Research Article - Biomedical Research (2017) Volume 28, Issue 19
Quantitative three-dimensional assessment of buccal alveolar bone thickness with dental cone-beam computed tomography
Salmeh Kalbassi1*, Foong Weng Chiong2, Hwang Yee Cheau3 and Wong Hung Chew4
1Orthodontist in Private Practice, Iran (Tehran), Oman, UAE
2Associate Professor, Department of Preventive Dentistry, National University of Singapore, Singapore, Singapore
3Senior Consultant, Department of Preventive Dentistry, National University of Singapore, Singapore, Singapore
4Senior Biostatistican, Biostatistics Unit, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Accepted date: August 03, 2017
Abstract
Objectives: The purpose of this study was to develop a procedure for quantifying the buccal alveolar bone thickness surrounding each tooth prior to orthodontic treatment in 3D, using CBCT.
Methods: This retrospective cross-sectional study was carried out on 18 Singaporean Chinese patients. A total of 18 CBCT scans met the inclusion criteria, resulting in a sample size of 85 teeth, using two kinds of CBCT scanners. All CBCT data were stored in DICOM format. Buccal Alveolar bone thickness was measured after defining the boundaries of each individual tooth and surrounding alveolar bone using Kruskal-Wallis, Mann-Whitney U-test, and linear regression for statistical analysis.
Results: There was statistical significant difference in buccal bone thickness between incisor versus premolar, incisor versus molar, canine versus premolar, Canine and premolar versus molar. However, the difference between incisors and canines and between central and lateral incisors was not significant. There was also no statistical significant difference in the buccal bone thickness between maxillary and mandibular incisors, between maxillary and mandibular central incisors, and between maxillary and mandibular lateral incisors, neither between maxillary and mandibular canines.
Conclusions: The thickness of buccal bone is lowest in the incisor and canine reigns with no statistically significant difference between canines and incisors. The thickness of the alveolar bone in premolar region is significantly greater than incisor and canine regions but lesser than molar region. No statistically significant differences were found regarding buccal bone thickness between maxillary and mandibular incisors and canines.
Keywords
Cone-beam computed tomography (CBCT), Alveolar process, Orthodontics
Introduction
Orthodontic diagnosis requires a thorough examination of the supporting periodontium [1]. Bone volume and bone thickness as well as dehiscences, fenestrations, and other intra-bony defects should be included for the orthodontic diagnosis and treatment plans [2]. The thickness of the alveolar bone defines the boundaries of the orthodontic movement and taxing these limits may cause undesirable effects on the periodontal tissues. The most critical orthodontic movement includes dental arch expansion and buccal-lingual movement of maxillary and mandibular incisors [3-5]. Such mechanics can move the teeth away from the alveolar bone envelope, causing bone dehiscences, fenestrations, and gingival recession, depending on the pre-treatment amount (depth and height) and morphology of the alveolar bone relative to tooth root dimensions, angulation, and spatial position, as well as on the amount of tooth movement [3,5].
Mini-implants have gained considerable popularity due to their low cost, effectiveness, clinical management, and stability [6,7]. Lee et al. conducted a study to quantify the buccal bone thickness and peri-radicular space in the tooth-bearing area to provide practical guidelines for mini-implant placement using Cone-Beam Computed Tomography (CBCT) [8]. Among the factors related to mini-implant stability, bone density and cortical bone thickness appear to be critical for successful placement. Thin cortical bone has been reported to be a possible cause for failure of orthodontic mini-implants [9-11]. Moreover, bone thickness is thought to be a major factor for stability because primary retention is achieved by mechanical interdigitation rather than bone to mini-implant contact at an early stage of healing [11-13]. Therefore, support from cortical bone is essential for initial stability of mini-implants [14,15].
Identifying dehiscences before treatment is of paramount importance due to its effects on treatment plan decision. However, this requires a surgical flap procedure or a Computed Tomography (CT) image. Significant risks from flap surgery are possible including recession, soft tissue dehiscence, and tissue necrosis [16,17]. CT’s had a very high dose of radiation, incurring large expense to the practitioner as well as patient, and is not practical for dentistry [18]. A newer technology CBCT has the potential to identify these periodontal defects without most of the cost and radiation issues associated with CTs [19,20].
Despite many reports in the literature on the various uses of CBCT, studies on its accuracy and image quality for assessing bone morphology have been limited. Instead, most studies used radiographic phantoms, which do not accurately represent some anatomic structures such as tooth sockets and alveolar bone margins [21,22]. Other studies have used human dry skulls for this purpose [19,20,23]. Vandenberghe et al. investigated periodontal bone architecture using conventional intraoral radiography and three-dimensional (3D) CBCT images. The conclusions of this study were that traditional radiography images provided more bone details, but CBCT provided a better morphologic description of the alveolus and periodontal defects. Intraoral radiography scored significantly better for contrast, bone quality, and delineation of lamina dura, while CBCT was superior for assessing crater defects and furcation involvements [24]. In a follow up study, CBCT scans with 0.4 mm thick cross-sections demonstrated more accurate values, indicating enhanced assessment of periodontal bone loss [25]. CBCT’s offer tooth and bone assessment without obstruction from overlying structures [26]. They also have a reduced radiation dosage and cost compared to CT [19,27].
The aim of this study was to develop a methodology for quantifying alveolar bone thickness in 3D. Furthermore, evaluation of the buccal alveolar bone thickness of each tooth type was conducted prior to orthodontic treatment through CBCT. Since the alveolar bone boundaries may limit or dictate the potential tooth movement, this study is crucial because the identification of alveolar bone thickness before orthodontic treatment is instrumental for the clinician to make more precise diagnosis and treatment plans. We hypnotized that prior to orthodontic tooth movement all teeth housed within the alveolar trough have complete bone cover of the teeth roots on the buccal side.
Materials and Methods
Sample and data acquisition
This retrospective cross-sectional study was carried out on 18 Singaporean-Chinese patients (10 males and 8 females) with age ranges from 11 to 45 y. CBCT scans were taken at our medical center prior to orthodontic treatment. A total of 18 CBCT scans met the inclusion criteria, resulting in a sample size of 85 permanent teeth. Two kinds of CBCT scanners were used in this experiment: (1) 3D exam 2nd Generation, KaVo, Biberach, Germany; (2) Pax-Reve3D, Vatech, Canonsburg, PA, USA. All CT data saved as digital imaging and communications in medicine (DICOM) files.
Measurement procedures
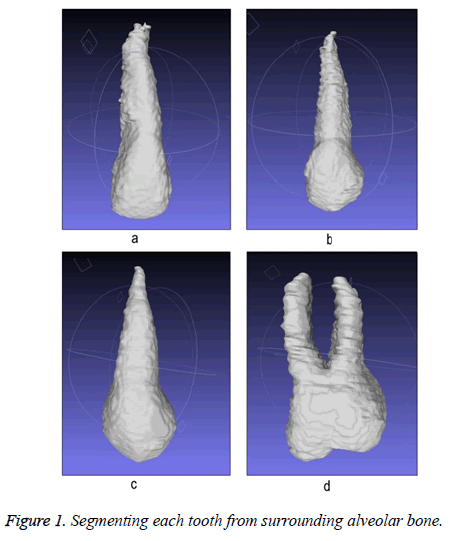
Step 1: Segment each tooth from surrounding alveolar bone (our region of interest) in axial plane by cutting from mesiodistal edges of crown parallel to the long axis of the tooth (Figure 1).
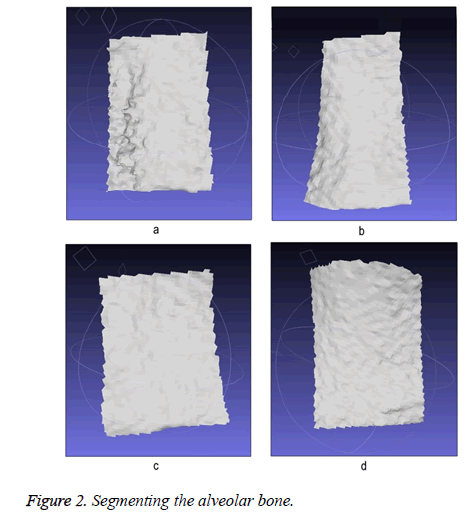
Step 2: Segment the alveolar bone from the alveolar crest to the tooth apex (Figure 2), which is already gotten in step 1. Define the surface of the tooth as “ST”. Define the surface of the alveolar bone as “SA”.
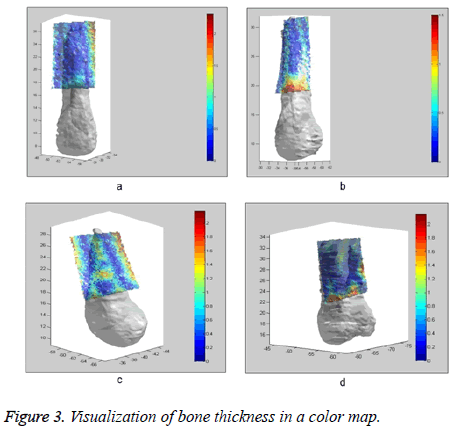
Step 3: Find the iso-surface points of two surfaces “ST” and “SA”. For each point sampled from “SA”, we can find the corresponding nearest neighbour point in surface “ST”, which can serve as the distance from that point of alveolar bone to the corresponding point of the tooth. These distances are the alveolar bone thickness.
Step 4: Visualize these distances (buccal bone thickness) in a color map (Figure 3).
For a meaningful comparison of the bone thickness measurements, we continued to make: (i) intra-arch comparisons of bone thickness measurements between teeth type, i.e., incisors vs. canines, and so forth for each tooth type (incisors vs. canine’s vs. premolars vs. molars) within each arch; (ii) inter-arch comparisons of incisors and canines. We did not compare left vs. right sides, as this comparison is not clinically meaningful.
Statistical analysis
Kruskal-Wallis test has been used to evaluate whether there are any differences in the buccal bone thickness among the type of tooth. Mann-Whitney U test has been further carried out to evaluate the pairwise differences. Mann-Whitney U test is a nonparametric test of the null hypothesis that it is equally likely that a randomly selected value from one sample will be less than or greater than a randomly selected value from a second sample. Kruskal-Wallis test is a non-parametric method for testing whether samples originate from the same distribution. It is used for comparing two or more independent samples of equal or different sample sizes. Kruskal-Wallis test extends the Mann-Whitney U test when there are more than two groups.
Linear regression has been used to assess whether there are any differences in the buccal bone thickness among the type of tooth in order to account for the effect of the site (maxilla/ mandible). To evaluate the differences in the number of points that is less than 0.l mm among the type of tooth, negative binomial regression has been utilized with and without accounting for the effect of the site (maxilla/mandible). Mann- Whitney U test has also been carried out to assess the differences in the buccal bone thickness between: 1) Lateral and central incisors; 2) Mandibular and maxillary incisors; 3) Mandibular and maxillary central incisors; 4) Mandibular and maxillary lateral incisors; 5) between mandibular and maxillary canines. For any multiple pairwise comparisons, Bonferroni correction technique has been applied. The Bonferroni correction is one of several methods used to counteract the problem of multiple comparisons. For all analyses, statistically significant level was set at 0.5. All the analyses performed using Statistical Package for the Social Sciences (SPSS) software (SPSS Inc., Version 19 and Chicago, IL).
Results
Since the buccal bone thickness was irregularly excessive in one of the molar specimens (18.02 mm), it was excluded from the statistical analysis. Descriptive statistics are presented in Tables 1 and 2. The Kruskal Wallis test showed that there was a significant difference between the teeth type (p<0.05). Pairwise comparisons using the Mann-Whitney U test showed significant differences between incisors versus premolars (p<0.001), incisors versus molars (p<0.001), canines versus premolars (p=0.001), canines versus molars (p<0.001), and premolars versus molars (p=0.042). However, there were no significant difference between incisors and canines (p=1.0) and between central and lateral incisors (p=0.635).
| Tooth type | Number | Median | Minimum | Maximum |
|---|---|---|---|---|
| Incisor | 32 | 0.89 | 0.24 | 3.67 |
| Central incisor | 18 | 0.89 | 0.38 | 1.91 |
| Lateral incisor | 14 | 0.81 | 0.24 | 3.67 |
| Canine | 13 | 0.82 | 0.42 | 1.9 |
| Premolar | 24 | 2.04 | 0.31 | 5.57 |
| Molar | 16 | 3.55 | 1.6 | 12.72 |
Table 1. Descriptive statistics for buccal bone thicknesses.
| Tooth type | Number | Median | Minimum | Maximum |
|---|---|---|---|---|
| Maxilla | ||||
| Incisors | 25 | 0.89 | 0.24 | 3.67 |
| Central incisor | 14 | 0.89 | 0.38 | 1.91 |
| Lateral incisor | 11 | 0.97 | 0.24 | 3.67 |
| Canine | 11 | 0.66 | 0.42 | 1.25 |
| Premolar | 18 | 1.94 | 0.31 | 5.57 |
| Molar | 13 | 2.78 | 1.6 | 12.72 |
| Mandible | ||||
| Incisors | 7 | 0.89 | 0.48 | 1.85 |
| Central incisor | 4 | 0.95 | 0.82 | 1.85 |
| Lateral incisor | 3 | 0.52 | 0.48 | 1.1 |
| Canine | 2 | 1.08 | 0.91 | 1.25 |
| Premolar | 6 | 2.12 | 1.38 | 4.04 |
| Molar | 3 | 6.15 | 3.21 | 8.61 |
Table 2. Descriptive statistics for buccal bone thicknesses in maxilla and mandible.
Linear regression showed that while there were statistical significant differences in the buccal bone thickness among the type of the tooth (p<0.001) even after accounting for the effect of the site (mandible/maxilla). It was found that there were significant differences in the buccal bone thickness between incisors and molars (p<0.001), between canines and molars (p<0.001), and between premolars and molars (p<0.001). It was also found that there was statistical significant difference in the number of points that is less than 0.l mm among the type of tooth with and without accounting for the effect of the site (mandible/maxilla). Incisor and canine were found to have higher number of points that is less than 0.1 mm compared with premolar, respectively (Univariate test: incisor versus premolar: relative risk (RR) (95% Confidence Interval)=18.76 (3.05 to 115.28), canine versus premolar: (RR) (95% Confidence Interval)=36.01 (3.59 to 361.22); Multivariate: incisor versus premolar: Adjusted RR (95% Confidence Interval)=13.49 (1.96 to 92.75), canine versus premolar: Adjusted RR (95% Confidence Interval)=30.92 (3.09 to 309.27). However, cautious has to be practiced in the interpretation of the results since the confidence interval is wide.
There were no statistical significant differences in the buccal bone thickness between maxillary and mandibular incisors (p=0.945), between maxillary and mandibular central incisors (p=0.366), and between lateral incisors (p=0.815). In addition, no statistical significant difference was found in the buccal bone thickness between the upper and lower canines (p=0.323).
Discussion
Understanding the alveolar bone morphology using the images derived from a CBCT has been of great interest in the dental community and comparing CBCT images to traditional.
Intraoral radiography, it was found that CBCT had better potential to represent the alveolus, especially detecting the 3D volume of intrabony defects. CT permits the dental professional to visualize what the conventional radiographs never showed the thickness and level of the labial/buccal and lingual alveolar bone.
Previously to the introduction of CT, the visualization of the labial/buccal and lingual bone plates was not possible due to image superimposition of conventional radiographs and due to gingival covering in clinical analysis [24,25]. The detection of dehiscences through traditional radiography or direct evaluation is nearly impossible.
However, due to the high definition and sensitivity, helical and CBCT images can show bone dehiscences and fenestrations [3,26,28-30]. Before the introduction of CT, efforts to define tooth movement effects on the buccal and lingual bone plates were concentrated on animal experiments, and on studies with conventional radiographs [31-33]. Currently, there are few CT studies on the alveolar bone morphology before orthodontic treatment [30-32]. However, their measurement limited to mandibular cortical bone, mandibular central incisors or maxillary incisors [30-32]. A few CT studies are also available on the consequences of tooth movement on the alveolar bone [34-37].
In 2008, a high accuracy of CBCT for quantitative analyses of the level of buccal and lingual bone plates was demonstrated [21,30]. The results of our study showed that buccal/labial bone thickness can be accurately measured pre-orthodontics using CBCT. For a meaningful comparison of the bone thickness measurements, we have made intra-arch comparisons of bone thickness measurements between teeth type, i.e. incisors vs. canines vs. premolars vs. molars. The results of present study indicated that the thickness of buccal bone is lowest in the incisor and canine regions with no statistically significant difference between canine and incisor groups, which can be explained by the greater volume of the permanent canine’s root. The thickness of the alveolar bone in premolar region is significantly greater than incisors and canine region but lesser than molar region thus the thickest buccal bone is associated with molar area.
Studies on animals showed that the labial movement of the incisors, even using light forces, produces an increase in the distance between buccal alveolar crest and Cement-Enamel Junction (CEJ) [31,32]. Interestingly, studies conducted on human maxillary bones extracted during autopsy presented similar conclusions [38,39]. Based on our survey this can be due to the thin buccal bone at the incisor region.
In the permanent dentition, both the maxillary rapid expansion, and the slow maxillary expansion, might cause buccal bone dehiscences in the posterior teeth, mainly in patients with an initial thin buccal bone plate [28,34,40]. Maxillary first premolars showed more critical bone dehiscences than the first molars during RME, which also can be explained by the results of present study due to the thinner buccal bone at premolar region compare to molar area [34].
Lee et al. performed a study to quantify the buccal bone thickness and peri-radicular space in the tooth-bearing area to provide practical guidelines for mini-implant placement [8]. CTs of 30 maxillae and mandibles were taken from nonorthodontic Korean adults with normal occlusion. Both mesiodistal inter-radicular distance and buccal bone thickness over the narrowest inter-radicular space (safety depth) were measured at 2, 4, 6, and 8 mm from the CEJ, respectively. Their result showed that the overall bone thickness overlying the buccal surface of each root was greater in the posterior area compared with the anterior region, which is in agreement to our finding. They found that mean thickness of the incisors and the first premolar was less than 1 mm, even at 8 mm level, in both the maxilla and the mandible. However, in our study, the mean thickness for incisors and canines was less than 1mm but for premolar mean thickness was more than 2 mm. In addition, they used medical CT in their study which has its own limitation compare to CBCT due to high cost and high radiation dose. They have also done measurements of bone thickness at only 4 vertical levels for maxilla and mandible. However, in our measurement method after defining the surface of the alveolar bone as “SA” and tooth surface as “ST”.We found the corresponding nearest neighbor point in “ST” for each point sampled from “SA”.
In this study, we also measured the number of point with the bone thickness less than 0.1 mm for each tooth and we found there is a statistically significant difference between teeth type except for canine and incisors. Higher number of point<0.1 mm of bone thickness belonged to incisor and canine groups, premolars region shows less point<0.1 mm compared to former group. There were no points<0.1 mm for molars.
CT has revealed that incisor protrusion or retraction represent the movements that have the greatest risk of causing bone dehiscences [28,34]. Thus, we decided to make intra-arch comparison for incisors and canines which are critical areas and more prone to dehiscence and fenestration owing to the thin buccal bone. In this investigation, no statistically significant differences were found regarding buccal bone thickness between maxillary and mandibular incisors and canines. It is somehow difficult to compare the results of present study with others because to our knowledge, there was not any similar study compared the buccal bone thickness between different tooth types using CBCT.
The limitations of this study also need to be addressed; firstly, these data might not be directly applied to Caucasian patients, since they were obtained from Chinese or Singaporean- Chinese subjects. Secondly, since it has been shown that buccal cortical bone thickness can vary on the vertical pattern and, we did not consider the vertical facial patterns in our study, further study may be needed to evaluate and validate the outcomes [41]. Thirdly, although the high accuracy of CBCT for quantitative analyses of the level of buccal and lingual bone plates was demonstrated, limitations in CBCT such as CBCT 3D reconstructions show a small frequency of false-positive results and a high frequency of false-negative results for bone dehiscences, which can affect the accuracy of our result [21,29,30,35]. For obtaining a good spatial resolution, the Field of View (FOV) and the voxel dimension should be both the smallest possible [42].
Conclusion
Within the limitations of the current study, the results showed that the thickness of buccal bone is the lowest in the incisor and canine reigns with no significant difference between canine and incisor groups. The thickness of the alveolar bone in premolar region is significantly greater than incisor and canine regions, but lesser than molar region, so the thickest buccal bone is associated with molar area. No significant differences were found regarding buccal bone thickness between maxillary and mandibular incisors and canines. Based on the limitations of the current study, the authors suggest conducting further studies to evaluate and validate the present results.
Acknowledgment
The authors would like to express their gratitude to Mr. Dongxu Ji for his much appreciated help in the setup of our research and for sharing his expertise in cone beam software manipulation. We are also grateful to Ms. Wong Hung Chew, Senior Biostatistician for her knowledge in statistical analysis. This research was kindly funded by the Academic Research Fund, Faculty of Dentistry, and National University of Singapore.
References
- Mathews DP, Kokich VG. Managing treatment for the orthodontic patient with periodontal problems. Seminars Orthod 1997.
- Bjerklin K, Ericson S. How a computerized tomography examination changed the treatment plans of 80 children with retained and ectopically positioned maxillary canines. Angle Orthod 2006; 76: 43-51.
- Zargham A, Geramy A, Rouhi G. Evaluation of long-term orthodontic tooth movement considering bone re-modelling process and in the presence of alveolar bone loss using finite element method. Orthod Waves 2016; 75: 85-96.
- Castro LO, Castro IO, de Alencar AHG, Valladares-Neto J, Estrela C. Cone beam computed tomography evaluation of distance from cement enamel junction to alveolar crest before and after non-extraction orthodontic treatment. Angle Orthod 2015; 86: 543-549.
- Maheshwari S, Verma SK, Tariq M, Gaur A. Rapid Orthodontics-A critical review. Univ J Dent Sci 2015; 1: 35-38.
- Park Y, Kim J, Lee J. Atlas of contemporary orthodontics (vol III). Sinheung, Seoul, Korea 2005; 178-193.
- Naidu N, Mandava P, Sankar Singaraju G, Ganugapanta VR. Orthodontic mini-implants. Ann Essen Dent 2016; 8.
- Lee KJ, Joo E, Kim KD, Lee JS, Park YC, Yu HS. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic mini screw placement. American journal of orthodontics and dentofacial orthopaedics. Am Assoc Orthod 2009; 135: 486-494.
- Ozdemir F, Tozlu M, Germec-Cakan D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am J Orthod Dentofacial Orthop 2013; 143: 190-196.
- Shinohara A, Motoyoshi M, Uchida Y, Shimizu N. Root proximity and inclination of orthodontic mini-implants after placement: cone-beam computed tomography evaluation. Am J Orthod Dentofacial Orthop 2013; 144: 50-56.
- Hong SB, Kusnoto B, Kim EJ, BeGole EA, Hwang HS, Lim HJ. Prognostic factors associated with the success rates of posterior orthodontic mini screw implants: A subgroup meta-analysis. Korean J Orthod 2016; 46: 111-126.
- Parsa A, Ibrahim N, Hassan B, Stelt P, Wismeijer D. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin Oral Implants Res 2015; 26.
- Deguchi T, Nasu M, Murakami K, Yabuuchi T, Kamioka H, Takano-Yamamoto T. Quantitative evaluation of cortical bone thickness with computed tomographic scanning for orthodontic implants. Am J Orthod Dentofacial Orthop 2006; 129: 7-12.
- Melsen B, Luzi C. The use of mini-implants in clinical orthodontics for the treatment of Class II malocclusions: The Aarhus anchorage system. Mosby 2015; 143-146.
- Oliver DR. Mini-implants: The orthodontics of the future. Am J Orthod Dentofacial Orthop 2016; 150: 547.
- Kim Y, Kim TK, Leem DH. Clinical study of a flap advancement technique without vertical incision for guided bone regeneration. Int J Oral Maxillofacial Implants 2015; 30.
- Greenstein G, Greenstein B, Cavallaro J, Elian N, Tarnow D. Flap advancement: practical techniques to attain tension-free primary closure. J Periodontol 2009; 80: 4-15.
- White SC. Cone-beam imaging in dentistry. Health Physics 2008; 95: 628-637.
- Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol 2006; 77: 1261-1266.
- Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: an in vitro study on native pig and human mandibles. J Periodontol 2005; 76: 665-673.
- Loubele M, Maes F, Vandermeulen D, Denis K, Jacobs R, White S. Assessment of bone segmentation quality of CT scanners using laser scanning. Int J Cars 2006; 389-402.
- Marmulla R, Wortche R, Muhling J, Hassfeld S. Geometric accuracy of the NewTom 9000 cone beam CT. Dentomaxillofacial Radiol 2005; 34: 28-31.
- Pinsky H, Dyda S, Pinsky R, Misch K, Sarment D. Accuracy of three-dimensional measurements using cone-beam CT. Dentomaxillofacial Radiol 2006; 35: 410-416.
- Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Med Pathol Radiol Endodontol 2007; 104: 395-401.
- Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: an in vitro assessment of bony and/or infrabony defects. Dentomaxillofacial Radiol 2008; 37: 252-260.
- Fuhrmann R. Three-dimensional interpretation of alveolar bone dehiscences. An anatomical-radiological study-Part I. J Orofacial Orthoped 1996; 57: 62-74.
- Palomo JM, Kau CH, Palomo LB, Hans MG. Three-dimensional cone beam computerized tomography in dentistry. Dentistry Today 2006; 25: 130.
- Fuhrmann R, Bücker A, Diedrich P. Assessment of alveolar bone loss with high resolution computed tomography. J Periodontal Res 1995; 30: 258-263.
- Loubele M, Van Assche N, Carpentier K, Maes F, Jacobs R, van Steenberghe D. Comparative localized linear accuracy of small-field cone-beam CT and multi-slice CT for alveolar bone measurements. Oral Surg Med Pathol Radiol Endodontol 2008; 105: 512-518.
- Mol A, Balasundaram A. In vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofacial Radiol 2008; 37: 319-324.
- Steiner GG, Pearson J, Ainamo J. Changes of the marginal periodontium as a result of labial tooth movement in monkeys. J Periodontol 1981; 52: 314-320.
- Wennström JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol 1987; 14: 121-129.
- Mulie R, Hoeve A. The limitations of tooth movement within the symphysis, studied with laminagraphy and standardized occlusal films. J Clin Orthod 1976; 10: 882-893.
- Garib DG, Henriques JFC, Janson G, de Freitas MR, Fernandes AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop 2006; 129: 749-758.
- Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop 2010; 137: 109-119.
- Rungcharassaeng K, Caruso JM, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop 2007; 132: 428.
- Sarikaya S, Haydar B, Ciǧer S, Ariyürek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop 2002; 122: 15-26.
- Wehrbein H, Bauer W, Diedrich P. Mandibular incisors, alveolar bone, and symphysis after orthodontic treatment. A retrospective study. Am J Orthod Dentofacial Orthop 1996; 110: 239-246.
- Wehrbein H, Fuhrmann RA, Diedrich PR. Human histologic tissue response after long-term orthodontic tooth movement. Am J Orthod Dentofacial Orthop 1995; 107: 360-371.
- Gracco A, Lombardo L, Mancuso G, Gravina V, Siciliani G. Upper incisor position and bony support in untreated patients as seen on CBCT. Angle Orthod 2009; 79: 692-702.
- Masumoto T, Hayashi I, Kawamura A, Tanaka K, Kasai K. Relationships among facial type, bucco lingual molar inclination, and cortical bone thickness of the mandible. Euro J Orthod 2001; 23: 15-23.
- Molen AD. Considerations in the use of cone-beam computed tomography for buccal bone measurements. Am J Orthod Dentofacial Orthop 2010; 137: 130-135.