and upper third of the trachea on the anterior wall there is a skin insert, sealed. The tracheal lumen in the lower part of the skin insert is narrowed due to the prolapse of the skin-cartilage muscle flap into the lumen. Bronchoscope can pass this area, but the breathing is disrupted. The lumen diameter=6mm. Below the trachea and bronchi are normal. As there was a restenosis of area plastics by auto-rib cartilage patient underwent repeated operation of the plastic of the lumen of the trachea on a T-shaped stent with preservation of implanted previously auto-rib cartilage. The patient in a satisfactory condition was discharged for further supervision at the place of residence. At the control examination, the patient's condition improved, there was no stenosis. He was hospitalized for further examination and decision of treatment tactics (Figures 13a and 13b).
Diagnosis: Tracheo-laryngeal cicatricial-granulation restenosis. State after plasty of the anterior wall of the trachea by auto-rib cartilage (01.03.2016). State after plastic of the lumen of the trachea on a T-shaped stent with preservation of implanted previously auto-rib cartilage (10.03.2016).
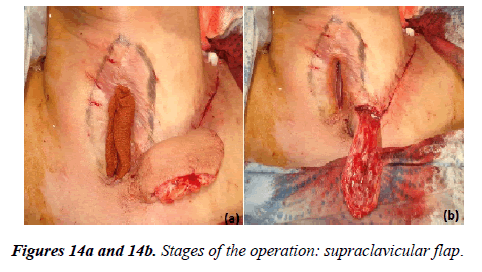
The patient underwent surgery: Plasty of defect of the trachea by supraclavicular flap in combination with autodermoplasty (Figures 14a and 14b).
In two patients after skin-muscle plasty and in 1 case after auto-rib plastics in the early postoperative period there was a partial failure of the seams with the flow of air from the zone created by the skin-muscle anterior wall without discrepancies of outer seams. In these cases, conservative methods have been achieved to eliminate the signs of insolvency of the seams with the termination of air flow in the phonation and cough with a sealed defect. In all other cases, good immediate and long-term results were obtained. On the control bronchoscopy, the zone of defect plasty covered with a skin insert was determined, without violation of patency and without narrowing of the tracheal lumen.
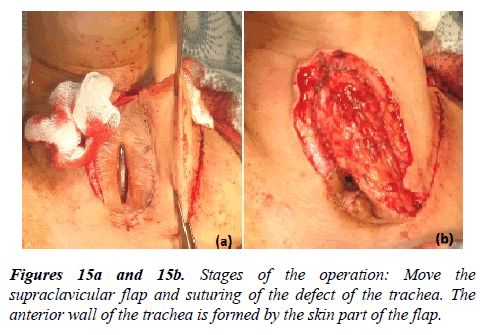
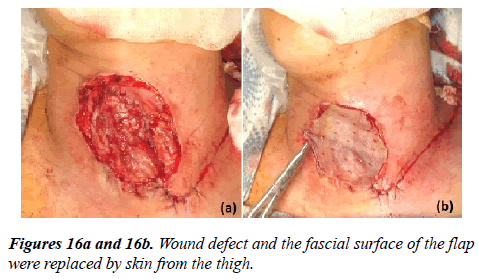
Thus, the choice of the method of plastic surgery or reconstruction of the tracheal defect is determined in each case individually. Local skin-muscle grafts as well as complex skinbone- muscle grafts from the adjacent neck area and various parts of the chest can be used. The indication for this operation is the presence of a persistent defect and formed tracheal lumen at this level, without signs of restenosis of the respiratory tract, the absence of inflammation and infection of the tissues around the stoma. When the size of the defect of the trachea up to 2 × 4 cm, a sufficient depth of the lumen of the trachea corresponding to the clearance above and below the stoma, the common axis of the trachea and the distal part of the larynx without displacement and deformation of the lumen we recommended a skin-muscle plasty of a defect with the substitution of local textiles (Figure 15{a,b} and 16{a,b}).
Conclusions
The presence of a large number of donor zones of arterialized flaps near the neck defects allows to use them widely for the plasty of extensive and persistent tissue defects. The use of an improved method of forming prefabricating flap, allows the plasticity of large defects of the trachea with reconstruction of the cartilaginous skeleton. The formation of rotational flaps, in particular, auto-rib cartilage and delta-pectoral flaps, for the reconstruction of extensive persistent defects of the trachea and soft tissues of the neck is technically simple, allows to create a frame of the front wall without disturbing the airway, without narrowing and deformation of the lumen.
References
- Milanov NO, Parshin VD, Trofimov EI. The results of the use of complex revascularizing of autotransplants in reconstructive surgery of the trachea. Ann Surg. 2005;6:27-30.
- Hashizume K, Kanamori Y, Sugiyama M, et al. Vascular-pedicled costal cartilage graft for the treatment of subglottic and upper tracheal stenosis. J Pediatr Surg. 2004;39(12):1769-71.
- Gudowsky LM, Milanov NO, Parshin VD, et al. Long-term results of elimination of extensive defects of the trachea with the aid of microsurgical technology. Prob Tubercul Dis lungs. 2006;3:18-23.
- Milanov NO, Trofimov EI, Parshin VD. Closure of large defects of the trachea using revascularizing prefabricating radiation skin and cartilage autograft. Ann Plastici Reconstruc Aesth Surg. 2006;4:109.
- Parshin VD, Milanov NO, Gudowsky LM, et al. Ten years of application of microsurgical techniques in reconstructive surgery of the trachea. Thorac Cardiovasc Surg. 2008;2:36-42.
- Topolnitskiy EB, Dambaev GC, Semichev EV, et al. Method of substitution graduate of defects of the trachea and larynx. Patent Invent. 2010;RUS:2440789.
- Milanov NO, Trofimov EI, Parshin VD, et al. Free revascularizable grafts in surgery of the trachea. Iss Reconst Plast Surg. 2007;3(4):79-82.
- Royer AK, Royer MC, Ting JY, et al. The use of a prefabricated radial forearm free flap for closure of a large tracheocutaneous fistula: a case report and review of the literature. J Med Case Rep. 2015;9:251-53.
- Tatur AA, Leonovich SI, Tchaikovsky VV, et al. Local plasty of tracheal defects in its stage reconstruction in patients with scar stenosis. Healthcar Minsk. 2007;4:32-6.
- Starka AV, Simonov SV, Muhamedov MR, et al. Plastic surgery of extensive trachea defects. Patent for invention. 2010;RUS:2453281.
- Soon-Hyun A, Myung-Whun S, Kwang Hyun K. Factors associated with taged reconstruction and successful stoma closure in tracheal resection end-to-end anastomosis. Arch Otolaryngol Head Neck Surg. 2004;130:57-62.
- Bockstein JS. Modification of the plastics of the double skin flap of the neck when the closure of the defects of the larynx and trachea. J Otolaryng. 1936;2:17-21.
- Bockstein JS. Surgical treatment of persistent stenosis of the larynx and trachea. Dis Dr Med Sciences. 1947.
- Bystrenin AV. Experience of restoration of the skeleton of the cervical trachea with the use of the half-rings from the rib autocartilage. J Otolaryng. 2005;1:41-3.
- Zenger VG. Reconstructive surgery of the larynx, pharynx, cervical trachea and esophagus. Dis Dr Med Scien. 1988;381.
- Jianxing He, Xin Xu, Manyin Chen, et al. Novel method to repair tracheal defect by pectoralis major myocutaneous flap. Ann Thorac Surg. 2009;88:288-91.
- Kamiyoshiara M, Nagashima T, Takeyoshi I. A novel technique for closing a tracheocutaneous fistula using a hinged skin flap. Surg Today. 2011;41(8):1166-68
- Watanabe Y, Umehara T, Harada A, et al. Successful closure of a tracheocutaneous fistula after tracheostomy using two skin flaps: a case report. Surg Case Repor. 2015,1:43-7.