Case Report - Biomedical Research (2017) Volume 28, Issue 14
Re-opening of Eustachain tube atrisia after radiotherapy in nasopharyngeal carcinoma: Two case reports
Huagong Gao, Ding Li, Jun Tong, Wenwen Chen*, Lijun Du and Liang Shan
Department of Otorhinolaryngology, Divided Hospital of Shanghai University Communication Affiliated First People Hospital, Shanghai, PR China
- *Corresponding Author:
- Wenwen Chen
Department of Otorhinolaryngology
Divided Hospital of Shanghai University, PR China
Accepted date: April 29, 2017
Abstract
Nasopharyngeal Carcinoma (NPC) is a highly happening disease. Eustachain tube atrisia after radiotherapy is easy to occur in NPC patients. This study presented 2 cases of re-opening of Eustschian tube atresia after radiotherapy for NPC patients. Two female cases (62 and 64 y old; receiving postradiothapy 6 and 20 y ago, respectively) were diagnosed with Eustachian tube pharyngeal orifice atrisia. The Eustachain tube atrisia was re-opened by laser. A plastic cum cone-shape top tube was inserted and pulled and pushed repeatedly for about 6 months. The patients were followed up over 12 months. After treatment, the opened roundness pharyngeal orifice was formed. The Valsava’s air-blowing was easy. All two cases had no reduced pharyngeal orifice in follow up, and they had no yet abnormal patency of Eustachian tube. The Eustachain tube atrisia after radiotherapy can be cured by using laser and inserting plastic cum cone-shape top tube with pulling and pushing repeatedly.
Keywords
Eustachian tube, Atresia, Nasopharyngeal carcinoma, Radiotherapy
Introduction
Nasopharyngeal Carcinoma (NPC) is a high happen diseases in south China. Radiotherapy is the first choice for NPC. In many NPC patients, the Eustachain tube atrisia is easy to occur after radiotherapy. The morbidity of this lesion is high as 35-75% [1]. Eustachain tube atrisia is the primary cause for hearing loss in NPC patients after radiotherapy. It has a relationship inextricably interwoven with loss function of Eustachain tube, and is a result of radiotherapy harm [2]. The common Eustachain tube atrisia can be remitted by puncture drum or a tube insert drum. However, it is more severe after radiotherapy, and the Eustachain tube is often closed by adhesion or scar at pharyngeal orifice or luminal cartilage segment [3]. In addition, the meddle ear has secondary changes such as tympanic cavity adhesiveor, choresteatoma, etc.. Furthermore, the atrisia of Eustachain tube is very difficult to relieve. Until now there is no report on the cases with successful re-opening of Eustachain tube atrisia. In this study, we firstly presented 2 cases of re-opening of Eustachain tube atrisia after radiotherapy in NPC. The objective was to provide a reference for the treatment of Eustachain tube atrisia after radiotherapy in NPC.
Case Report
Case 1
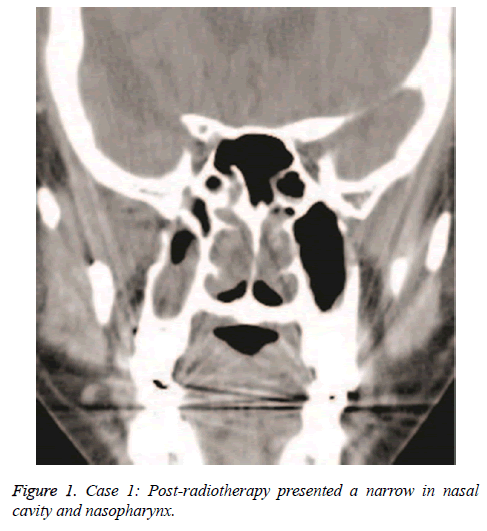
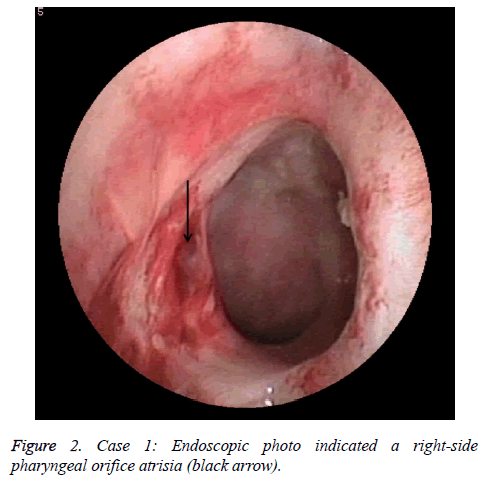
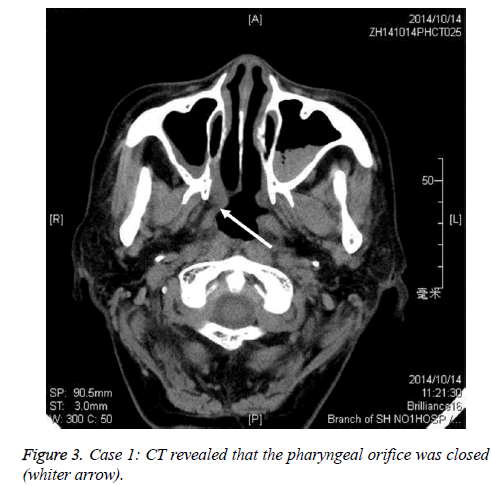
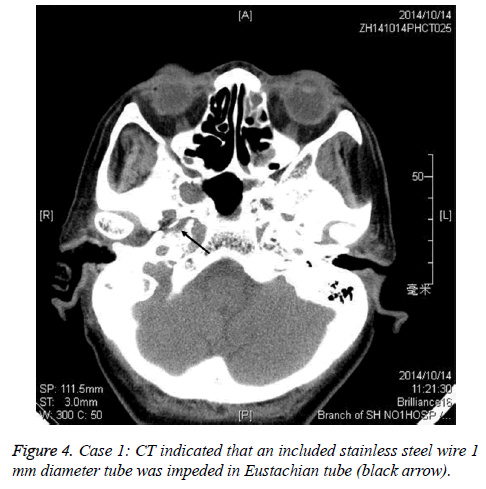
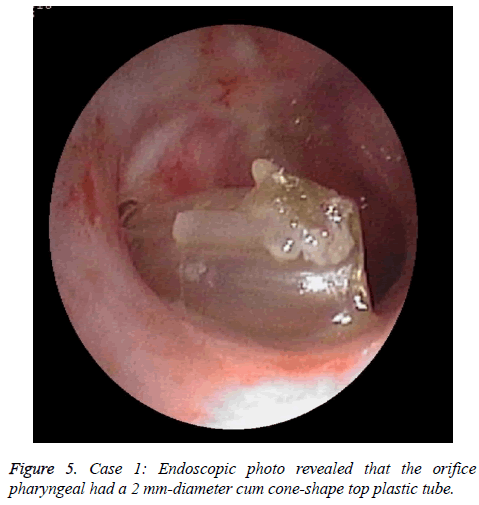
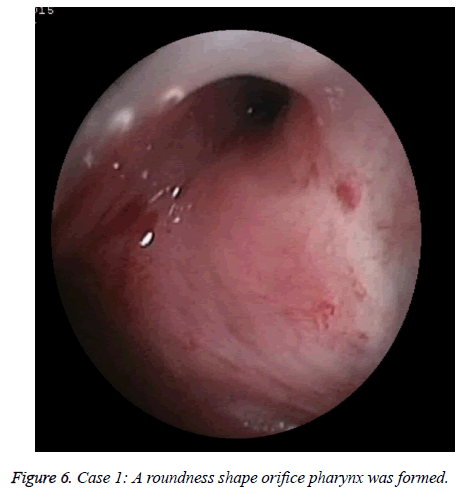
A female NPC patient with 65 y old received radiotherapy 6 y ago. She suffered from an atrisia in nasal cavity and nasopharyngeal. The CT finding was shown in Figure 1. The Eustachain tube pharyngeal orifice also had an atrisia. The endoscopic photo finding was in shown in Figure 2, and the CT finding was in Figure 3. When inserting an included stainless steel wire plastics tube with 1 mm diameter from ostium tympanicum, it was impeded about 10 mm separate orifice of pharynx. The CT finding was in shown in Figure 4. The atrisia orifice pharynx was re-opened by diode laser. A 1 mm diameter plastics tube was inserted to keep open about 6 months. A 2 mm-diameter plastics tube including a cone-shape head end was inserted to replace the 1 mm tube and was activated back and forth repeatedly. The endoscopic photo finding was in shown in Figure 5. The tube was pulled out after about 6 months, and finally a roundness shape orifice pharynx was formed. The endoscopic photo finding was in shown in Figure 6. The Valsava’s air-blowing was very easy. The tympani member perforation was closed up after 1 month by itself. The hearing was improved compared with before treatment. The patient was followed up over one year, and the outcome was maintained good.
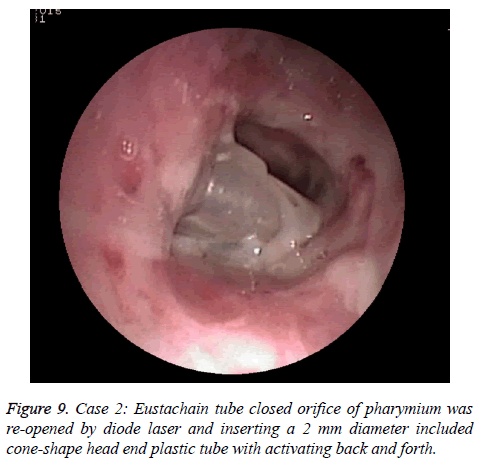
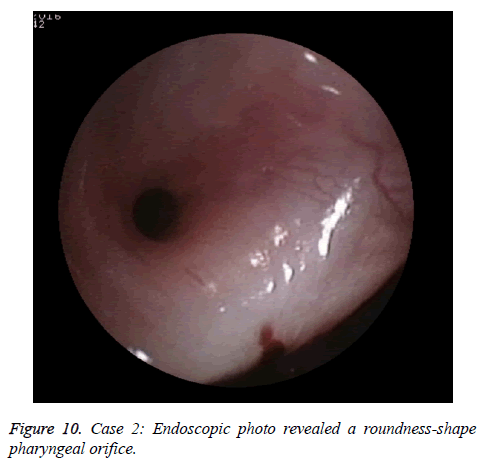
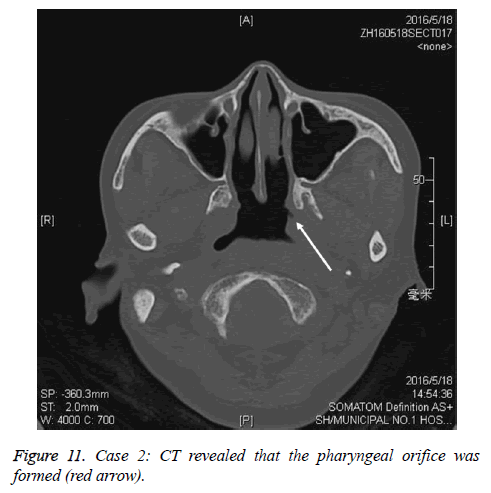
Case 2
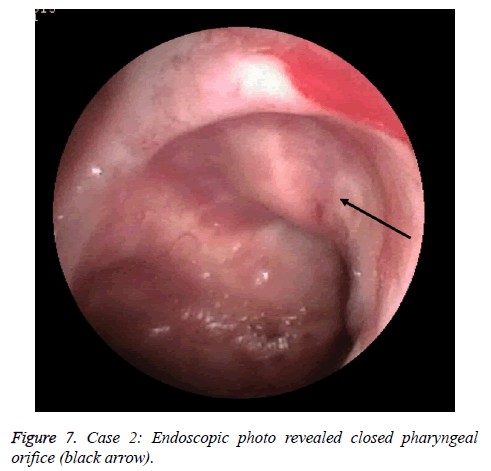
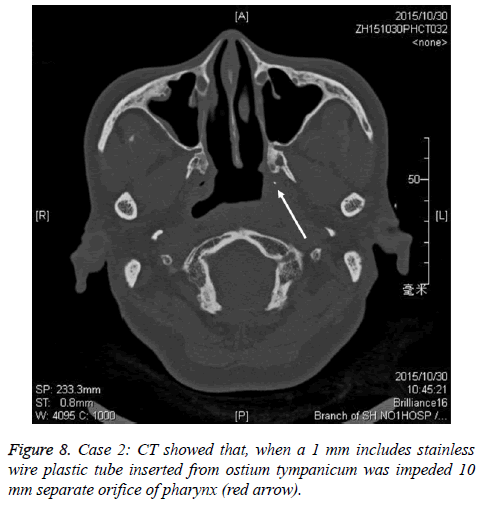
A female patient with 64 y old received the radiotherapy over 20 y for nasopharynic cancer. She had left orifice pharynx atrisia and soft palate paralysis. The endoscopic photo finding was in shown in Figure 7. The pharyngeal orifice was closed when a 1 mm include stainless wire plastic tube was inserted from ostium tympanicum to impede 10 mm separate orifice of pharynx. The CT finding was shown in shown in Figure 8. The Eustachain tube pharyngeal orifice atrisia was re-opened by diode laser and inserting a 2 mm diameter included a coneshape head end plastic tube and activating back and forth. The endoscopic photo finding was showed in Figure 9. The tube was pulled out after about 6 months, and a roundness shape orifice pharynx was formed. The endoscopic photo finding was showed in Figure 10. The CT finding was shown in Figure 11. The Valsava’s air-blowing was very easy too.
Discussion
The orifice pharynx atrisia after radiotherapy for nasopharyngeal cancer is a common condition. However, it has not treatment experience for past very long time because of lacking valid methods.
This study may be first report for re-opening of pharyngeal orifice atrisia after radiotherapy in whole world as we are aware.
We had reported a case of pharyngeal orifice seal off since 8 y before [4]. In that case, the orifice pharynx atrisia was after operation of nasal endoscopy.
The closed orifice was re-opened by a diode laser, and 1 mm plastic tube and a titanic stent were inserted. The orifice presented a small hole after 6 months.
The secret could discharge from tympani to pharynx when airball compress in ear canal, but Valsava’s air-blowing could not. Apparently, this result was not satisfactory.
Now we used a cum cone-shape top plastic tube pulling and pushing repeatedly for dilating the pharyngeal orifice. It made the mucous member and submucous together, and overturn into tube. The orifice was formed with a roundness hole and had not narrowed again. The two cases could perform the Valsava’s air-blowing, which was a gold index for Eustachian tube unblocked. Recently, Kivekas et al. [5] report the histopathology of balloon-dilation Eustachian tube, which can make mucus member inflammatory reaction and swelling altered. Therefore, the dysfunction Eustachian tube was improved. Our cases are based on the same mechanism for gaining re-opened pharyngeal orifice.
In this study, both two cases had no “patulous” or abnormal patency Eustachian tube. Recently, Aper et al. [6] report quantitative description of Eustachian tube movement during swallowing as visualized by transnasal videoendoscopy. This perhaps had some revelation. When Eustachian tube is opened, the torus happen medial rotation and soft palate elevation close the pharynx airway. Similarly, in respiration, the Eustachian tube is closed. As long as ruling Eusthian tube and several muscles coordinate, the tube open or respiration cannot happen at the same time. This physiologic mechanism can ensure no occurrence of “patulous”. Dennis et al. [7] have reported balloon dilation of the cartilaginous Eustachian tube. No “patulous” happens in their cases. Of course, the “patulous” perhaps has more complicated cause, so more studies are needed.
References
- Zhou Y, Tang AZ. Nasopharyngeal carcinoma was radiotherapy complication and prevention. Practical NPC clinic diagnose and treatment. Beijing Sci Publ Comp 2010; 205.
- Wang SZ, Chen ZC, McNamar JP, Wang SY, Cheng QF. The relationship between the protective effect of amifostine and decreased intercellular adhesion molecule 1 expression. Am J Otolaryngol 2005; 26: 118-122.
- Zhou Y, Tang AZ, Li J. The Eustachian tube dysfunction types after radiotherapy for nasopharyngeal carcinoma. Clinic Otorhinolaryngol 2003; 17: 464-465.
- Chen WW, Tong J, Deng YX. Laser eustanchian tubeplasty and titanic-nickel stent insert for atresia: a case report. Chin J Otorhinolaryng Head Neck Surg 2008; 43: 860-861.
- Kivekas I, Chao WC, Faquin W, Hollowell M, Silvola J, Rasooly T, Poe D. Histopathology of balloon-dilation Eustachian tuboplasty. Laryngoscope 2015; 125: 436-441.
- Alper CM, Teixeira MS, Swarts JD, Doyle WJ. Quantitative description of eustachian tube movements during swallowing as visualized by transnasal videoendoscopy. JAMA Otolaryngol Head Neck Surg 2015; 141: 160-168.
- Dennis SP, Juha S, Llmari P. Balloon dilation of the cartilaginous eustachian tube. Otolaryng Head Neck 2011; 144: 563-569.