Research Article - Biomedical Research (2017) Volume 28, Issue 17
Investigation of the effect of Elaeagnus angustifolia flower capsule on sexual satisfaction and levels of androgenic hormones in 18-40 year old married women with low sexual desire referring to selected clinics of Shiraz University of medical sciences, 2012
Zeinalzadeh Sanaz1, Dabbaghmanesh Mohammad H2, Akbarzadeh Marzieh3*, Mohagheghzadeh Abdol Ali4 and Sayadi Mehrab51Department of Midwifery, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Community Based Psychiatric Care Research Center, Shiraz, Iran
2Department of Internal Medicine, Endocrine and Metabolism Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
3Department of Midwifery, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Maternal-Foetal Medicine Research Center, Shiraz, Iran
4Department of Traditional Pharmacy, School of Pharmacy, Shiraz University of Medical Sciences, Shiraz, Iran
5Department of Bio-Statistics, Shiraz University of Medical Sciences, Shiraz, Iran
- *Corresponding Author:
- Akbarzadeh Marzieh
Department of Midwifery, School of Nursing and Midwifery
Shiraz University of Medical Sciences
Maternal-Foetal Medicine Research Center, Shiraz, Iran
Accepted date: July 24, 2017
Abstract
Purpose: Sexual satisfaction is one of the main dimensions of family life. This study aimed to investigate the effect of Elaeagnus angustifolia flower capsule on sexual satisfaction and levels of androgenic hormones with low sexual desire in 2012.
Methods: This randomized clinical trial was conducted on 84 women aged 18-40 y old. The intervention group that was not suffering from hypothyroidism and hyperprolactinemia received E. angustifolia, while the control group received placebo (4 capsules a day, 2 capsules every 12 h, for 35 d). Female Sexual Function Index (FSFI) and enrich marital satisfaction questionnaire were filled out and the levels of androgenic hormones were measured before and after the intervention.
Results: No significant difference between was observed between the two groups regarding sexual desire disorder before the intervention (P=0.269). After the intervention, however, this measure decreased from 53.7 to 19.5, which was statistically significant (P=0.001). Nevertheless, no significant difference was found between the two groups regarding sexual satisfaction mean score (0.89 vs. 0.96) and mean level of androgenic hormones before and after the intervention (P>0.05).
Conclusion: E. angustifolia flower capsule was effective in improvement of sexual desire, but it did not improve the sexual satisfaction and level of androgenic hormones.
Keywords
Sexual desire, Elaeagnus angustifolia, Flower, Sexual satisfaction.
Introduction
Sexual satisfaction is one of the main dimensions of family life, which is necessary for family establishment and raising the children, it plays a critical role in family’s health and welfare [1,2]. Evidence has shown that emotional, physical, and sexual intimacy and common religious beliefs are associated with the duration and stability of marital satisfaction, thereby affecting sexual satisfaction, as well [3,4]. Some studies have emphasized that sexual issues are among the main issues of marital life [5]. Additionally, satisfaction, quality of sexual relationships, and expression of love have been considered as determinants of sexual satisfaction [6].
Sexual disorder is defined as any problem leading to imbalance in and dissatisfaction with sexual relationship. According to DSM-IV, sexual disorder means disorder in sexual desire and psycho-social changes affecting sexual response cycle and leading to interpersonal problems including low sexual desire, sexual aversion, sexual arousal disorder, orgasmic disorder, pain during intercourse, and vaginismus. The prevalence of these disorders cannot be accurately estimated due to sociocultural barriers, taboos, and misunderstandings. Yet, these disorders highly influence the couples’ marital satisfaction, self-confidence, feeling “less connectedness”, relationships, and social activities [7,8]. Overall, it has been estimated that 30-63% of women suffer from sexual disorders [9].
Laumann et al. reported that one third of women had low sexual desire, one fourth had orgasmic disorder, one fifth had lubrication problems, and one fifth was not satisfied with their sexual relationships [10].
Similarly, Nejad conducted a study on 20-60 y old women in various provinces in Iran. In that study, the prevalence of low sexual desire, lack of sexual arousal, lack of orgasm, and pain during intercourse was reported as 35%, 30%, 37% and 26%, respectively [11].
Recent studies in Europe have shown that out of the 2467 women in France, England, Germany and Italy, 16% of those with low sexual desire were in 20-49 y old age group and 42% were 50-70 y old with normal menopause [12]. Moreover, studies have mostly focused on pharmacological treatments for male’s sexual dysfunction and less attention has been paid to female’s sexual disorders [13,14].
In the studies conducted on mental health and sexual satisfaction, a significant relationship has been found between sexual satisfaction and mental health as well as between marital pressure and mental disorders, particularly depression, anxiety disorders, and physical diseases. Also, studies have revealed a mutual relationship between sexual satisfaction and marital satisfaction [15].
Up to now, many studies have been carried out on marital consultation and creation of sexual satisfaction. For instance, Kleinstäuber stated that increase in knowledge and provision of communication training for health care providers to the elderly regarding sexual health played a key role in mental health and well-being in older adults [16]. Hallberg showed the significant effect of Cognitive-Behavioural Therapy Group intervention on sexual satisfaction in the intervention group compared to the control group [17].
Recently, measures have been taken towards pharmacological treatment of female’s sexual dysfunction and improvement of sexual satisfaction mostly aiming at improvement of androgen deficiency, increase of blood flow towards sexual organs, and stimulation of central nervous system [14,18,19]. Complementary and Alternative Medicine (CAM) is also another therapeutic method for treatment of sexual disorders [20]. Herbal medicine, as a branch of CAM, has been utilized in various communities for a thousand years and has been highly recommended to women by midwives [21,22]. Ginseng, Yohimbine, and Ginkgo Biloba are among the effective herbal medicines used for sexual disorders [23]. However, researches have shown that Yohimbine was more effective in treatment of male’s sexual disorders in comparison to female’s sexual dysfunction [24]. According to studies, herbal medications, such as ArginMax, Ginseng, Ginkgo Biloba, and ethanol extract [25] improved sexual dysfunction through increase of Nitric Oxide (NO) production. NO is among the compounds derived from E. angustifolia. E. angustifolia flower grown in some parts of Iran which, according to the specialists in traditional medicine, is hot and dry, is aromatic, and can stimulate sexuality, especially in young girls and women [26].
In Iranian traditional medicine for fruits, flowers and gum leaves of E. angustifolia plants are listed many health benefits that contain significant amounts of flavonoids, terpenoids, carvacrol and sitosterol [26,27].
Studies have shown that this herb has properties such as antiinflammatory, antioxidant activities, anti-fatigue, and muscle relaxant activity via flavonoid component [28-31]. So far, nine flavonoids were isolated from this plant, including catechin, epicatechin, gallocatechin, epigallocatechin, kaempferol, quercetin, luteolin, isorhamnetin, and isorhamnetin-3-O-beta- D--galactopyranoside [32,33]. Flavonoid components may, in turn, result in muscle relaxation [31].
Through the recent 30 y, no studies have investigated the effect of E. angustifolia flower on males and female’s sexual disorders and most studies have been conducted on the effect of this medicinal plant on non-sexual issues.
Nowadays, sociologists and psychologists believe that the society’s health depends on family’s health. Furthermore, hiding the problems does not help their resolution and may even cause the problems to present as a crisis. Sexual disorders are also among the problems which individuals tend to hide. Considering the importance of sexual satisfaction and its effects on family’s stability and the fact that no studies have been conducted on this issue in Iran, the present study aimed to investigate the effect of E. angustifolia flower capsule on sexual satisfaction of married women between 18 and 40 y old suffering from low sexual desire.
Methods
Study design
The present Randomized Clinical Trial (RCT) aimed to assess the effects of E. angustifolia flower capsule and placebo on sexual desire in 18-40 y old married women referring to health clinics of Shiraz, Iran.
Setting and sample
Based on the study objectives and the previous studies conducted on the issue, considering alfa=5%, power=80%, least mean difference=0.6, and variance=0.92, and using the following formula, a 72-subject sample size (36 in each group) was determined for the study [34-36].
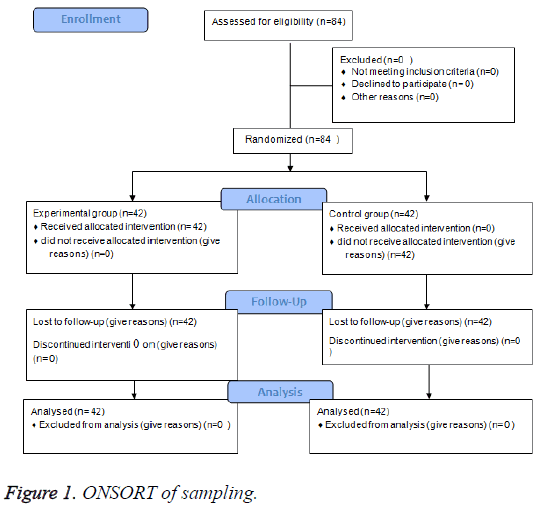
Nonetheless, due to the longitudinal design of the study, repeated measurements, and loss rate of 10%, the sample size was increased to 84 subjects (42 in each group) (Figure 1).
In this study, subjects were selected using purposive sampling. In doing so, the researcher referred to the selected centers and started selecting the participants. In case the selected individual could not participate in the study for any reason, the next one was replaced. Then, using the table of random numbers, numbers ending in 1 or 2 were allocated to the first group, while those ending in 3-5 were allocated to the second group. Afterwards, the two groups were randomly labelled as A or B representing the intervention and the control groups.
Ethical considerations
This research project was approved by the local Ethics Committee of SUMS. To ensure ethical issues, all women who participated in the study were fully informed about the nature and purpose of the study, and an emphasis was put on the voluntary nature of their participation. Written informed and oral consent was obtained from the women before collection of the data. The research proposal No. 91-01-33-4439 was financially supported by Endocrine and Metabolism Research Center, Shiraz University of Medical Sciences.
Data collection and procedure
The inclusion criteria of the study were being willing to take part in the study, signing written informed consents for participation in the study, being married and between 18-40 y old, not being pregnant, not suffering from hypothyroidism and hyperprolactinemia, not breastfeeding, not consuming drugs affecting sexual function such as common antidepressants, not suffering from dyspareunia or vaginismus, not using hormone drugs particularly oral contraceptive pills, lack of drug or alcohol abuse, and not having familial or emotional problems. On the other hand, the exclusion criteria of the study were lack of willingness to continue cooperation in the study and suffering allergic reaction to the drug.
The study data were collected using demographic information form, Female Sexual Function Index (FSFI), Enrich marital satisfaction questionnaire, and measurement of TSH and prolactin.
FSFI which contains 19 items evaluates the female’s sexual function in 6 domains of sexual desire, arousal, lubrication, orgasm, satisfaction, and pain. The study women were required to answer the questions according to their sexual desire and function during the past 4 weeks. In general, scores<28 are considered as sexual dysfunction. Nevertheless, since assessment of pain (6 points) was omitted from the present study, score of 22 was considered instead of 28. The reliability and validity of the Persian version of FSFI were determined by Mohammadi et al. in 2008. The reliability of the whole questionnaire and the subscales was confirmed by Cronbach’s alpha>0.70. Moreover, investigation of the validity of the Persian version of this questionnaire indicated a significant difference between the total mean score and the mean scores of the subscales in the two groups (P<0.001) [37,38].
Enrich marital satisfaction questionnaire was used to evaluate the sexual satisfaction. This questionnaire has been utilized in many researches and clinical studies as a reliable instrument. The original version of the questionnaire includes 115 items, but various versions of this questionnaire have been designed up to now. In this study, the researchers made use of the 47 item version of this scale whose validity and Cronbach’s alpha coefficient have been respectively reported as 95% and 85% by Nejad. The items of this questionnaire are answered through a 5-option Likert scale ranging from 1 (completely agree) to 5 (completely disagree). The maximum score of the scale is 235 and higher scores represent higher sexual satisfaction [39].
In case the individuals met the inclusion criteria of the study and signed written informed consents, they were required to fill out Hurburt index of sexual desire. Then, they were randomly allocated to either the intervention or the control group. Afterwards, blood was taken from the study participants in order to measure their serum levels of sexual hormones. The intervention group received E. angustifolia flower capsule and the control group received the placebo (4 capsules a day, 2 capsules every 12 h, for 35 d).
All the statistical analyses were performed using the SPSS statistical software. The study data were analyzed using descriptive statistics. Paired T-test was used to compare the mean scores of sexual desire within groups before and after the intervention. Besides, Pearson correlation coefficient was used to determine the relationship between sexual desire and age, marriage age, length of marriage, husband’s age, and husband’s marriage age. In addition, Spearman correlation coefficient was employed to assess the association between sexual desire and level of education. P<0.05 was considered as statistically significant.
Data analysis
The data were analyzed using T-test, Chi-square test, Fisher’s exact Test, and Pearson correlation.
Results
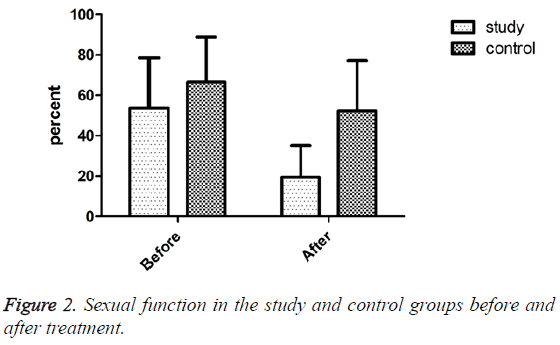
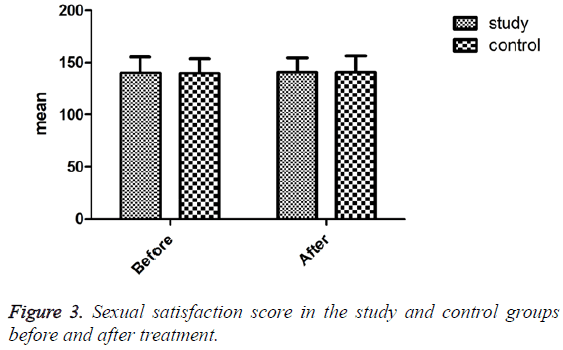
The results of independent T-test revealed no significant difference between the two groups regarding the level of TSH (P=0.448) and prolactin (P=0.179) before the intervention. Also, no significant relationship was observed between sexual desire and age (r=-0.129, P=0.129), marriage age (r=0.002, P=0.985), length of marriage (r=0.119, P=0.189), husband’s age (r=-0.175, P=0.050), and husband’s marriage age (r=-0.095, P=0.294) (Table 1). The mean score of sexual desire was 60.66+7.51 in the employed women and 62.57+9.71 in the homemaker ones, but the difference was not statistically significant (P=0.266). Also, no significant difference was found between the two groups concerning sexual desire before the intervention (P=0.269). After the intervention, however, frequency of sexual desire disorder decreased from 53.7% to 19.5% in the intervention group (P=0.001) (Figure 2). Nevertheless, no significant difference was observed between the intervention and control groups regarding the sexual satisfaction mean score before (p=0.893) and after the intervention (p=0.963) (Figure 3). Also, no significant difference was found between the two groups concerning the mean levels of androgenic hormones (free testosterone, DHEAS, and total testosterone) before and after the intervention (P>0.05) (Table 2).
| Sexual desire | Demographic variables | r-value | p-value |
|---|---|---|---|
| Age | -0.129 | 0.121 | |
| The age of marriage | 0.002 | 0.985 | |
| Duration of marriage | -0.119 | 0.185 | |
| Age of wife | -0.175 | 0.05 | |
| The age of Married wife | -0.095 | 0.294 | |
| Education | 0.147 | 0.102 | |
| Spouse education | -0.1 | 0.916 |
Table 1: The relationship between sexual desire and demographic variables.
| Hormonal test | Intervention groups |
Elaeagnus angustifolia flower capsule group | Control group | p-value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Free testosterone | Before | 0.57 ± 0.58 | 0.76 ± 0.68 | 0.199 |
| After | 0.57 ± 0.58 | 0.87 ± 0.64 | 0.411 | |
| DHEAS | Before | 1.28 ± 0.65 | 1.48 ± 0.75 | 0.184 |
| After | 1.41 ± 0.68 | 1.47 ± 0.72 | 0.716 | |
| Total testosterone | Before | 0.59 ± 0.35 | 0.63 ± 0.21 | 0.531 |
| After | 0.59 ± 0.23 | 0.59 ± 0.19 | 0.882 |
Table 2: Comparison of the results of hormone experiments in the two groups.
Discussion
In this study, prolactin and TSH were measured before the intervention in order to ensure the normal function of the thyroid and lack of suffering from hyperprolactinemia. Atis et al. investigated sexual function in the women suffering from hypothyroidism and subclinical hypothyroidism. Their study was conducted on 25 women with hypothyroidism, 25 women with subclinical hypothyroidism, and 20 healthy women in the control group. According to the results, sexual dysfunction was more prevalent among the participants with thyroid disorders (P=0.006) [40].
Kadioglu et al. investigated sexual function among the patients with hyperprolactinemia. Out of the 25 women suffering from hyperprolactinemia, 22 (88%) had sexual dysfunction. However, only 4 out of the 16 healthy women in the control group (25%) had sexual dysfunction [41].
The results of the present study showed that E. angustifolia flower was effective in sexual desire, but no significant increase was observed in the level of sexual hormones in the intervention group. Up to now, no studies have been conducted on the effect of E. angustifolia flower on sexual disorders and this issue has only been discussed in Iranian traditional medicine and ancient books, such as Zakhireh Kharazmshahi (Treasure of Kharazmshahi). The only research conducted in Iran on this herbal medicine was that of Akbarzadeh et al. which showed that it affects the sexual dysfunction and anxiety of women [42,43]. Other studies have been conducted on different properties of E. angustifolia plant or on some diseases [44,45]. Therefore, the study results are compared with those of the studies performed on other herbal medications used for sexual disorders. Maca is among the medicinal plants leading to improvement of sexual desire. This plant is from brassica (mustard) family and has been proved to be effective in improvement of female’s sexual desire and male’s erectile dysfunction [46].
Ito et al. investigated the effect of ArginMax, as a nutritional supplement, on improvement of female’s sexual function in the US in 2001. That double-blind clinical trial was conducted on 77 women between 22 and 71 y old who suffered from sexual dysfunction. ArginMax is a supplement including Korean ginseng extract, Ginkgo, damiana, L-Arginine, multivitamin, and minerals. In that study, 86 participants were randomly allocated to either the placebo or the ArginMax group. After 4 weeks, the participants in the ArginMax group reported a considerable improvement in their sexual life (73.5%) compared to the placebo group (37.2%) (P<0.01). Sexual desire had also significantly increased in the intervention group (70.6%) in comparison to the control group (41.9%) [25].
Overall, previous studies have shown that increase in the blood flow in clitoris and vagina during sexual arousal results from NO/cyclic guanosine monophosphate (CGMP) pathway [46,47]. Increase in NO production in other herbal medicines have also improved sexual function and increased sexual hormones. NO is also among the compounds derived from E. angustifolia [35]. Improvement of sexual desire in the present study might also be due to the slight increase in the sexual hormones in the intervention group compared to the control group. In any event, further studies should be conducted on different doses of this extract to assess the androgenic hormones levels. In this way, more scientific conclusions can be drawn by comparing the clinical symptoms to blood hormone levels.
Also researches have shown that certain flavonoids E. angustifolia plants have vascular smooth muscle relaxation efforts [48]. Flavonoids are also believed to increase NO and cyclic Endothelial Guanosine Mono-Phosphate (cGMP), eventually resulting in vascular smooth muscle relaxation. Evidence has shown that NO, as an endogenous vascular dilator, plays a critical role in regulation of vascular tone and is the main stimulant of cGMP production in smooth muscles [49-51]. Increase in cGMP leads to an increase in the activity of kinase G protein which leads to vascular relaxation by phosphorylation of different molecules [52].
On the other hand, some experts believe that increase of cGMP results in smooth muscle vascular relaxation through other mechanisms [53]. For instance, cGMP may lead to relaxation of smooth muscles by decreasing the intracellular calcium concentration [54]. The positive effect of E. angustifolia on sexual dysfunction in this study may be justified by the aforementioned mechanisms. The findings of the current study demonstrated no significant difference between the two groups regarding sexual satisfaction.
Capral et al. conducted a study on 370 women between 40 and 65 y old in Brazil to investigate the effects of climacteric symptoms on the women’s sexual function. According to the FSFI scores, 67% of the women in the climacteric stage had sexual dysfunction and obtained low scores in all dimensions including sexual desire (P<0.001) [55].
Moreover, Ornat et al. conducted a study on 260 Spanish women aged 40 to 59 y old using 14-item Changes in Sexual Functioning Questionnaire (CSFQ-14) and Satisfaction with Life Scale (SWLS). The results of that study revealed a direct relationship between reduction of sexual function and severity of menopause symptoms. In addition, the results indicated a direct association between CSFQ and SWLS scores (P<0.04) but a reverse relationship between CSFQ score and menopause symptoms (P<0.02) [56]. These results were in contrast to those of the current study.
Sexual function is one of the prognostic factors of sexual satisfaction. A large number of studies have referred to the positive impact of sexual function on sexual satisfaction [57]. Auslander indicated that the individuals with higher sexual satisfaction had more positive relationships with their spouses, had less emotional sensitivity in their relationships, and were more sexually active [58]. Similarly, Litzinger et al. believed that expression of love and sexual relationships increased the marital satisfaction [6]. Brezsnyak et al. also stated that increase in marital satisfaction led to a considerable increase in sexual satisfaction [5]. In the same line, Basson mentioned that sexual function is like a cycle which is affected by various biological and psychological, and in other words internal and external, factors [59]. This finding might be due to the fact that sexual relationship forms the couple’s perception of each other and can guarantee their marital life. Although a successful life does not only depend on having desirable sexual relationships, such a relationship may be one of the main determinants of success in marital life. In case a couple’s sexual relationship is not convincing, it can lead to the feeling of disappointment, insecurity, deprivation, reduction of mental health, reduction of marital satisfaction, and family breakdown.
In spite of the improvement of sexual desire in the present study, no significant increase was observed in marital satisfaction. This might be due to the fact that other effective factors in marital satisfaction were not assessed in this study.
Some researchers, such as Nicolson, have expressed that sexual and marital satisfaction in women does not depend on sexual desire. Similarly, Basson indicated that sexual arousal was sometimes possible in women without sexual desire [60].
Sinha et al. mentioned satisfaction with one’s spouse as one of the main factors affecting family performance [61]. On the other hand, dissatisfaction by one’s spouse has been considered to result in reduction of mental health and satisfaction with marital life [62].
Overall, most researchers agree upon the effect of couple’s behavioural and personal characteristics on the positive or negative outcomes of sexual relationships [63]. The couple’s moods and responsibility have also been reported to be associated with marital satisfaction [64,65]. However, this issue was not investigated in the current study. In the study of Velten et al., factors such as “sexual function, sexual distress, frequency of sexual activity, desire discrepancy, sexual initiative, sexual communication, socio-sexual orientation, masturbation” were considered effective in marital satisfaction [66]. Besides, Tao et al. reported that penile-vaginal intercourse In contrast to masturbation and some aspects of non-PVI, partnered sex is the most effective factor for marital satisfaction [67]. All of those factors cannot be considered in our study and as study limitations. Another limitation of this study is that sexual function and satisfaction were only assessed in the women who had referred to health and treatment clinics for receiving services; this decreases the generalizability of the results.
Conclusion
In this study, the intervention was effective in improvement of women’s sexual desire, but had no effects on improvement of their marital satisfaction. Sexual dysfunction is highly prevalent among women and can significantly affect their mental health. Therefore, in addition to consumption of medications, psychotherapy and consultation can also be used to achieve more desirable results.
Competing Interests
The authors declare that they have no known competing interests.
Author’s Contribution
MA and SZ designed the study and MA prepared the first draft of the manuscript. MA and AM and MH D participated in the writing of the final. AM were supervisors and guides on issues related to the dose and the construction of Elaeagnus angustifolia flower capsule and placebo capsules and MS supervised the data analysis.
Financial Support
The study was financially supported by the endocrine and metabolism research center of Vice-chancellor of Shiraz University of Medical Sciences, Shiraz, Iran.
Iranian Registry of Clinical Trial Code
IRCT201212076819N2.
Acknowledgement
The present study was extracted from the research proposal No. 91-01-33-4439 and financially supported by endocrine and metabolism research center, Shiraz University of Medical Sciences, Shiraz, Iran. Hereby, the authors would like to thank endocrine and metabolism research center, Research Vicechancellor of Shiraz University of Medical Sciences, the selected health centers, and all the patients for their kind cooperation in the study. The authors would like to thank Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
References
- Tripoli TM, Sato H, Sartori MG, de Araujo FF, Girão MJ, Schor E. Evaluation of quality of life and sexual satisfaction in women suffering from chronic pelvic pain with or without endometriosis. J Sex Med 2011; 8: 497-503.
- Allendorf K, Ghimire DJ. Determinants of marital quality in an arranged marriage society. Soc Sci Res 2013; 42: 59-70.
- Nezhad MZ, Goodarzi AM. Sexuality, intimacy, and marital satisfaction in Iranian first- time parents. J Sex Marital Ther 2011; 37: 77-88.
- Yoo H, Bartle-Haring S, Day RD, Gangamma R. Couple communication, emotional and sexual intimacy, and relationship satisfaction. J Sex Marital Ther 2014; 40: 275-293.
- Brezsnyak M, Wisman MA. Sexual desire and relationship functioning: the effects of marital satisfaction and power. J Sex Marital Ther 2004; 30: 199-217.
- Litzinger S, Gordon KC. Exploring relationships among communication, sexual satisfaction, and marital satisfaction. J Sex Marital Ther 2005; 31: 409-424.
- Kendler KS, Gardner CO. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am J Psychiatry 2014; 171: 426-435.
- Kingsberg SA1. Attitudinal survey of women living with low sexual desire. J Womens Health (Larchmt) 2014; 23: 817-823.
- Lou WJ, Chen B, Zhu L, Han SM, Xu T, Lang JH, Zhang L. Prevalence and factors associated with female sexual dysfunction in Beijing, China. Chin Med J 2017; 130: 1389-1394 .
- Laumann E, Farrer G, Pan S. Sexual practices and sexual satisfaction: A population base Study of Chinese urban adults. Archiv Sexual Behav 2007; 36: 5-20.
- Safarinejad MR . Female sexual dysfunction in a population-based study in Iran: prevalence and associated risk factors. Int J Impot Res 2006; 18: 382-395.
- Dennerstein L, Koochaki P, Barton I, Graziottin A. Hypoactive sexual desire disorder in menopausal women: a survey of western European women. J Sex Med 2006; 3: 212-222.
- Basson R. Women’s sexual function and dysfunction: current uncertainties, future directions. Int J Impot Res 2008; 20: 466-478.
- Brown AD, Blagg J, Reynolds DS. Designing drugs for the treatment of female sexual dysfunction. Drug Discov Today 2007; 12: 757-66.
- Yoshany N, Morowatisharifabad MA, Mihanpour H, Bahri N, Jadgal KM. The effect of husband’s education regarding menopausal health on marital satisfaction of their wives . J Menopausal Med 2017; 23: 15-24.
- Kleinstäuber M. Factors associated with sexual health and well-being in older adulthood. Curr Opin Psychiatry 2017; 13.
- Hallberg J, Kaldo V, Arver S, Dhejne C, Öberg KG. A cognitive-behavioural therapy group intervention for hypersexual disorder: a feasibility study. J Sex Med 2017; 14: 950-958.
- Allahdadi K, Tostes RCA, Clinton WR. Female Sexual dysfunction: therapeutic options and experimental challenges. Cardiovasc Hematol Agents Med Chem 2009; 7: 260-69.
- Bancroft J. The endocrinology of sexual arousal. J Endocrinol 2005; 186: 411-427.
- Azaizeh H, Saad B, Cooper E and Said O. Traditional Arabic and Islamic medicine, a re-emerging health aid. Evid Based Complement Alternat Med 2010; 7: 419-424.
- Hastings-Tolsma M, Terada M. Complementary medicine use by nurse midwives in the U.S. Complement Ther Clin Pract 2009; 15: 212-219.
- Abedzadeh KM. Complementary and alternative medicine in midwifery. Nursing Midwifery Studies 2014; 3: 19449.
- Mazaro-Costa R, Andersen ML, Hachul H, Tufik S. Medicinal plants as alternative treatments for female sexual dysfunction: utopian vision or possible treatment in climacteric women? J Sex Med 2010; 7: 3695-3714.
- Krychman ML, Gubili MS, Pereira L, Holstein L, Cassileth B. Female sexual enhancers and neutraceuticals. Curr Sexual Health Rep 2007; 4: 177-182.
- Ito TY, Polan ML, Whipple B, Trant AS. The enhancement of female sexual function with ArginMax, a nutritional supplement, among women differing in menopausal status. J Sex Marital Ther 2006; 32: 369-378.
- Amin G. Herbal medicine, the Iranian folkloric drugs. Ministry Health Deputy Res 2001; 101-106.
- Hosseinzadeh H, Rahimi R. Anti-Inflammatory effects of Elaeagnus angustifolia fruits in mice and in rats. Irn J Med Sci 1999; 24: 144-147.
- Çakmakç S, Topdaş E, Kalın P, HanH, Şekerci P, Köse L. Antioxidant capacity and functionality of oleaster (Elaeagnus angustifolia L.) flour and crust in a new kind of fruity ice cream. Int J Food Sci Technol 2015; 50: 472-481.
- Okmen G, Turkcan O. A study on antimicrobial, antioxidant and antimutagenic activities of Elaeagnus angustifolia L. leaves. Afr J Tradit Complement Altern Med 2013; 11: 116-120.
- Chen Q, Chen J, Du H, Li Q, Chen C, Zhang G. Structural characterization and antioxidant activities of polysaccharides extracted from the pulp of Elaeagnus angustifolia L . Int J Mol Sci 2014; 15: 11446-11455.
- Hosseinzadeh H, Ramezani M, Namjo N. Muscle relaxant activity of Elaeagnus angustifolia L. fruit seeds in mice. J Ethnopharmacol 2003; 84: 275-278.
- Si CL, Xu J, Wu L, Hui LF, Liu PT, Liu Z. “Antioxidant flavonoids from bark of Elaeagnus angustifolia”. Plant Med 2009; 75: 943-944.
- Saboonchian F, Jamei R, Hosseini Sarghein S. Phenolic and flavonoid content of Elaeagnus angustifolia L. (leaf and flower). Avicenna J Phytomed 2014; 4: 231-238.
- Oelkeby M, Hedlund P, Albrecht K, Ellinghaus P, Christian SG, Jonas U, Andersson KE. Expression of cAMP and cGMP phosphodiesterase isoenzymes 3, 4, and 5 in the human clitoris: immunohistochemical and molecular biology study. Urol 2006; 67: 1111-1116.
- Uckert S, Ellinghaus P, Albrecht K, Jonas U, Oelke M. Expression of messenger ribonucleic acid encoding for phosphodiesterase isoenzymes in human female genital tissues. J Sexual Med 2007; 4: 1604-1609.
- Cavalcanti AL, Bagnoli VR, Fonseca AM, Pastore RA, Cardoso EB, Paixão JS. Effect of sildenafil on clitoral blood flow and sexual response in postmenopausal women with orgasmic dysfunction. Int J Obstetr Gynaecol 2008; 102: 115-119.
- Rosen RC. Assessment of female sexual dysfunction: Review of validated methods. Fertility Sterility 2002; 77: 80-93.
- Jaafarpour M, Khani A, Khajavikhan J, Suhrabi Z. Female sexual dysfunction: prevalence and risk factors. J Clin Diagn Res 2013; 7: 2877-2280.
- Rostami A, Ghazinour M, Richter J. Marital satisfaction: the differential impact of social support dependent on situation and gender in medical staff in Iran . Glob J Health Sci 2013; 5: 151-164.
- Atis G, Dalkilinc A, Altuntas Y, Atis A, Caskurlu T, Ergenekon E. Sexual dysfunction in women with clinical hypothyroidism and subclinical hypothyroidism. J Sex Med 2010; 7: 2583-2590.
- Kadioglu P, Yalin AS, Tiryakioglu O, Gazioglu N, Oral G, Sanli O. Sexual dysfunction in women with hyperprolactinemia: a pilot study report. J of Urol 2005; 174: 1921-1925.
- Zeinalzadeh S, Akbarzadeh M, Mohagheghzadeh A, Faridi P, Sayadi M. Comparison of the effects of Elaeagnus angustifolia flower capsule and sildenafil citrate tablet on anxiety resulting from sexual dysfunction in women referring to the selected clinics of shiraz university of medical sciences. J Evid Based Complementary Altern Med 2016; 21: 186-193.
- Akbarzadeh M, Zeinalzadeh S, Zolghadri J, Mohagheghzadeh A, Faridi P, Sayadi M. Comparison of Elaeagnus angustifolia extract and sildenafil citrate on female orgasmic disorders: a randomized clinical trial. J Reprod Infertil 2014; 15: 190-198 .
- Karimifar M, Soltani R, Hajhashemi V, Sarrafchi S. Evaluation of the effect of Elaeagnus angustifolia alone and combined with Boswellia thurifera compared with ibuprofen in patients with knee osteoarthritis: a randomized double-blind controlled clinical trial. Clin Rheumatol 2017.
- Niknam F, Azadi A, Barzegar A, Faridi P, Tanideh N, Zarshenas MM. Phytochemistry and Phytotherapeutic aspects of Elaeagnus angustifolia L. Curr Drug Discov Technol 2016; 13: 199-210.
- Giuliano F, Rampin O, Allard J. Neurophysiology and pharmacology of female genital sexual response. J Sex Marital Ther 2002; 28: 101-121.
- Kim NN, Stankovic M, Cushman TT, Goldstein I, Munarriz R, Traish AM. Streptozotocin-induced diabetes in the rat is associated with changes in vaginal hemodynamics, morphology and biochemical markers. BMC Physiol 2006; 6: 4.
- Kang DG, Choi DH, Lee JK, Lee YJ, Moon MK, Yang SN. Endothelial NO/cGMP-dependent vascular relaxation of cornuside isolated from the fruit of Cornus officinalis. Planta Med 2007; 73: 1436-1440.
- Durand S, Davis SL, Crandall CG. Exogenous nitric oxide inhibits: Sympathetically mediated vasoconstriction in human skin. J Physiol 2005; 562: 629-634.
- Konishi M, Su C. Role of the endothelium in dilator responses of spontaneously hypertensive rat arteries. Hypertension 1983; 5: 881-886.
- Heuzé-Joubert I, Mennecier P, Simonet S, Laubie M, Verbeuren TJ. Effect of vasodilators, including nitrice oxide, on the release of cGMP and cAMP in the isolated perfused rat kidney. Eur J Pharmacol 1992; 220: 161-71.
- Vineent SR. Nitric oxide: a radical neurotransmission in the CNS. Prog Neurobiol 1994; 42: 129-160.
- Gray E, Ferrell WR. Acute joint inflammation alters the adrenoceptor profile of synovial blood vessels in the knee joint of rabbits. Ann Rheum Dis 1992; 51: 1129-1133.
- Waldman SA, Murad F. Cyclic GMP synthesis and function. Pharmacol Rev 1987; 39: 163-196.
- Cabral PU, Canario AC, Spyrides MH, Uchoa SA, Eleuterio J, Amaral RL. (Influence of menopausal symptoms on sexual function in middle-aged women) Revista brasileira de ginecologia e obstetricia. Revista da Federacao Brasileira das Sociedades de Ginecologia e Obstetricia 2012; 34: 329-334.
- Ornat L, Martinez-Dearth R, Munoz A, Franco P, Alonso B, Tajada M. Sexual function, satisfaction with life and menopausal symptoms in middle-aged women. Maturitas 2013; 75: 261-269.
- Byers ES. Relationship satisfaction and sexual satisfaction: A longitudinal study of individuals in long-term relationships. J Sex Res 2005; 42: 113-118.
- Auslander BA, Rosenthal SL, Fortenberry JD, Biro FM, Bernstein DI, Zimet GD. Predictors of sexual satisfaction in an adolescent and college population. J Pediatr Adolesc Gynecol 2007; 20: 25-28.
- Basson R. Women sexual dysfunction: Revised and expanded definitions. Synthesis 2005; 172: 1327-1333.
- Nicolson P. What is normal about women sexual desire and orgasm? Soc Sci Med 2003; 57: 1735-1745.
- Sinha SP, Mukerjee N. Marital adjustment and space orientation. J Soc Psychol 1991; 130: 633-639.
- Nock SL. A comparison of marriage and capability relationship. JFI 1995; 16: 53-76.
- Donnellan MB, Conger RD, Bryant CM. The Big Five and enduring marriages. J Res Pers 2004; 38: 481-504.
- Blum JS, Mehrabian A. Personality and temperament correlates of marital satisfaction. J Pers 1999; 67: 93-125.
- Hart SD, Dutton DG, New love T. The prevalence of personality disorder among wife assaulters. J Pers Disord 1993; 7: 329-341.
- Velten J, Margraf J. Satisfaction guaranteed? How individual, partner, and relationship factors impact sexual satisfaction within partnerships. PLoS One 2017; 12: e0172855.
- Tao P, Brody S. Sexual behaviour predictors of satisfaction in a Chinese sample. J Sex Med 2011; 8: 455-460.