Research Article - Biomedical Research (2017) Volume 28, Issue 7
Reverse LISS plate in treating femoral intertrochanteric fractures: A review of 22 cases
Hong-Wei Chen1* and Jun Pan21Department of Orthopaedics, Yiwu Central Hospital, Wenzhou Medical University, Yiwu, Zhejiang Province, China
2Department of Orthopaedics, Second Affiliated Hospital, Wenzhou Medical University, Wenzhou, Zhejiang Province, China
- *Corresponding Author:
- Hong-Wei Chen
Department of Orthopaedics
Yiwu Central Hospital
Wenzhou Medical University, China
Accepted on November 28, 2016
Abstract
Background: This study aimed to evaluate the treatment effects of reverse Less Invasive Stabilization System (LISS) on femoral intertrochanteric fractures.
Methods: A total of 22 cases with femoral intertrochanteric fractures were treated with reverse LISS. The period from injury to operation was 3-14 days.
Results: The haemorrhage was 130.5 ± 60 ml during the surgery and the operation time was 55 ± 15 min. The fracture healing time was 10-27 W (average 13.4 W). According to the Harris functional scoring, the results were excellent in 11, good in 8, fair in 2 and poor in 1, excellent and good rate of clinical results were 86.4%. 2 cases developed discomforts and pains in greater trochanter. Plate collapse was found in 1 case by X-ray 6 months following surgery. Fortunately, no further treatment was required for fracture malunion. The rest 19 cases had no surgical site infection, no varus deformity of hip, any implant failure and displacement of fracture, no backing out or loosening of the locking screws.
Conclusions: Reverse LISS plate is an effective way for femoral intertrochanteric fractures, although there is certain failure rate. In order to improve the clinical effect, intraoperative normative operation and avoiding early weight bearing are very important.
Keywords
Femoral intertrochanteric fractures, Fracture fixation, Internal, LISS.
Introduction
Femoral Intertrochanteric Fracture (FIF) is one of most common diseases in older people. Many materials and measures are available for internal fixation of such fracture. Therefore, there is no one-size-fit-all option. Whether the extra-medullary fixation surpass the intramedullary fixation remains to be debated [1-6]. Minimally invasive technology has been widely used in traumatic orthopaedics in recent years. Proximal Femoral Nail Anti-Rotation (PFNA) for closed reduction is the first choice for the treatment for FIFs [7]. Unfortunately, the results of intramedullary nail are not always favourable. Intramedullary implant for unstable fractures is more likely to cause complications such as poor reduction, secondary distal femoral fracture, lag screw cutting, introversion and malformation of hip joint. In a study conducted by Simmermacher et al. 315 cases with PFNA fixation were treated with PFNA fixation and 6.5% of them developed complications including acetabular penetrations, lateral displacement of screw blade, loosening, intramedullary rupture, rotational deformity, ipsilateral femoral shaft fractures and delayed healing [8]. Less Invasive Stabilization System (LISS) is a plate system that integrates screw locking, minimally invasive technology and biological fixation.
Recently, reverse femoral LISS plate has been used by some researchers for treatment of hip fractures and other special cases [9-13]. Whether the result of LISS for the treatment of FIF is satisfactory is still under controversy. We treated a total of 22 cases with FIF with reverse LISS plate in our hospital from January 2008 to January 2013. The results were favourable and reported as follows.
Materials and Methods
Ethical considerations
This study has been approved by the Ethics Committee of Affiliated Yiwu Central Hospital of Wenzhou Medical College (Reference Number: 2014-10-9A).
Inclusion and exclusion criteria
Patients in accordance with following criteria were included: 1) single fracture; and 2) new closed intertrochanteric fracture with follow-ups. Patients in accordance with following criteria were excluded: 1) multiple fractures; 2) a history of hip disease; and 3) not cooperating with treatments.
General data
There were 22 patients enrolled in this study, including 12 males and 10 females, ranging from 44 to 86 years old with an average of 72.5 years old. 8 cases had left fractures and 14 had right fractures. For traumatic causes, 15 had a fall, 4 had a traffic accident and 3 had a fall from height. According to Evans-Jensen classification [14], there were 13 type III fractures and 9 type IV fractures. All fractures were closed fractures. 12 cases had coexisting medical conditions including 6 cases with high blood pressure, 4 cases with diabetes, and 4 cases with coronary heart disease. 2 cases had multiple coexisting medical conditions. The period from injury to operation was 3-14 days, with an average of 5.3 days.
Preoperative preparation
Physical examinations and routine laboratory tests were performed after admission. Patients were also assessed for heart, lung and brain function. Patients received active treatment for complications. When patients were stable with normal blood pressure (measured every 2 hours), haemoglobin>90 g/L as well as fasting blood glucose<10.0 mmol/L, they were assessed for the risk of anaesthesia prior to the surgery.
Procedures
Patients received routine antibiotics before surgery. Then, patients were subject to general anaesthesia or epidural anaesthesia. They were positioned supine on the traction table and closed reductions were performed. After satisfactory alignment and collodiaphyseal angle were observed under C-arm X-ray device, the traction was maintained.
A 4-6 cm long incision was made over the greater trochanter. For fracture with greater displacement, especially for those with fracture fragments in medial and medial posterior lesser trochanter of femur, the anatomical reduction should be preferred as much as possible to regain consistency of medial and medial posterior bone cortex. After the incision, a submuscular tunnel was made on the femoral surface. A contralateral femoral LISS plate of appropriate length was submuscularly inserted to the femur, without stripping the periosteum. The LISS plate was correctly placed with the help of inserted handle and radiograph. To expose plate, a small incision was made on the distal end. To match with the anterior arch of the femur, the plate was temporarily fixed in the center of lateral femur using bone forceps. The back and forth, rotating force line and length of low extremities were examined. If any deformity of force line or variance in length of lower extremities were found, another reduction should be performed. The Krischner wire was used for temporary fixation of the plate. It was inserted through Hole A. The guidewire was inserted at 1/3 below the femoral neck on the anteriorposterior view and in the center of the femoral neck on the lateral view Based on age and bone mass; 4-6 locking screws were placed at proximal end of the fracture. 4 bicortical or unicortical angle-stabilized screws were required at the distal end of the fracture. The optimum positioning and length of screws were observed on the radiograph. Finally, the closed incision was washed.
Postoperative treatment
All patients were treated with low molecular weight heparin for anticoagulation after surgery. 24 h after surgery, patients were able to rise from bed and practiced isometric contraction of quadriceps femoris. 2 d following surgery, the patients were advised to sit in semi-Fowler's position and move within the bed. 10-14 d following surgery, the sutures were removed if the wound was normally healed. 6 weeks after surgery, the patients exercised with weights which became step-wise heavier from 10-15 Kg. 3-6 months later, the patients took workout with full weight, which was dependent on the severity of fracture and callus shown by the radiography. They were also guided for out-of-bed activities based on healing of fracture. The medical conditions and complications should be noted and treated without delay. The elderly with poor physical fitness and severe osteoporosis were not suitable for early workout with weight.
Outcome assessment criteria
According to the Harris hip score which includes four items such as pain (44), function (47), lower limb malformation (4), hip mobility (5), full mark (100), the results were excellent for a score of ≥ 90, good for 80-89, fair for 70-79 as fair and poor for<70, respectively [15].
Results
The intraoperative blood loss was 130.5 ± 60 ml (70-340 ml). The operative time was 55 ± 15 min (40-110 min). 22 cases were followed up for 12-30 (average 14.8) months. The fracture healing time was 10-27 weeks (average 13.4 weeks) no death or major medical complications occurred. According to the Harris functional scoring, the results were excellent in 11, good in 8, fair in 2 and poor in 1. The excellent and good rate of clinical results was 86.4%. 2 cases developed discomforts and pains in greater trochanter. Plate collapse was found in 1 case by X-ray 6 months following surgery.
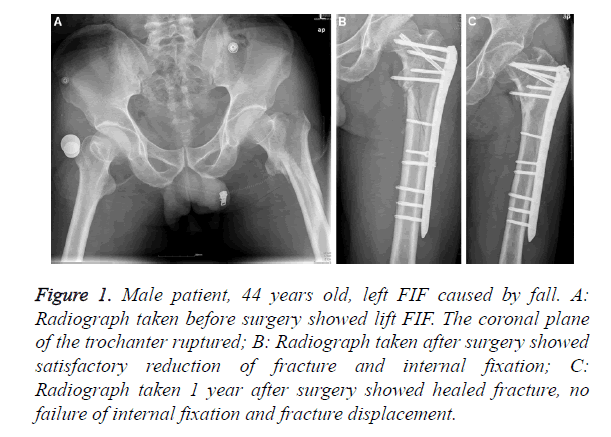
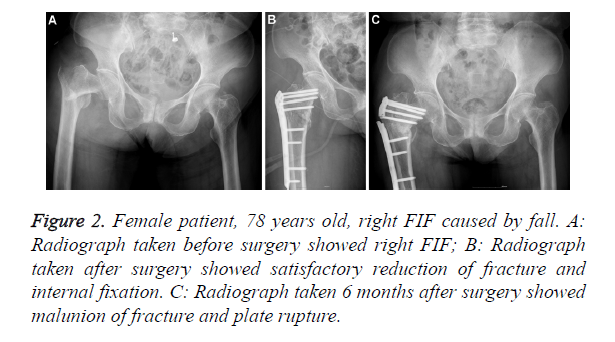
Fortunately, no further treatment was required for fracture malunion. The rest 19 cases had no surgical site infection, no varus deformity of hip, any implant failure and displacement of fracture, no backing out and loosening of the locking screws, as shown in Figures 1 and 2.
Figure 1. Male patient, 44 years old, left FIF caused by fall. A: Radiograph taken before surgery showed lift FIF. The coronal plane of the trochanter ruptured; B: Radiograph taken after surgery showed satisfactory reduction of fracture and internal fixation; C: Radiograph taken 1 year after surgery showed healed fracture, no failure of internal fixation and fracture displacement.
Figure 2. Female patient, 78 years old, right FIF caused by fall. A: Radiograph taken before surgery showed right FIF; B: Radiograph taken after surgery showed satisfactory reduction of fracture and internal fixation. C: Radiograph taken 6 months after surgery showed malunion of fracture and plate rupture.
Discussion
Feasibility of Reverse LISS for FIF
FIF is a common clinical injury, accounting for 50% of proximal femoral fractures. The incidence of unstable fractures was up to 60% [9]. FIF often coexists with medical conditions and osteoporosis. Non-surgical treatments may cause many severe complications such as lung infection, urinary tract infection, deep venous thrombosis and pain leading to fracture malunion and functional limitations, possibly due to long rest in bed and traction. Early internal fixation is first choice for these fractures. It enables early mobility, early recovery and prevention from complications. Although treatment technology and internal fixation for FIF is getting better, failure of fixation is still a problem. The treatment of FIF is a challenge in traumatic orthopaedics. Different implants have been recently designed to treat these fractures. Which one are the best remains controversial [16]. There major treatments include extra-medullary fixation and intramedullary fixation. From biomechanics, intramedullary nail device is more stable and has shorter force army under load, which is recommended for treatment of unstable FIF [17]. D'Arrigo et al. treated 51 unstable FIF cases with PFNA and suggested PFNA had advantages such as shorter operative time, less trauma, less blood loss, higher fracture healing rate and fewer complications [18]. However, use of intramedullary nail in splintered fracture may cause a variety of complications including non-union, delayed union, varus deformity, damage of nervous peroneus communis, intraoperative fracture of femoral shaft, fracture of trochanter major, perforation of neck of femur or knee and collapse of internal fixation [19]. Although intramedullary fixation is stronger from the biomechanics and more suitable to prevent displacement in unstable fractures, the evidence-based studies have not yet demonstrated that intramedullary devices are better than plates and screws regarding blood loss, complications, functional recovery and the rate of another surgery [4-6]. Adams et al. conducted a perspective randomized controlled study in a total of 400 cases to compare the intramedullary nail with DHS plate regarding the effectiveness [4]. The rates of need for another fixation, fracture of femoral shaft and lag screw cutting were higher in the intramedullary nailing group compared to the DHS group, despite of no significant difference. There were no significant differences in early-stage and 1-year functions between two groups. Papasimos et al. designed a perspective randomized study in 120 cases with unstable intertrochanteric fracture to compare SHS, Gamma nails with PFN and found there were no significant differences in average blood loss, hospital stay, screw cutting and reduction of fracture among three groups [5]. But the PFN group had longer operative time (P<0.05), possibly due to operator's insufficient experience in PFN. Liu et al. also demonstrated Gamma nail was not significantly better than DHS for the treatment of FIF [6]. For the unstable crushed FIF, the compressive stress could not pass through the calcar femorale cortex due to defect in calcar femorale. The application of DHS to fix the lateral cortex may cause higher incidences of complications such as loosening of screws, screw cutting, collapse of plate, nonunion or malunion because the tensile stress and comprehensive stress are centered on the plate for a long time to increase the stress on internal implant. Haidukewych et al. reported that angle stabilizer resulted in better outcomes and less complications when compared with DHS, since it provided stronger anti-rotation and prevented excess lateral sliding, thus seldom causing later lateral wall fracture [20]. The “LISS” system was developed by the AO group for treatment of distal femoral fracture. The plate is an angle stabilizer designated based on anatomy of distal femur. Some reports demonstrated the feasibility of reverse LISS in the treatment of proximal femoral fracture [9-13]. Lewis et al. reported LISS could lower surgery-related complications administered shorten operative time when it was performed for proximal femoral fracture [10]. Gao et al. suggested that LISS might be an alternate for people with unstable hip fractures but not candidates for intramedullary nailing [12]. Yao et al. treated FIF 56 cases with LISS or PFN and found there were no significant differences in operative time and intraoperative blood loss, but the LISS group had lower hemochrome [9]. They proposed that LISS was a better choice to provide quick fixation and control of the injury for patients with multiple traumas and also to perform open reduction and internal fixation for those with subtrochanteric fractures and reverse trochanter, although it was not recommended as routine option for unstable elderly FIF. Ma et al. reported that reverse LISS for 22 cases with unstable proximal femoral fractures achieved 100% healing rate and low incidence of complications [13]. Malunion and infection were not observed in 22 FIF cases treated with reverse LISS in this study.
For unstable FIF fractures, the nailing site for DHS and PFNA is located at fracture line, which makes it hard to select nailing site and also causes instability of nail or plate when it passes through the fracture line to femoral neck, more likely to cause complications such as collapse of plate and screw, loosening screw, femur cutting, another fracture and hip varus. If femoral subtrochanteric fractures affect sinus piriformis, or if patients have poor reduction by closed traction, or free trochanteric bone blocks, ruptured coronal plane, narrowed femoral marrow cavity, big femoral anterior arch, or severe femoral deformity, there can be difficulties in use of intramedullary nail, especially if the patient is obese. In these cases, reverse femoral LISS is optimum choice [21]. It is characterized by minimal invasion, easy operation, reliable fixation, high safety and fewer complications [21].
Features of LISS and precautions during operation
First, the LISS plate and screw can be fixed in different angles through the screw thread. The locking of plate and screw forms a frame structure to lower the incidence of screw penetration out of the femoral head and prevent loosening of screw. In osteoporotic and comminuted fractures, screws have better binding force and anti-tensile strength. Second, there is no contact and pressure between the plate and the bone, and it avoids compression of the plate on periosteum, maintains the blood supply to the bone, which is helpful for fracture healing. Third, the screw for LISS plate can be placed percutaneously and the locking of LISS plate and screw can be performed percutaneously without exposure of the fracture site, which supports the concept of BO technology. The LISS is easy to use and requires short operative time, and avoids extensive exposure. There is also no need for reconstruction. Fourth, at least 4 screws can be inserted on the LISS plate since it has multiple pores on the proximal end. This substantially enhances anti-rotation of femoral neck and improves stability of fracture after fixation. Fifth, Lateral placement of LISS can reduce tension of iliopsoas and adductor, which benefits natural reduction of posterointernal fracture fragments and reduce stress on proximal screw [22]. Sixth, the LISS plate has no effect on reduction of fractures. Therefore, reduction should be performed and maintained before placement of screw. The preliminary reduction is first performed, which includes recovery of normal length and axis, and adjustment of rotation. Seventh, the first guidewire inserted through Hole A is very important. It must be located at 1/3rd below the femoral neck on the anteriorposterior view and in the center of the femoral neck on the lateral view [19].
Disadvantages of reverse LISS for FIF
First, the femoral condylus lateralis has similar structure to femoral greater trochanter, so LISS plate is more attached to lateral cortex of femoral greater trochanter. However, the width of plate head is greater than that of greater trochanter in some patients, especially in thin women, which can cause pain and then cause trochanteric synovitis. In this present study, there were 2 cases who felt uncomfortable in greater trochanter following surgery. Such discomfort was relieved after removal of the implant. Second, the arch of femur should also be taken into account when the reverse LISS plate is used for FIF. The plate may not match with the femur and may be appropriately preflexed during surgery [23]. Third, reverse LISS is an angle stabilizer. Not like sliding hip screw and intramedullary nail, it does not provide sliding and pressure on fracture fragments.
When the calcar femorale is not adequately supported, varus union or rupture of implant may occur in case of weight bearing. This is particularly so for osteoporotic unstable fractures. Acklin et al. reported the incidence of complications was 16%, including 1 case with screw rupture [24]. In this study, plate rupture and varus malunion of fracture were found in 1 case, caused by poor adherence after surgery such as out-of- bed activities and weight bearing 2 months after surgery.
The limitations of this study are mainly as follows: 1) The sample size was small, which may have influenced the final results of this study. 2) This is only a retrospective study. Large, double-blind, and random perspective trials are needed to verify the results of Reverse LISS plate in treating femoral intertrochanteric fractures.
Conclusions
We concluded that reverse LISS is effective for the treatment of FIF. There may be difficulties in application of intramedullary nailing. It has its own advantages in spite of some unsuccessful cases. To improve the clinical outcomes, the procedures must be standardized and early weight bearing must be prevented following surgery.
Acknowledgment
This study was supported by Yiwu Science and Technology Plan Projects (11-3-03).
References
- Bohl DD, Basques BA, Golinvaux NS, Miller CP, Baumgaertner MR, Grauer JN. Extramedullary compared with intramedullary implants for intertrochanteric hip fractures: thirty-day outcomes of 4432 procedures from the ACS NSQIP database. J Bone Joint Surg Am 2014; 96: 1871-1877.
- Cheng Q, Huang W, Gong X, Wang C, Liang X, Hu N. Minimally invasive percutaneous compression plating versus dynamic hip screw for intertrochanteric fractures: a randomized control trial. Chin J Traumatol 2014; 17: 249-255.
- Lopez-Vega M, Gil-Monzo ER, Rodrigo-Perez JL, Lopez-Valenciano J, Salanova-Paris RH, Peralta-Nieto J, Morales-Suarez MM. Randomized prospective study on the influence distal block and Gamma 3 nail on the treatment of intertrochanteric fractures of femur. Rev Esp Cir Ortop Traumatol 2015; 59: 26-35.
- Adams CI, Robinson CM, Court-Brown CM, McQueen MM. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma 2001; 15: 394-400.
- Papasimos S, Koutsojannis CM, Panagopoulos A, Megas P, Lambiris E. A randomised comparison of AMBI, TGN and PFN for treatment of unstable trochanteric fractures. Arch Orthop Trauma Surg 2005; 125: 462-468.
- Liu M, Yang Z, Pei F, Huang F, Chen S. A meta-analysis of the Gamma nail and dynamic hip screw in treating peritrochanteric fractures. Int Orthop 2010; 34: 323-328.
- Sahin EK, Imerci A, Kinik H, Karapinar L, Canbek U, Savran A. Comparison of Proximal Femoral Nail Antirotation (PFNA) with AO Dynamic Condylar Screws (DCS) for the treatment for unstable peritrochanteric femoral fractures. Eur J Orthop Surg Traumatol 2014; 24: 347-352.
- Simmermacher RK, Ljungqvist J, Bail H, Hockertz T, Vochteloo AJ. The new Proximal Femoral Nail Antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury 2008; 39: 932-939.
- Yao C, Zhang CQ, Jin DX, Chen YF. Early results of reverse less invasive stabilization system plating in treating elderly intertrochanteric fractures: a prospective study compared to proximal femoral nail. Chin Med J (Engl) 2011; 124: 2150-2157.
- Pryce Lewis JR, Ashcroft GP. Reverse LISS plating for proximal segmental femoral fractures in the polytrauma patient: a case report. Injury 2007; 38: 235-239.
- Li Y, Chen Y, Liu X, Liang Y, Shao X, Zhang Y, Wang H, Wang X, Li B, Deng K, Liu Q, Holthofer H, Liu H, Zou H. Metabolic syndrome and chronic kidney disease in a Southern Chinese population. Nephrology (Carlton) 2014; 19: 325-331.
- Gao K, Gao W, Li F, Tao J, Huang J. Treatment of ipsilateral concomitant fractures of proximal extra capsular and distal femur. Injury 2011; 42: 675-681.
- Ma CH, Tu YK, Yu SW, Yen CY, Yeh JH, Wu CH. Reverse LISS plates for unstable proximal femoral fractures. Injury 2010; 41: 827-833.
- Jensen JS, Michaelsen M. Trochanteric femoral fractures treated with McLaughlin osteosynthesis. Acta Orthop Scand 1975; 46: 795-803.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51: 737-755.
- Kokoroghiannis C, Aktselis I, Deligeorgis A, Fragkomichalos E, Papadimas D. Evolving concepts of stability and intramedullary fixation of intertrochanteric fractures-a review. Injury 2012; 43: 686-693.
- Aktselis I, Papadimas D, Fragkomichalos E, Deligeorgis A, Kokoroghiannis C. Intramedullary nailing of trochanteric fractures-operative technical tips. Injury 2012; 43: 961-965.
- Darrigo C, Carcangiu A, Perugia D, Scapellato S, Alonzo R, Frontini S, Ferretti A. Intertrochanteric fractures: comparison between two different locking nails. Int Orthop 2012; 36: 2545-2551.
- Kakkar R, Kumar S, Singh AK. Cephalomedullary nailing for proximal femoral fractures. Int Orthop 2005; 29: 21-24.
- Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am 2001; 83: 643-650.
- Zhou F, Zhang ZS, Yang H, Tian Y, Ji HQ, Guo Y, Lv Y. Less invasive stabilization system (LISS) versus Proximal Femoral Nail Anti-Rotation (PFNA) in treating proximal femoral fractures: a prospective randomized study. J Orthop Trauma 2012; 26: 155-162.
- Ouyang Y, Wang Y, Fan C, Liu Z, Liu S, Li F. Using the contralateral reverse less invasive plating system for subtrochanteric femur fractures in elderly patients. Med Princ Pract 2012; 21: 334-339.
- Jaiman A, Neogi DS. Comment on minimally invasive management of unstable proximal femoral extracapsular fractures using reverse LISS femoral locking plates. Hip Int 2011; 21: 507-507.
- Acklin YP, Bereiter H, Sommer C. Reversed LISS-DF in selected cases of complex proximal femur fractures. Injury 2010; 41: 427-429.