- Biomedical Research (2014) Volume 25, Issue 1
Multicentric study on the thrombotic events of patients with Hepatocarcinoma.
Fr??il? O1, Mih?il? RG2*, Nedelcu L3
1Faculty of Medicine, University of Oradea, Romania
2Faculty of Medicine, “Lucian Blaga” University of Sibiu, Romania
3Faculty of Medicine, University of Bra?ov, Romania
- *Corresponding Author:
- Romeo-Gabriel Mih?il?
B-dul Corneliu Coposu, Nr. 2-4, Sibiu
COD 550245
România
Accepted date: October 16 2013
Citation: Fr??il? O, Mih?il? RG, Nedelcu L. Multicentric study on the thrombotic events of patients with Hepatocarcinoma.Biomedical Research 2014; 25 (1): 19-23.
Abstract
In recent years there has been an important change regarding the thrombotic risk estimation of patients with liver cirrhosis, underestimated in the past in favor of the hemorrhagic risk. The appearance of the hepatocarcinoma in the chronic liver diseases evolution increases the thrombotic risk of the patients. We have created a retrospective, multicentric clinical study, including 215 consecutive patients hospitalized in 3 university sites from Transylvania. We have analyzed the complete blood panel parameters, coagulation tests, the thrombotic risk score and the thrombotic and hemorrhagic events of the patients. Over a third of the patients presented thrombosis. The mean platelet volume and the other platelet parameters do not correlate with thrombotic events. The number of platelets correlates directly with the thrombotic risk score. The results are analyzed in the light of the physiopathologic disturbances induced to these patients.
Keywords
Hepatocarcinoma, liver cirrhosis, mean platelet volume, platelets, thrombosis
Introduction
The medical world assisted recently to a reevaluation of the coagulation status of the patients with liver cirrhosis. Until recently it was considered that they have a main hemorrhagic risk. The body of proof accumulated last time argue justified that they are also predisposed to thrombosis. The development of hepatocarcinoma, which occurs more frequently in liver cirrhosis evolution, contributes to the increased thrombotic risk of these patients. The incidence of hepatocarcinoma in liver cirrhosis is 3- 5% per year [1]. Because the prevalence of hepatocarcinoma in our geographic area is much smaller than that from East and South-East Asia, in order to study the thrombotic complications we endorsed the creation of a multicentric study. The increased mean platelet volume (MPV) is an independent risk factor for stroke in patients with chronic atrial fibrillation. We proposed to study also the significance of the MPV and other platelet parameters at patients with hepatocarcinoma.
Material and Method
We carried out a retrospective, multicenter study including all the patients with hepatocarcinoma admitted between January 2010 and December 2012 in the Internal Medicine and Gastroenterology Department of Emergency County Clinical Hospitals of Brașov, Oradea and Sibiu. From the electronic evidence systems of medical data we have selected the following parameters of the patients: age, gender, liver disease coexistent with hepatocarcinoma, the presence of obesity, leukocyte amount, value of hemoglobin and haematocrit, mean platelet volume (MPV), platelet distribution width (PDW), platelet large cell ratio (P-LCR), plateletcrit (PCT), international normalized ratio (INR), prothrombin activity, Quick's test (QT), activated partial thromboplastin time (APTT), eventual portal vein thrombosis, thrombotic antecedents (myocardial infarction, ischemic stroke, thrombophlebitis, carotid artery occlusion, inferior vena cava thrombosis, suprahepatic vein thrombosis, partially thrombosed aortic
aneurysm, superior mesenteric vein thrombosis), recent thromboses (in the past 2 months), ongoing thromboses, the total number of thrombotic events, thrombotic risk score, recent hemorrhages (in the past 2 months). The thrombotic risk score was calculated as: 1 point for each of the following factors that were present: platelets number before chemotherapy ≥ 350x109/l, hemoglobin level below 100 g/l or use or erythropoietin, the number of leukocytes before chemotherapy over 11x109/l, body mass index ≥ 35 kg/m2 [2].
The data obtained was statistically analyzed: arithmetic mean, standard deviation, t Student test and Pearson test.
Results
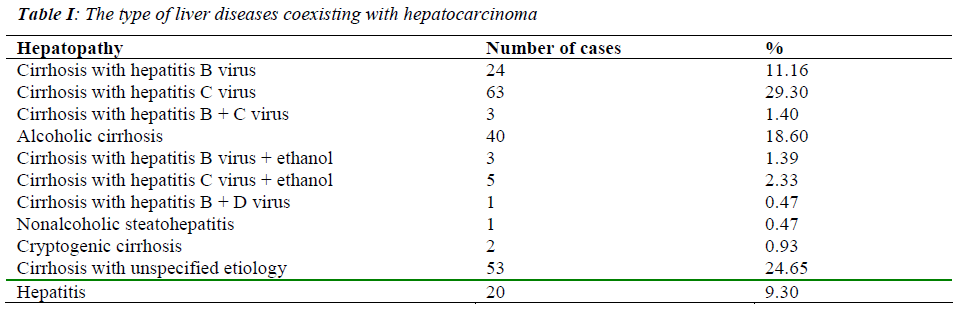
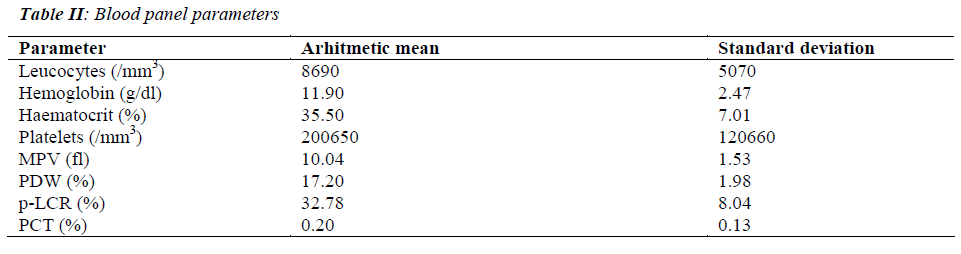
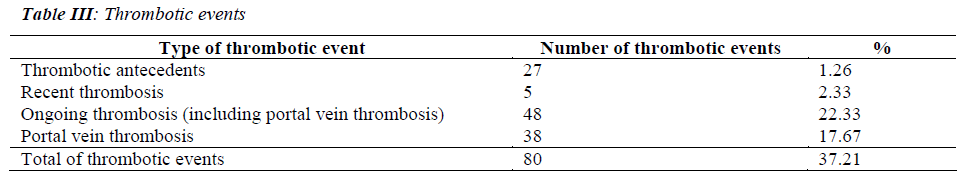
The group included 215 patients. The mean age was 65.96+/-10.83 years. Gender repartition: 140 men (65.1%) and 75 women (34.9%). The type of hepatopathy of the patients with hepatocarcinoma is found in table I. The analyzed parameters of the complete blood panel are found in table II. The coagulation tests had the following mean values: prothrombin time 16.68+/-4.28 s, prothrombin activity 60.68+/-16.97%, INR 1.37+/-0.41 and APTT 34.18+/-12.61 s. The mean thrombotic risk score was 0.57+/-0.78. The thrombotic events are represented in table III. Recent hemorrhagic accidents: 31 (14.42%). The coagulation tests were not correlated with the thrombotic events. The platelet count, MPV and the other platelet indices were not correlated with the thrombotic risk score, the thrombotic antecedents, and current thrombotic events and with the total thrombotic events of the patient even after the exclusion from the group of the patients with recent hemorrhagic episodes. Neither after the exclusion of the patients with current thrombosis the above mentioned parameters were not correlated with the thrombotic antecedents or the MPV with the platelet count of these patients (r=0.173). The thrombotic risk score was not correlated with MPV (r=-0.07) or with the past (r=0.023), current (r=-0.078) or with the total number of thrombotic events (r=-0.043), but was directly correlated with the platelet count (r=0.447).
Discussion
An increased MPV, indicator of platelet activation [3], is considered a thrombotic risk factor in different circum stances, including to the patient with atrial fibrillation, to whom the increased risk of ischemic stroke is associated [4]. Also the patients with fatty liver disease have MVP increased. MPV inverse correlates with the platelet number at these patients [3], as at healthy subjects. Any situation that involves increased platelet consumption (thrombosis with various locations) is followed by the release into the blood stream of sequestered platelets until then in the spleen, where are young and with increased MPV - hyper-functional platelets. Also the patients with primary immune thrombocytopenia, with platelet destruction through immune mechanisms, have increased MPV. Also in patients with chronic hepatitis B a significantly higher MPV compared to the healthy control population has been found. The MPV was not increased for those with advanced liver fibrosis compared with those with minor fibrosis [5]. The MPV does not have the same value in any liver disease. Thus, in another study, the number of platelets and the MPV of the patients with hepatopathies were significantly smaller than control group. Additionally, in cirrhosis the platelet number and the MPV do not correlate inversely as in healthy subjects [6]. We have not found any correlation between the MPV and platelet number, the thrombotic risk score or the thromboses of patients with hepatocarcinoma, most of them occurred in the development of some liver cirrhoses.
Besides the MPV, we have also studied the other platelet parameters because in liver cirrhosis the PDW and the megathrombocyte index are better indicators of an altered platelet homeostasis compared with MPV [7]. Neither these have a correlation with the thrombotic events.
Why are there no correlations between the platelet indices and the thrombotic events at patients with hepatocarcinoma? There are multiple explanations: MPV and the other platelet parameters can be influenced by the thrombotic or hemorrhagic events but it was observed that the MPV does not increase when the platelet number decreases at cirrhotic patients. Because the majority of the patients with hepatocarcinoma have liver cirrhosis, this finding was confirmed for our study group, too. The thrombocytopenia of patients with liver cirrhosis +/- hepatocarcinoma (explainable by spleen sequestering and increased destruction by hypersplenism, with procoagulation status and low thrombopoietin levels) doesn’t lead to an increased number of medullary megakaryocytes as it happens in other peripheral thrombocytopenia cases. In case of thromboses, the platelet number is lower than in their absence [8] because the hematopoietic bone marrow doesn’t compensate for the platelets loss (through young platelets with high MPV). It results that the thrombotic risk of patients with liver cirrhosis + hepatocarcinoma is not influenced by the MPV but by the disturbance of the coagulation, fibrinolysis and homeostasis processes.
The patients with decompensated liver cirrhosis have an impaired hepatic synthesis, affecting also the synthesis of some coagulation factors (I, II, V, VII, IX, X, XI, XIII). Additionally the platelets function if deficient. It was thought for a long time that the liver cirrhosis is a model of aquired hemorrhagic coagulopathy. In this nosologic entity not only the procoagulation factors are decreased but also some of the anticoagulation factors, thus the global coagulation tests are usually normal for patients with chronic liver diseases. The thrombotic events are promoted by the increased level of coagulation factor VIII, von Willebrand factor and by the decrease of the antithrombin, plasminogen, protein C and S levels. There is a weak correlation between the hemorrhagic risk and the usual hemostasis tests [9]. Cirrhotic patients can have an increased risk of thrombotic events [10,11] due to a systemic and portal prothrombotic state [11]. It is believed that the portal vein thrombosis increases the morbidity and mortality associated with the liver transplant at patients with liver cirrhosis. When the thrombus extends to the superior mesenteric vein this procedure becomes contraindicated [12]
The presence of the hepatocarcinoma grafted on the cirrhosis significantly increases the patient’s thrombotic risk. In our study 37.21% of the patients had thromboses in antecedents or during the admission. In the scientific literature there was one case published, that, starting from the diagnosis had disseminate tumor thrombosis, including mobile thrombus in the right atrium and pulmonary embolism [13]. The portal vein thrombosis at patients with hepatocarcinoma constitutes an independent prognostic factor for them [14]. At 17.67% of the patients studied by us the thrombosis of the portal vein was present. The thrombi can be present even in the biliary tract at these patients leading to difficulties in differentiating from biliary calculus or cholangiocarcinoma [15].
The presence of the portal vein thrombosis can create imagistic diagnostic difficulties of the hepatocarcinoma because the characteristic hypervascularization can be absent, supplied by the hepatic parenchyma background [16]. TGFβ1 had higher values at patients with hepatocarcinoma with portal vein thrombosis and can be involved in the neoplasia progression [17].
What is the explanation of this prothrombotic status? The patients with hepatocarcinoma have significant changes regarding the coagulation and the fibrinolysis: a decreased number of platelets, antithrombin level, plasminogen, protein C, coagulation factors XI, X, VII, V was discovered whereas the APTT, thrombin time, fibrin degradation products, von Willebrand factor, tissue plasminogen activator and prothrombin fragments 1 + 2 had higher values than in the control group (without hepatocarcinoma) [18].
After splenectomy or simultaneously hepatectomy and splenectomy for hepatocarcinoma made on a group of 38 consecutive patients with liver cirrhosis, the postoperatory incidence of the portal or splenic veins thrombosis was 34.2% [19]. After hepatocarcinoma resection the presence of the portal vein thrombosis was significantly correlated with shorter survival without progression [20]. Venous thromboses (of portal or hepatic veins) were cited after hepatocarcinoma ablation by radiofrequency but their incidence was only of 1.08% in a group of 1046 patients, with 1379 ablations [21]. Besides hepatocarcinoma, the risk factors for portal vein thrombosis are: liver cirrhosis, abdominal infections, umbilical catheterization, abdominal surgery, including hepatectomy, and very rarely thrombophilia [22]. The deficit of proteins C and S was involved in the chronic thrombosis of the portal vein [23]. The portal vein thrombosis can be influenced by the gene IL-28B polymorphism: an increased thrombotic event risk was observed at Chinese Han population with genotype GA + GG at rs4803223 polymorphism [24]. Hypoxic hepatitis does not appear only after digestive hemorrhage at cirrhotic patients but also at those with portal vein thrombosis, that was proved to be an independent risk factor for hypoxic hepatitis [25].
Could the thrombotic complications of these patients be prevented? In a recent Italian study, enoxaparin administered to patients with Child-Pugh B7-C10 liver cirrhosis, at dosage of 4000UI/day, for 48 weeks, has significantly reduced the incidence of the portal vein thrombosis and has delayed the liver decompensation, contributing to the patient’s life expectancy prolongation, in safety conditions [26]. Additionally, the anticoagulant treatment can lead to splenic-portal ax re-permeabilization and can prevent the thrombosis progression [12]. However, the guide of the American Association for the Study of Liver Diseases makes no recommendation on anticoagulant treatment for cirrhotic patients with venous thrombosis [9]. A case of recanalization of the portal vein in a patient with advanced hepatocellular carcinoma after treatment with sunitinib was reported [27].
Conclusions
Over a third of the patients with hepatocarcinoma had in the past or at the study moment venous thrombosis. The most frequent thrombosis was of the portal vein (17.67%). The thrombotic risk was not correlated with MPV or with other platelet indices, but was directly correlated with platelet number. The thrombotic events were not correlated with the thrombotic risk score or with the platelet indices. The low number of megakaryocytes and the low level of thrombopoietin explain this lack of correlation. The coagulation, fibrinolysis and hemostasis processes dysfunctions and the direct tumoral effects are involved in the thrombotic events of these patients and can aggravate the disease evolution and, sometimes, establish the prognosis. Therefore, their prophylaxis must be taken into account in each case and the opportunity of it must be analyzed dependent on individual particularities and risks.
References
- Fares N, Péron JM. Epidemiology, natural history, and risk factors of hepatocellular carcinoma. Rev Prat 2013;63: 216-217.
- Khorana AA, Kuderer NM, Culakova E, Lzman GH,Francis CW. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 2008; 111: 4920-4907
- Ozhan H, Aydin M, Yazici M, Yazgan O, Basar C, Gungor A, Onder E. Mean platelet volume in patients with non-alcoholic fatty liver disease. Platelets 2010; 21: 29-32.
- Turfan M, Erdogan E, Ertas G, Duran M, Murat SN, Celik E, Baydar C, Tasal A, Vatankulu MA, Sevgili E, Kul S, Yoldas T, Goktekin O. Usefulness of mean platelet volume for predicting stroke risk in atrial fibrillation patients. Blood Coagul Fibrinolysis 2013; 24: 55-58.
- Ekiz F, Yüksel O, Koçak E, Yılmaz B, Altınbaş A, Çoban S, Yüksel I, Üsküdar O, Köklü S. Mean platelet volume as a fibrosis marker in patients with chronic hepatitis B. J Clin Lab Anal 2011; 25: 162-165.
- Jørgensen B, Fischer E, Ingeberg S, Hollaender N, Ring-Larsen H, Henriksen JH. Decreased blood platelet volume and count in patients with liver disease. Scand J Gastroenterol 1984; 19: 492-496.
- Luzzatto G, de Franchis G, Fabris F, Gerunda GE, Girolami A. Increased proportion of giant platelets and platelet distribution width are better indicators of altered platelet homeostasis than mean platelet volume in liver cirrhosis. Folia Haematol Int Mag Klin Morphol Blutforsch 1988; 115: 719-726.
- Ikura Y, Ohsawa M, Okada M, Iwai Y, Wakasa K. The significance of platelet consumption in the development of thrombocytopenia in patients with cirrhosis. Am J Med Sci 2013; 346: 199-203.
- Prelipcean CC, Fierbinteanu-Braticevici C, Drug VL, Lăcătuşu C, Mihai B, Mihai C. Liver cirrhosis-- procoagulant stasis. Rev Med Chir Soc Med Nat Iasi 2011; 115: 678-685.
- Amarapurkar PD, Amarapurkar DN. Management of coagulopathy in patients with decompensated liver irrhosis.Int J Hepatol 2011; 2011: 695470.
- Ferro D, Angelico F, Caldwell SH, Violi F. Bleeding and thrombosis in cirrhotic patients: what really matters?Dig Liver Dis 2012; 44: 275-279.
- Seijo S, García-Criado A, Darnell A, García-Pagán JC. Diagnosis and treatment of portal thrombosis in liver cirrhosis. Gastroenterol Hepatol 2012; 35: 660-666.
- Panduranga P, Al-Mukhaini M, Ratnam L, Al-Harthy S. Mobile right atrial thrombus with pulmonary thromboembolism in a patient with advanced hepatocellular carcinoma and disseminated tumor thrombosis. Heart Views 2011; 12: 173-177.
- Lee SS, Shin HS, Kim HJ, Lee SJ, Lee HS, Hyun KH, Kim YH, Kwon BW, Han JH, Choi H, Kim BH, Lee JH, Kang HY, Shin HD, Song IH. Analysis of prognostic factors and 5-year survival rate in patients with hepatocellular carcinoma: a single-center experience. Korean J Hepatol 2012; 18: 48-55.
- Uchima-Koecklin H, Balderramo D, Cárdenas A. Bile duct hepatocellular carcinoma thrombi. Gastroenterol Hepatol 2012; 35: 326-329.
- Thian YL, Low AS, Chow PK, Ooi LL, Chung AY, Low SC, Xie W, Thng CH. Atypical enhancement pattern of hepatocellular carcinoma with portal vein thrombosis on multiphasic CT. Ann Acad Med Singapore 2011; 40: 454-459.
- Lee D, Chung YH, Kim JA, Lee YS, Lee D, Jang MK, Kim KM, Lim YS, Lee HC, Lee YS. Transforming growth factor beta 1 overexpression is closely related to invasiveness of hepatocellular carcinoma. Oncology 2012; 82: 11-18.
- Alkim H, Ayaz S, Sasmaz N, Oguz P, Sahin B. Hemostatic abnormalities in cirrhosis and tumor-related portal vein thrombosis. Clin Appl Thromb Hemost 2012; 18: 409-415.
- Ushitora Y, Tashiro H, Takahashi S, Amano H, Oshita A, Kobayashi T, Chayama K, Ohdan H. Splenectomy in chronic hepatic disorders: portal vein thrombosis and improvement of liver function. Dig Surg 2011; 28: 9- 14.
- Liu L, Miao R, Yang H, Lu X, Zhao Y, Mao Y, Zhong S, Huang J, Sang X, Zhao H. Prognostic factors after liver resection for hepatocellular carcinoma: a singlecenter experience from China. Am J Surg 2012; 203: 741-750.
- Kim AY, Rhim H, Park M, Lee MW, Kim YS, Choi D, Lim HK. Venous thrombosis after radiofrequency ablation for hepatocellular carcinoma. AJR Am J Roentgenol 2011; 197: 1474-1480.
- Lertpipopmetha K, Auewarakul CU. High incidence of hepatitis B infection-associated cirrhosis and hepatocellular carcinoma in the Southeast Asian patients with portal vein thrombosis. BMC Gastroenterol 2011; 11:66.
- Das SK, Ray A, Jana CK, Banerjee N, Khaskil S.Chronic portal vein thrombosis due to combined deficiency of protein C and protein S. J Indian Med Assoc 2011; 109: 753-754.
- Wang Y, Zhang HH, Chen YH, Xie XW, Liao WJ, Qin LL, Sun XY, Fei R, Wang XY, Wei L, Chen HS, Mei MH. Correlation between interleukin-28B genetic polymorphisms and primary hepatocellular carcinoma.Zhonghua Yu Fang Yi Xue Za Zhi 2012; 46: 527-532.
- Amitrano L, Guardascione MA, Martino R, Manguso F, Menchise A, Balzano A. Hypoxic hepatitis occurring in cirrhosis after variceal bleeding: still a lethal disease. J Clin Gastroenterol 2012; 46: 608-612.
- Villa E, Cammà C, Marietta M, Luongo M, Critelli R, Colopi S, Tata C, Zecchini R, Gitto S, Petta S, Lei B,Bernabucci V, Vukotic R, De Maria N, Schepis F, Karampatou A, Caporali C, Simoni L, Del Buono M, ambotto B, Turola E, Fornaciari G, Schianchi S, Ferrari A, Valla D. Enoxaparin Prevents Portal Vein Thrombosis and Liver Decompensation in Patients With Advanced Cirrhosis. Gastroenterology 2012; 143: 1253-1260.
- Basso M, Basso M, Iaculli A, Pompili M, Riccardi L, Barbaro B, Rufini V, Cassano A, Castaldi P, Barone C.Complete Metabolic Response with Recanalization of Portal Vein Tumor Thrombosis after Sunitinib in a Patient with Advanced Hepatocellular Carcinoma. Case Rep Oncol 2010; 3: 391-396.