Research Article - Biomedical Research (2018) Volume 29, Issue 3
Study on the influence of acupoints selection on ghrelin and GHSR expression in gastric fundus tissue of DGP rats
Zenghui Yue, Ping Li, Li Liu, Xiaoli Chen, Qiqi Wen, Xinran Wei, Yan Wang, Jianling Yuan* and Guoshan Zhang*
Hunan University of Chinese Medicine, Changsha, PR China
- *Corresponding Authors:
- Jianling Yuan
Hunan University of Chinese Medicine
Changsha, PR China
Guoshan Zhang
Hunan University of Chinese Medicine
Changsha, PR China
Accepted on November 13, 2017
DOI: 10.4066/biomedicalresearch.29-17-3125
Visit for more related articles at Biomedical ResearchAbstract
Objective: To explore the acupoint selection compatibility according to different departments and to study the influence on ghrelin and GHSR expression in the gastric fundus in rats with Diabetic Gastroparesis (DGP).
Methods: Sixty male SPF SD rats were given adaptive feeding for one week and were randomly divided into a blank control group, a model group, the Zusanli and Zhongwan (ZZ) group, the Zusanli and Neiguan group (ZN), as well as the Zusanli and non-meridian acupoint (ZNA) group, with 12 rats in each group. Except for the blank group, the other 48 rats were used to establish a DGP model by using streptozotocin. Acupuncture therapy was performed from the end of the tenth week for an additional four weeks. Then the rats were sacrificed and the serum and gastric fundus tissues were collected. ELISA assay was used to detect the ghrelin content in the serum. The expression of ghrelin positive cells in the gastric fundus tissue was detected by immunohistochemistry. The expression of ghrelin and GHSR mRNA in the gastric fundus tissue was detected by real-time PCR.
Results: Compared with the blank group, the food intake and the expression of ghrelin and GHSR mRNA in the gastric fundus tissue in the model group were significantly increased, while the small intestinal propulsion rate, the ghrelin content in the serum and the gray value of the gastric fundus were significantly decreased (P<0.05). Compared with the model group, the expression of ghrelin and GHSR mRNA in the gastric fundus tissue, the small intestinal propulsion rate, the ghrelin content in the serum and the gray value of the gastric fundus were significantly increased (P<0.05). Compared with the ZZ group, the food intake were significantly increased in the ZN and the ZNA groups (P<0.05), and the expression of ghrelin and GHSR mRNA in the gastric fundus tissue of rats were significantly increased (P<0.05) but the ghrelin content in the serum in ZN group was significantly decreased (P<0.05).
Conclusions: The improvement of gastrointestinal motility in DGP by acupuncture therapy was associated with the ghrelin content in the serum and GHSR expression in the gastric fundus. The treatment effect of local acupoints compatibility was better than that of the distal acupoints compatibility, and the acupoint selection according to department was one of the main influencing factors of acupoints compatibility.
Keywords
Acupoints compatibility, Acupoints selection according to the sections, Diabetic gastroparesis, Acupuncture therapy.
Introduction
Acupoints compatibility is a method of choosing two or more acupoints with the same effect to exert a synergistic effect, achieve a certain therapeutic effect, and improve clinical efficacy. This is based on traditional Chinese meridian theory, guided by the acupoint selection principle and combined with clinical and acupoints characteristics. However, there are three possibilities for acupoints compatibility of two or more acupoints including efficiency, inefficiency, and invalidity. Therefore, the appropriateness of acupoints compatibility is the key that affects clinical efficacy and mastering the influencing factors of acupoint compatibility is an important part of treatment [1-3]. In this study, we used acupoint selection according to department is one of the influence factors of acupoints compatibility as the hypothesis and the Diabetic Gastroparesis (DGP) as the disease model, and compared the difference between acupoints selection according to the meridian and acupoints selection according to the department. Our aim was to explore if acupoint selection according to department is one of the influencing factors of acupoints compatibility.
Diabetic Gastroparesis (DGP), the most common chronic complications of diabetes, refers to diabetic patients with clinical syndromes characterized by low gastric motility such as anorexia, early satiety, and nausea and vomiting [4]. At present, the pathogenesis of DGP has not been fully understood and results as a combination of multiple factors, and has been suggested to be related to abnormal secretion of gastrointestinal hormone (intestinal peptide or brain gut peptide) [5,6], decreased number of pacemaker cells [7], autonomic neuropathy [8] or hyperglycemia [9]. Currently, ghrelin and Growth Hormone Secretagogue Receptor (GHSR) have been getting more attention in studies concerning the pathogenesis of DGP. The main functions of ghrelin are stimulation of growth hormone secretion and regulation of energy balance. In addition, loss of weight caused by lowmedium caloric diet, exercise, anorexia nervosa, organ (heart, lung, kidney and liver) failure, or malignant tumor cachexia could lead to increased level of ghrelin [10,11]. It has been indicated that in addition to being a short-term signal for eating regulation, ghrelin is also a long-term signal for nutritional status. It also has the roles of promoting gastric acid secretion and gastrointestinal motility and protecting the digestive mucosa [12]. Besides, ghrelin also plays a role in gastrointestinal motility, gastrointestinal tract digestive enzyme secretion, and intestinal cell proliferation [13]. Therefore, this study mainly focused on the effect of acupoint selection according to department on the expression of ghrelin in the serum and gastric fundus tissue of diabetic rats with DGP.
Materials and Methods
Animals and grouping
Ethical approval was given by the medical ethics committee of Hunan University of Chinese Medicine with the following reference number: 2016004,Sixty SPF adult male Sprague Dawley (SD) rats weighing 200-220 g were provided by Hunan SJA Laboratory Animal Co., Ltd. (Certificate No.: SYXK2013 (Hunan)-0005). The rats with normal blood glucose were selected. The rats were fed in the SPF laboratory animal room of experimental animal center in Hunan University of Chinese Medicine, under the condition of temperature 22-25°C, humidity 40%-60%. After adaptive feeding for 1 w, the rats were randomly divided into a blank control group, a model group, the Zusanli and Zhongwan (ZZ) group, the Zusanli and Neiguan (ZN) group, as well as the Zusanli and non-meridian acupoint (ZNA) group, with 12 rats in each group. During the experiment, the disposal and operation of the animals complied with the guiding opinions on treating experimental animals promulgated by the Ministry of Science and Technology.
Main reagents and instruments
Streptozotocin (STZ) (Sigma, Cat.No.015H1492, U.S.A.); Trizol kit (Invitrogen, U.S.A.); blood glucose meter and blood sugar test paper (OneTouch SelectSimple, Johnson & Johnson, U.S.A.); Acupuncture needle (0.30 mm × 25 mm, Hua Tuo brand, Suzhou); violet spectrophotometer (UV-1800, Shimazduo, Japan); electrophoresis apparatus trophoresis (DDY-5, Beijing Liuyi Instrument Factory); gel document system (Bio-Red, U.S.A.); Centrifuge (Thermo Legend Micro 17 R, U.S.A.); PCR Instrument for Fluorescence Detection (Applied Biosystems, 7900 HT Fast, U.S.A.); Rabbit antimouse ghrelin antibody (1:2500) and Rabbit anti-human GHSR antibody (1:100) (the primary and secondary antibodies were purchased from Phoenix Biological Technology Co., Ltd.).
Modelling methods and evaluation
All the study rats fasted for 12 h. STZ was diluted in citric acid/sodium citrate buffer (PH 4.5, 4°C) with the concentration of 2% before using and then administered by a one-time injection in the left lower abdominal cavity in a concentration of 60 mmol/kg body weight. Random blood glucose was determined 72 h after the injection. The rats with random blood glucose level of ≤ 16.7 mmol/L were re-injected by using the same approach. The rats in the blank control group were injected with an identical volume of 0.1 mmol/L citric acid/ sodium citrate buffer. The rats were fed periodically at 10:00 am daily by ordinary animal feeds. During the 13 w of the experiment, the rats with random blood glucose level of ≤ 16.7 mmol/L were removed from the experiment. Success criteria of the DGP model were as follows [14]: the blood glucose level to be ≥ 16.7 mmol/L; the general conditions and stool characteristics of the rats to be significantly different from the blank group; the rate of gastric emptying and small intestinal propulsion rate in rats to be significantly different from the blank group.
Intervention methods
The location of acupoints: according to the Atlas of animal acupuncture and moxibustion [15] in “Experimental Acupuncture” edited by Zhongren and human imitation method, the acupoints of the rats were located as follows: Zhongwan: located in the linea alba, about 20 mm above the umbilicus. Zusanli: located in the underside of the knee joint, 5 mm away from the margo inferior of fibulae capitulum, with one on each side. Neiguan: located in the gap between the ulna and radius in the inside of the forelimbs, about 3 mm away from the wrist joint of the rat. Non-meridian acupoint: located in the medial elbow, midpoint of the connecting line between elbow and axillary.
In the blank and model groups: the rats were tied on the rat board, 30 min for each time, and once a day for 4 w. In the ZZ, ZN, and the ZNA groups: the corresponding points on both sides of the rats were selected and acupunctured with the depth of 0.3-0.5 cm following the conventional needle-insertion method with the needle retained for 30 min; the handmanipulation of the needle was performed every 10 min for lifting and thrusting, twirling, mild reinforcing, and attenuating. The range of lifting and thrusting was 0.3-0.5 cm, and the frequency was 60-90 times/min. The range and frequency of twirling were equal to those of lifting and thrusting. The needle was withdrawn 30 min at the end of the hand-manipulation procedure of the needle. This experiment was performed for 4 w.
Observed indexes and detection methods
The method for food intake determination: 300 g ordinary feeds were provided to the rats at 10:00 am daily. On the next day, the weight of the remaining feeds was recorded before feeding. Daily food intake in each cage of the rats was calculated as 300 g minus the weight of the remaining feeds.
Blood glucose measurement: Blood samples were collected from the vena caudalis per week for detection of the blood glucose by using blood glucose meter and blood glucose test paper.
Determination of small intestine propulsion rate: The rats were fasted for 24 h after the last injection. Intragastric administration was performed in each group of the rats with black ink at a dose of 1 ml/100 g body weight. Then the rats were sacrificed and the abdominal cavities were opened at 20 min after the intragastric administration. The small intestine from the pylorus to the ileocecal bowel was gently extracted with tweezers and placed on a tray. The small intestine was gently pulled into a straight line and the gastrointestinal propulsion index was measured by ruler. The gastrointestinal propulsion index was calculated by the following formula:
Small intestinal propulsion rate=the distance from the front of ink marking to the front end of the range × 100% (cm)/h sphincter to the small intestine end distance (cm).
ELISA assay: 4 ml blood from the rats’ hearts were collected after anesthesia and placed in the centrifuge tube without anticoagulant (for determination of serum ghrelin). While whole blood samples were placed at 4°C overnight and then centrifuged at 1000 round/min for 20 min. The supernatant was absorbed and stored at in -20°C or -80°C; repeated freezing and thawing was avoided. The ELISA assay was performed strictly according to the kit instructions.
Immunohistochemistry: The gastric tissues were extracted and cut into 4 mm pieces, then, post fixed in paraformaldehyde buffer for 8 h and washed with the tap water, which was followed by 20% to 30% sucrose gradient dehydrated and liquid nitrogen frozen after tissue embedding. Then, 10 μm serial sections were prepared by using the cryostat freezing microtome and placed on the slides with poly-lysine. The immunohistochemical staining of ghrelin and GHS-R was performed by using the SABC method. Among which, rabbit anti-mouse ghrelin antibody (1:2500) and rabbit anti-human GHS-R antibody (1:100) were used as primary antibodies. The expression of ghrelin and GHS-R were observed by microscope under high magnification after DAB developing and neutral gum sealing. Ten fields of view were selected in each slice under high magnification (400X), and the average value was considered as the average gray value of the slice.
Real-time fluorescent quantitative PCR: Determination of ghrelin and GHSR mRNA expression level in the gastric fundus: the tissue of the gastric fundus were collected and stored at -80°C for determination. (1) RNA extraction: The total RNA of the rat gastric fundus was extracted by Trizol extraction kit according to the manufacturer’s instructions and analysed by 1.5% agarose gel electrophoresis. The concentration and purity of extracted RNA were calculated by measuring the OD 260 and OD 280. The concentration of RNA in our study was above 1.5 μg/μL, and the purity was between 1.8 and 2.1, which indicated that the quality of extracted RNA was reliable. (2) cDNA synthesis: cDNA reverse transcription was performed by using SuperScript III reverse transcription reagent kit. (3) PCR amplification: using β-actin as internal control, the primers are shown in Table 1. The amplification conditions were as the follows: 10 min initial denaturation at 95°C, 40 cycles of each 10 s denaturation at 95°C, 60 s annealing/extension at 60°C (fluorescence collection). After the amplification reaction, the conditions were as the follows for establishing the dissolution curve of PCR products: 10 s at 95°C, 60 s at 60°C, 15 s at 95°C, then slowly heated from 60°C to 99°C. (4) Relative expression level was quantified by using the relative quantitative 2-ΔΔCt method, ΔCt=Ct simple target gene-Ct simple β-actin gene, ΔΔCt =ΔCt-averaged Ct blank control group.
| Primer | Primer sequences | Length of amplified products (bp) |
|---|---|---|
| β-actin | F: 5'-CCTGTACGCCAACACAGTG-3' | 211 |
| R: 5'-ATACTCCTGCTTGCTGATC-3' | ||
| Ghrelin | F: 5'-ATCCAAGAAGCCACCAGCTA-3' | 121 |
| R: 5'-GAAGGGAGCATTGAACCTGA-3' | ||
| GHSR | F: 5'-CTCTACACCCGAAGCCGTAG-3' | 118 |
| R: 5'-CTGCCCATCTGGCTCTACTC-3' |
Table 1. Primer sequences and the length of amplified products.
Statistical analysis
SPSS 17.0 statistical software was used for data analysis. Data followed normal distribution were represented as x? ± s. If the data followed normal distribution and were homogeneity of variance, one way ANOVA and LSD test were used for multigroup comparison and the post hoc test, respectively. The Tamhane T2 test was used if heterogeneity of variance. Skewness distribution data were represented as Median (M) and Interquartile Range (QR), and the rank-sum test was used for comparison among groups. A value P<0.05 was considered significant difference.
Results
Comparison of general signs in the study rats
During the experiment, the rats in the blank group showed good mental state, normal locomotor behavior, sensitive response, healthy eating, milky white and glossy fur, and normal cacation and emiction. Polydipsia, polyphagia, and polyuria appeared in the rats of the ZZ, ZN, and the ZNA groups three days after STZ injection. The DGP rats showed poor mental state [16], slow behavioral activity, slow growth of body mass and even reduced body mass from the third week, unpolished fur, changed stool property, unpleasant odor, and abdominal swelling in the sixth week. Mortality status: one rat in the blank group, three rats in the model group, two rats each in in the ZZ and the ZN group, and three rats in the ZN group.
Comparison of the effect of acupoint selection according to department on food intake in rats
The results depicted in Table 2 suggested that compared with the blank group, the food intake was significantly increased in the model group, the difference was statistically significant (P<0.05); compared with the model group, the food intake was significantly increased in the ZNA group (P<0.05) but not in the ZZ or the ZN groups (P>0.05); compared with the ZZ group, the food intake was significantly increased in the ZN and ZNA groups, with statistical significance (P<0.05). These results indicated that local acupoints compatibility was capable of reducing the food intake of DGP rats, while distal acupoints compatibility showed no significance in the change of food intake, and the non-meridian acupoint was capable of increasing the food intake of DGP rats.
| Group | n | Food intake (g/d) |
|---|---|---|
| Blank group | 11 | 104.73 ± 13.57 |
| Model group | 9 | 230.86 ± 19.10* |
| Zusanli and Zhongwan group | 10 | 213.65 ± 29.58 |
| Zusanli and Neiguan group | 10 | 240.04 ± 15.99? |
| Zusanli and non-meridian acupoint group | 9 | 250.41 ± 20.89?? |
Note: compared with blank group, *P<0.05; compared with model group, ?P<0.05; compared with Zusanli and Zhongwan group, ?P<0.05.
Table 2. Comparison of the effect of acupoint selection according to department on food intake in rats (x? ± s).
Comparison of the effect of acupoint selection according to department on small intestinal propulsion rate in rats
The results illustrated in Table 3 indicate that compared with the blank group, the small intestinal propulsion rate was significantly decreased in the model group, the difference was statistically significant (P<0.05), which indicated the successful modeling of the DGP disease model; compared with the model group, the small intestinal propulsion rate was significantly increased in the ZZ, ZN, and the ZNA groups (P<0.05). However, there was no significant difference among the three treatment groups (P>0.05). These results indicated that the small intestinal propulsion rate of DGP rats could be improved in the three treatment groups, the effect of local acupoints compatibility was better than that of distal acupoints compatibility, and the effect of the latter was better than that of non-meridian acupoint.
| Group | n | Propulsion rate |
|---|---|---|
| Blank group | 11 | 0.73 ± 0.05 |
| Model group | 9 | 0.60 ± 0.05* |
| Zusanli and Zhongwan group | 10 | 0.73 ± 0.05? |
| Zusanli and Neiguan group | 10 | 0.70 ± 0.06? |
| Zusanli and non-meridian acupoint group | 9 | 0.69 ± 0.05? |
Note: compared with blank group, *P<0.05; compared with model group, ?P<0.05.
Table 3. Comparison of the effect of acupoint selection according to department on small intestinal propulsion rate in rats (x? ± s).
Comparison of the effect of acupoint selection according to department on ghrelin content in the serum of rats
The results shown in Table 4 suggest that compared with the blank group, the ghrelin content in the serum was significantly decreased in the model group, the difference was statistically significant (P<0.05), which indicated the successful modeling of the DGP disease model; compared with the model group, the ghrelin content was significantly increased in the ZZ and the ZNA groups (P<0.05) but not in the ZN group (P>0.05); compared with the ZZ group, the ghrelin content was significantly decreased in the ZN group, with statistical significance (P<0.05). These results indicated that the effect of local acupoints compatibility and non-meridian acupoint were better than that of distal acupoints compatibility on regulation of ghrelin content in serum.
| Group | n | Concentration (ng/ml) |
|---|---|---|
| Blank group | 11 | 2380.79 ± 176.02 |
| Model group | 9 | 1795.74 ± 65.48* |
| Zusanli and Zhongwan group | 10 | 2019.51 ± 210.72? |
| Zusanli and Neiguan group | 10 | 1836.65 ± 170.67? |
| Zusanli and non-meridian acupoint group | 9 | 1978.10 ± 147.81? |
Note: compared with blank group, *P<0.05; compared with model group, ?P<0.05; compared with Zusanli and Zhongwan group, ?P<0.05.
Table 4. Comparison of the effect of acupoint selection according to department on ghrelin content in the serum of rats (x? ± s).
Comparison of the effect of acupoint selection according to department on gray value of ghrelin in the gastric fundus of the study rats
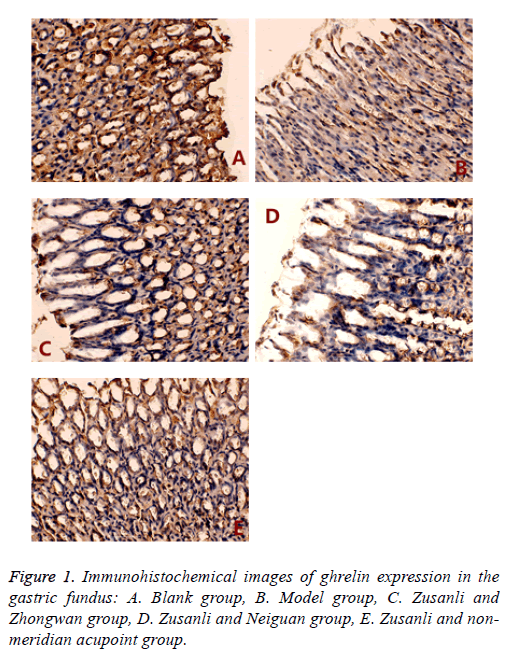
The changes in the immunohistochemical changes of ghrelin expression in the gastric fundus are depicted in Figure 1.
The results (Figure 1 and Table 5) suggested that compared with the blank group, the gray value of ghrelin in the gastric fundus was significantly decreased in the model group, the difference was statistically significant (P<0.05); compared with the model group, the gray value of ghrelin was increased in the ZZ, ZN, and the ZNA groups, the difference were found to be statistically significant (P<0.05); compared with the ZZ group, the gray value of ghrelin was significantly decreased in the ZNA group (P<0.05) but not in the ZN group (P>0.05). These results indicated that the treatment effect of local and distal acupoints compatibility were better than that of the nonmeridian acupoint.
| Group | n | Gray value |
|---|---|---|
| Blank group | 11 | 161.23 ± 0.89 |
| Model group | 9 | 71.29 ± 35.43* |
| Zusanli and Zhongwan group | 10 | 158.40 ± 15.55? |
| Zusanli and Neiguan group | 10 | 157.47 ± 37.97? |
| Zusanli and non-meridian acupoint group | 9 | 129.43 ± 18.56??# |
Note: compared with the blank group, *P<0.05; compared with the model group, ?P<0.05; compared with the Zusanli and Zhongwan group, ?P<0.05; compared with the Zusanli and Neiguan group, #P<0.05.
Table 5. Comparison of the effect of acupoint selection according to department on gray value of ghrelin in gastric fundus of DGP rats (x? ± s).
Comparison of the effect of acupoint selection according to department on ghrelin and GHSR mRNA expression in the gastric fundus of the study rats
| Group | n | Ghrelin | GHSR |
|---|---|---|---|
| Blank group | 11 | 23.71 ± 0.62 | 22.79 ± 0.35 |
| Model group | 9 | 24.30 ± 0.03 | 24.62 ± 0.19* |
| Zusanli and Zhongwan group | 10 | 22.54 ± 0.12? | 22.67 ± 0.35? |
| Zusanli and Neiguan group | 10 | 23.11 ± 0.17?? | 23.67 ± 0.31?? |
| Zusanli and non-meridian acupoint group | 9 | 23.53 ± 0.96 | 23.00 ± 0.42?# |
Note: compared with blank group, *P<0.05; compared with model group, ?P<0.05; compared with Zusanli and Zhongwan group, ?P<0.05; compared with Zusanli and Neiguan group, #P<0.05.
Table 6. Comparison of the effect of acupoint selection according to department on ghrelin and GHSR mRNA expression in gastric fundus of DGP rats (x? ± s).
Table 6 results show that compared with the blank group, the expression of GHSR mRNA in the gastric fundus tissue was increased in the model group, the difference was statistically significant (P<0.05); compared with the model group, both ghrelin and GHSR mRNA expression in the gastric fundus tissue were decreased in the ZZ and ZN groups, the GHSR mRNA expression was decreased in the ZNA group, the difference in both were statistically significant (P<0.05); compared with the ZZ group, both of the ghrelin and GHSR mRNA expression in the gastric fundus tissue were increased in the ZN group, with statistical significance (P<0.05); compared with the ZN group, GHSR mRNA expression in the gastric fundus tissue was decreased in the ZNA group, with statistical significance (P<0.05).
Discussion
In this study, we used acupoint selection according to department is one of the influence factors of acupoints compatibility as the hypothesis, the DGP as the disease model, acupoints selection according to the meridian and local acupoints selection according to the department as the treatment groups, and distal acupoints selection according to the department and non-meridian acupoint as the controls for comparison. DGP induced syndromes such as nausea, vomiting and abdominal distension belong to the category of traditional Chinese medicine such as “vomit” and “nausea”. Traditional Chinese medicine considered the DGP syndrome to be a result of spleen and stomach's ascending and descending dysfunction. The spleen is deficit in ascending and the stomach is deficit in descending, which lead to being unable to distinguish between the clear and the muddy, and belong to the spleen and stomach diseases. Our research group reviewed the relevant clinical literatures available in the last five years on acupuncture treatment of DGP. We found that the most frequently used acupoint was the Zusanli which belongs to the Yangming Stomach Meridian of Foot (the percentage of the total frequency was 15.53%). So we chose Zusanli according to the Meridian. Acupoint selection according to department includes two kinds of acupoints, the local and the distal acupoints. So literature analysis-derived 41 acupoints which were commonly used in the treatment of DGP was used in this study and divided into two groups. The most frequently used acupoint in each group was selected: Zhongwan (local) and Neiguan (distal). Therefore, a comparative study was performed in this research by using the healthy SPF rats as the blank group, the DGP model rats as the model group, ZZ group as the treatment group, and the ZN and ZNA groups as the control groups. We then compared the treatment effect among local acupoints, distal acupoints and non-meridian acupoint to guide the clinical work.
The main manifestations of patients with DGP are the disappearance of MMCIII period, pylorospasm, uncoordinated contraction among sinuses ventriculi, pylorus and duodenum, and delayed gastric emptying. Therefore, the gastrointestinal propulsion rate is commonly used as a standard to evaluate the DGP model. The results of comparison in our study were as the follows: compared with the blank group, the intestinal propulsive rate was decreased significantly in the model group; compared with the model group, the intestinal propulsive rate was increased significantly in the ZZ, ZN, and the ZNA groups, which indicated that the therapy in the three treatment groups had a promoting effect on the gastrointestinal propulsion rate.
Ghrelin is a newly discovered endogenous ligand of the Growth Hormone Secretagogue Receptor (GHSR), which is secreted into the blood by the gastric fundus. Since Kojima et al. first found this brain gut peptide in mice and human gastric endocrine cells and the hypothalamic arcuate nucleus, several studies in recent years have reported that ghrelin play an important role in a variety of tissues and provides immunity [17,18]. A large number of studies [19,20] showed that acupuncture and other traditional Chinese medicine treatments could improve gastrointestinal function by regulating the expression of ghrelin.
The effect of acupoint selection according to department on the expression of ghrelin and GHSR in serum and the gastric fundus of DGP rats suggested that the effect of the local acupoint (Zhongwan) on food intake regulation, ghrelin content in serum, and ghrelin and GHSR mRNA expression in the gastric fundus of DGP rats were better than those of the distal acupoint (Neiguan); and the effect of the local acupoint (Zhongwan) on regulation of small intestine propulsion rate and expression of ghrelin positive cells in the gastric fundus were better than those of the distal acupoint (Neiguan), which confirmed that acupoint selection according to department is one of the influencing factors of acupoints compatibility. In our study, we used spleen and stomach disease as the carrier, Zhongwan as the research object, and Neiguan and nonmeridian acupoint as the controls for drawing this conclusion. Whether the acupoint selection according to department had the same advantages in the treatment of the lesions in other organs or parts are yet to be further verified.
Chen et al. [21] found that in the early stage of DM, a large amount of ghrelin is secreted into blood from the gastric fundus, which results in increased contraction frequency of the pylorus and the frequency of gastric emptying. In the late stage of diabetes, plasma ghrelin is decreased, which might be associated with anorexia, muscle atrophy, decreased body mass, or even gastric paralysis. Clinical studies have shown that patients with DGP have decreased serum ghrelin content [22]. The results in our study suggested that the content of serum ghrelin in the model group was lower than that in the blank group; our results are consistent with the previous literature.
The results of this study showed that the protein content and gene expression of ghrelin and GHSR in the gastric fundus of the DGP model were higher than those of the blank group. A previous study [23] showed that the protein content and gene expression of ghrelin and GHSR in the gastric fundus of DGP model were decreased, which was not consistent with our findings. At present, no uniform conclusion has been drawn about the time for the establishment of the DGP model and, further, each experiment has different modelling methods. The time for the establishment of the DGP model were varied in previous studies which mostly focused on the time from 4 w to 12 w [24-26]. Therefore, the increased expression of ghrelin in the model group in our study was not consistent with the previous literatures, which might be due to the difference of method and time for the establishment of the DGP model. In addition, as one of the gastrointestinal hormones, whether the level of ghrelin is completely consistent with gastric motility in the progress of the DGP model has not been reported yet. Further experimental studies are needed to demonstrate this phenomenon.
Conclusion
The improvement of gastrointestinal motility in DGP by acupuncture therapy seems to be associated with the ghrelin content in the serum and GHSR expression in the gastric fundus. Local acupoints compatibility was better than that of the distal acupoints compatibility for acupoint selection, and the results of this study confirm that acupoint selection according to department is one of the main influencing factors of acupoints compatibility.
Funding
This work was supported by the National Basic Research Program of China (No: 2014CB543102 and No. 2015CB554502), the National Natural Science Foundation of China (No. 81673886 and No. 81603705).
Competing Interests
The authors declare that no competing interests exist.
References
- Zheng J, Chen B, Guo Y, Guo Y. Analysis on the factors that cause the difference of acupoints synergy effect. Zhongguo Zhen Jiu 2015; 35: 719-722.
- Zhang G, Liu H, Wang F. Acupoint combination and acupuncture-moxibustion prescription. Zhongguo Zhen Jiu 2014; 34: 987-990.
- Shi Y, Shan C, Wang F. Acupoint selection: a key factor to influence the compatibility of acupoint. Zhongguo Zhen Jiu 2015; 35: 1025-1027.
- Ma H, Gao X, Lin HD. Glycated haemoglobin in diagnosis of diabetes mellitus and pre-diabetes among middle-aged and elderly population: shanghai Changfeng study. Biomed Environ Sci 2013; 26: 155.
- Lund A, Knop FK, Vilsboll T. Glucagon-like peptide-1 receptor agonists for the treatment of type 2 diabetes: differences and similarities. Eur J Intern Med 2014; 25: 407-414.
- Tong J, Dalessio D. Give the receptor a brake: slowing gastric emptying by GLP-1. Diabetes 2014; 63: 407-409.
- OGrady G, Abell T L. Gastric arrhythmias in gastroparesis: low- and high-resolution mapping of gastric electrical activity. Gastroenterol Clin North Am 2015; 44: 169-184.
- Tang M, Donaghue KC, Cho YH. Autonomic neuropathy in young people with type 1 diabetes: a systematic review. Pediatr Diabetes 2013; 14: 239-248.
- Phillips LK, Deane AM, Jones KL. Gastric emptying and glycaemia in health and diabetes mellitus. Nat Rev Endocrinol 2015; 11: 112-128.
- Espelund U, Hansen TK, Hojlund K. Fastin gun masksa strong in verse association between ghrelinand cortiso linserum: studies in obese and normal-weight subjects. Clin Endocrinol Metab 2005; 90: 741-746.
- Schubert ML. Gastric exocrine and endocrine secretion. Curr Opin Gastroenterol 2009; 25: 529-536.
- Poitras P, Tomasetto C. The potential of ghrelin as a prokinetic. Regul Pept 2009; 155: 24-27.
- Ryszard P, Magdalena OG, Jerzy C, Violetta SP. Sports training and circulating adipokine levels. Postepy Hig Med Dosw 2013; 67: 35-42.
- Lin G, Zhang J, Li L, Zou Z, Chen C, Xue L, Zhao L. Effect of electroacupuncture on gastric interstitial cells of Cajal in a rat model of diabetic gastroparesis. Exp Ther Med 2016; 11: 2489-2494.
- Zhongren L. Experimental acupuncture. Beijing: China Press of Traditional Chinese Medicine 2007; 255-257.
- Kojima M, Hosoda H, Date Y. Ghrelin is a growth hormone-releasing acylated peptide from stomach. Nature 1999; 402: 656-660.
- Bazhanov N, Ylostalo JH, Bartosh TJ. Intraperitoneally infused human mesenchymal stem cells form aggregates with mouse immune cells and attach to peritoneal organs. Stem Cell Res Ther 2016; 7: 27.
- Sakurazawan MN. Effects of intracerebroventricular ghrelin on food in-take and Fos expression in the arcuate nucleus of the hypothalamus in female rats vary with estrous cycle phase. Neuro Sci Lett 2013; 541: 204-208.
- Zhou L, Cheng YP. Effect of Electroacupuncture on expression of ghrelin and mRNA expression of its receptor in functional dyspesia rats. Zhongguo Zhong Xi Yi Jie He Za Zhi 2016; 36: 322-326.
- Lin YP, Wan QQ, Peng Y, He FE, Shen J. Effect of electroacupuncture at Zusanli (ST 36), etc. on gastrointestinal motility and expression of ghrelin mRNA and growth hormone secretagogue receptor mRNA in diabetic gastroparesis rats. Zhen Ci Yan Jiu 2015; 40: 290-295.
- Chen CY, Fujimiya M, Laviano A, Chang FY, Lin HC, Lee SD. Modulation of ingestive behavior and gastrointestinal motility by ghrelin in diabetic animals and humans. J Chin Med Assoc 2010; 73: 225-229.
- Tack J, Vanormelingen C. Management of gastroparesis: beyond basics. Curr Treat Opt Gastroenterol 2014; 12: 468-477.
- Yang CG, Wang WG, Yan J. Gastric motility in ghrelin receptor knockout mice. Mol Med Rep 2013; 7: 83-88.
- Zhang H, Miao FR, Luo YY, Liu JL, Fan YS. Effect of moxibustion with ignited Zhuang-medicine medicated-thread on interstitial cells of Cajal in gastric antrum in diabetic gastroparesis rats. Zhen Ci Yan Jiu 2015; 40: 104-118.
- Jing Q, Wu GT, Du LD, Liu WZ, Li YD, Ren Y. Therapeutic effects of ethanol extracts of Angelica sinensis and Astragalus mongholicus in diabetic gastroparesis rats. Zhong Yao Cai 2014; 37: 1415-1420.
- Xu L, Li Z, Guo F. Curcumin improves expression of ghrelin through attenuating oxidative stress in gastric tissues of streptozotocin-induced diabetic gastroparesis rats. Eur J Pharmacol 2013; 718: 219-225.