Research Article - Current Pediatric Research (2018) Volume 22, Issue 3
Inter-rater variability and validity of the Clinical Assessment of Nutrition Score (CANS) in term newborns.
Aparna Jayaraman*, Sunitha Pazhaniandi, Shobhana SivathanuPaediatrics, ESIC MC& PGIMSR, K.K Nagar, Chennai, INDIA
- Corresponding Author:
- Aparna Jayaraman
Paediatrics, ESIC MC & PGIMSR, KK Nagar, Chennai, India
Tel: 044 2474 8959
Email: drjaparna18@gmail.com
Accepted date: August 09, 2018
Abstract
Aim: To assess the inter-observer reliability and validity of the CANScore (Clinical Assessment of Nutrition Score) compared to other anthropometric parameters namely, Ponderall Index, MAC:HC and BMI. Materials and Methods: Nighty eight term newborns with no medical complications were included. Ponderall Index, MAC:HC (Midarm Circumference to Head Circumference ratio) and BMI (Body Mass Index) were assessed. Two observers applied the CANScore individually on every neonate. At the end of the study, the scores of both the raters were entered in a datasheet and compared statistically. Results: Prevalence of Fetal malnutrition (FM) based on CANSore was ~59% in the study group. Inter-rater reliability of the CANScore was found to be fair to good but not excellent. CANScore had a good sensitivity and specificity compared with BMI (86.2 % and 75% respectively, AUC: 0.853). Conclusion: Inter- observer variability of CANScore is fair to good but not excellent. It has the highest sensitivity and specificity when compared with the BMI. CANScore alone may not accurately assess the fetal malnutrition.
Keywords
CANScore, Inter-rater reliability, Validity
Introduction
The term Fetal Malnutrition (FM) was introduced by Scott and Usher in 1966 to identify malnutrition in the newborn. Many fetal anthropometric indices exist, notably weight for gestational age, Rohrer’s Ponderall Index, Midarm Circumference to Head Circumference ratio (MAC:HC) and neonatal BMI (Body Mass Index). These generally assess Intrauterine Growth Restriction (IUGR) but not fetal nutrition, which specifically refers to muscle mass and adiposity. The Clinical Assessment of Nutrition Score (CANS), developed by Metcoff in 1994 is the most widely used score for assessment of malnutrition in the newborn.
However, being an entirely visual score, there seems to be a wide scope for subjectivity in the assessment.
We conducted the present study primarily to assess the inter-rater reliability of this score and also its validity when compared with other indices like the Ponderall Index (PI), Body Mass Index (BMI) and Mid Arm Circumference to Head Circumference ratio (MAC:HC).
Aim
To assess the inter-rater reliability of CANScore and its validity compared with other anthropometric indices of newborn namely PI, BMI and MAC:HC.
Materials and Methods
This was an observational study conducted at ESIC MC & PGIMSR, Chennai from January 2016-June 2016. CANScore is done as part of the routine assessment of all term newborns. The two raters involved were qualified paediatricians practicing in Paediatrics and Neonatology for the last 10 years. For a 70% probability of agreement between the raters (2 raters) and with an error margin of 20% the sample size calculated was 70 newborns.
A total of 98 neonates born in the hospital were included. Only term newborns (>37 weeks gestational age, by dates and modified Ballard’s score) aged less than 72 hours, with no medical complications or congenital anomalies were included.
The two raters individually did a CANScore on each of the included newborn. The score (Tables 1-3) consists of a total of nine physical parameters-hair, shape of the face, neck fat, subcutaneous fat of the upper limb, the back, buttock, lower limbs, the chest and abdomen.
| Parameter | Malnourished | Prevalence of Malnutrition % |
|---|---|---|
| Weight for gestational age | 3 | 3.1 |
| PI | 17 | 17.4 |
| MAC:HC<0.27 | 16 | 16.3 |
| MAC:HC<0.25 | 3 | 3.1 |
| BMI <11.2 | 24 | 24.5 |
| Rater 1 CANScore | 59 | 60 |
| Rater 2 CANScore | 58 | 59 |
| Average rater CANScore<25 | 63 | 60.2 |
Table 1: Prevalence of malnutrition in the study population based on each anthropometric parameter (n=98)
| Parameter | CANScore | ||
|---|---|---|---|
| Sensitivity % | Specificity % | Score | |
| Weight | 85.3 | 66.7 | 20 |
| PI | 60.7 | 58.6 | 24 |
| MAC:HC | 66 | 68.7 | 22 |
| (<0.27) | |||
| MAC:HC | 86.2 | 75 | 20 |
| (<0.25) | |||
| BMI | 84.3 | 78.6 | 22 |
Table 2: Sensitivity and Specificity of CANScore compared with other anthropometric parameters. (Score refers to the CANScore at which optimum sensitivity and specificity were obtained)
| S.No | Diagnosed Areas | Signs |
|---|---|---|
| 1 | Hair | • Large amount, smooth, silky, easily combed [4] • Thinner, some straight, "staring" hair [3] • Still thinner, more straight, "staring" hair [2] • Straight "staring" hair with depigmented stripe (flag sign) [l] |
| 2 | Cheeks | • Plump, round face [4] • Slightly reduced fat [3] • Significantly reduced [2] • Fat almost absent [1] |
| 3 | Neck and chin | • Double or triple chin, neck not evident [4] • Slightly reduced fat chin, the neck can be seen [3] • Fat pad thin chin, neck revealed [2] • Chin fat disappears, the neck is clear, loose skin, wrinkled [1] |
| 4 | Arm | • Fullness, cannot lift the skin [4] • Arm a little thin, check on the pressure of hands, the accordion-like folds can be formed [3] • Thinner arm, more accordion-like folds [2] • Very little fat, significant accordion- like folds [1] |
| 5 | Back | • Inter-scapular area of skin cannot be picked [4] • Skin can be lifted a little [3] • Easy to lift the skin [2] • Loose skin, easy to lift, wrinkles can form [1] |
| 6 | Buttock | • Full, round gluteal fat pads [4] • Slightly reduced fat [3] • Significantly reduced fat, with wrinkles [2] • Fat disappears, loose skin over upper posterior thigh too [1] |
| 7 | Legs (like arms) | |
| 8 | Chest | • Ribs not visible: Intercostal space full [4] • Intercostal space slightly visible [3] • Prominent ribs [2] • More prominent ribs: Obvious loss of intercostal tissues [1] |
| 9 | Abdomen | • Fullness, thick subcutaneous fat [4] • Slightly reduced fat [3] • Abdominal wall thinning, can form the accordion-like folds [2] • Abdomen boat-shaped, loose skin, can form accordion-like folds [1] |
Table 3: The nine signs for Clinical Assessment of Nutritional status in the newborn
Each of these is graded, the lowest grade for each being 1 and the highest 4. Hence, the maximal and minimal scores possible are 36 and 9 respectively.
Both raters recorded the scores separately. They did not discuss these scores throughout the study period.
Birth weight was measured using a digital infant weighing scale to the nearest 10 g. Length was measured using an infantometer. Mid arm circumference and head circumference were measured using a non stretchable tape.
Ponderall index was calculated using the formula:
Weight in grams/Length in cm3 × 100.
A PI of <2.2 and MAC:HC<0.27 were considered to be indicative of malnutrition. Small, appropriate and Large for Gestational age (SGA, AGA and LGA, respectively) were defined based on intrauterine growth percentile charts.
At the end of the study, the scores from the two raters were entered in the excel sheet. Kappa statistics and Bland Altmann analysis were used for assessing the inter-rater reliability. The results were analysed using SPSS version 21.
Results
A total of ninety-eight (98) newborns were included in the study. 53 (54.1%) of them were male and 45 (45.9 %) female. The average age of the study population was 33.58 hours (SD 20.39 hours).
Mean Weight was 2.96 kg (SD 0.39 kg), the mean length was 49.66 cm (SD 1.63 cm) and the mean Head Circumference was 33.52 cm (SD 1.24 cm).
Rater 1 assigned a score of <25 to 59 of the 98 newborns (60%), classifying them as having FM. Rater 2 assigned a score of <25 to 58 (59%) of the 98 newborns, classifying them as having FM.
The Kappa statistics for the inter-rater reliability was 0.682, indicating a fair to good agreement between the raters.
The raters had fair to good agreement in assessment of the following parameters- hair, face and chest, as evidenced by the Kappa statistic values (0.462 to 0.659).
For the remaining parameters namely neck, arm, back, buttock, leg and abdomen the agreement between the raters was poor with kappa <0.4.
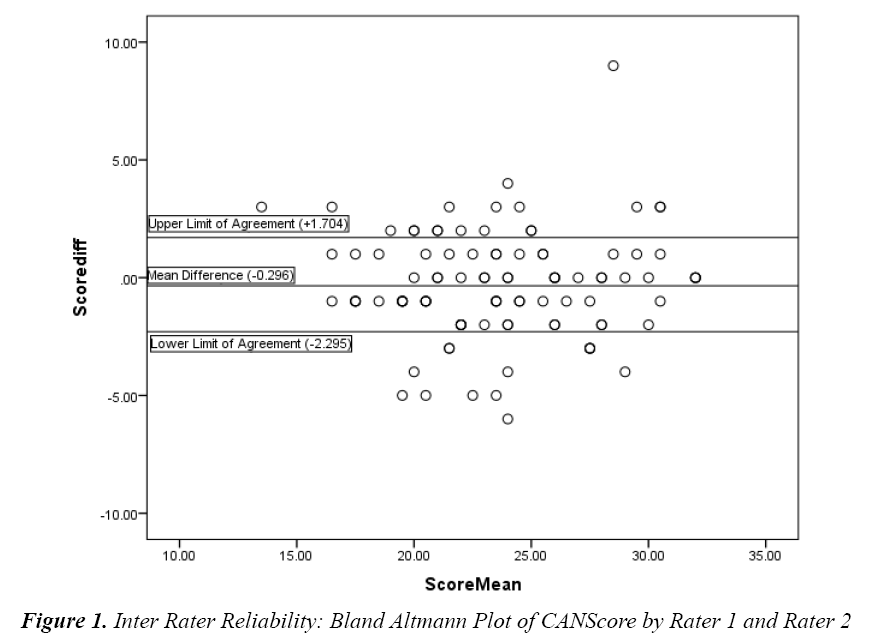
We also did the Bland- Altmann analysis for the scores by the two raters. The mean difference between the scores of the two raters was 0.296, with most values falling within the limits of agreement of -2.295 to +1.704, indicating a fairly good agreement between the raters.
Only 3 of the 98 newborns (6.2%) were Small for Gestational Age (SGA), each of who had a rater average CANScore of ≤20. CANScore had a sensitivity of 85.3% and specificity of 66.7% at a cut off of 20, compared with the weight for gestational age.
17 of the 98 newborns (17.4%) had a PI of <2.2, each of who had a rater average CANScore of <25. The sensitivity and specificity of CANScore compared with a Ponderall Index of 2.2, was highest at a score of 24 i.e. 60.7 and 58.6% respectively.
16 of the 98 newborns (16.3%) had an MAC:HC index of <0.27, indicating moderate malnutrition. Of these, 3 newborns had an index of <0.25 indicating severe malnutrition. The sensitivity and specificity of CANScore compared with MAC:HC of 0.27 was highest at a score of 22, i.e. 66% and 68.7%. (AUC = 0.78). Sensitivity and specificity of CANScore compared with MAC:HC of <0.25 (indicating severe malnutrition) was highest at a score of 20 i.e.86.2% and 75% respectively.
Sensitivity and specificity of CANSCORE compared with a BMI of<11.2, was highest at the score of 22 i.e. 84.3 and 78.6% respectively.
This Bland Altmann Plot shows that the mean difference between the score given by the two raters is -0.296. The Limits of Agreement are -2.295 to +1.704 (Figure 1). Plot shows a substantial portion of the readings within the limits of agreement, indicating a fairly good agreement between the two raters.
Discussion
Scott and Usher introduced the term Fetal Malnutrition (FM), in the 1960s to identify newborns with sub-optimal nutritional status as regards adiposity and muscle mass [1].
Metcoff introduced the Clinical Assessment of Nutrition Score based on nine readily detectable signs. In one of the most important studies, Metcoff et al. demonstrated that Fetal Malnutrition and SGA are not synonymous as ~5.5% of AGA newborns in his study had FM defined by the CANScore ≤ 24 [2].
The most important aspect of our study pertains to the inter-rater reliability of the CANScore in newborns. The Kappa statistic applied to the CANScore by both the raters showed that the inter-rater reliability was fair to good. This was corroborated by the Bland-Altmann analysis, which showed a fairly good agreement between the raters.
The parameters-hair, face and chest had fair to good interrater agreement as shown by the Kappa statistic (0.462 to 0.659) whereas the remaining parameters showed poor interrater agreement (Kappa <0.4).
The inter-rater reliability was however not excellent. This probably can be attributed to the fact that the CANScore is an entirely visual score with a wide scope for subjective differences. This, to some extent undermines its validity. Our study is limited by the small sample size and hence there is a need for more studies with larger sample sizes to ascertain the inter-rater reliability of the CANScore.
To the best of our knowledge, this is the only study assessing the inter-rater reliability of the CANScore. Mehta et al. in their study have mentioned that the inter- rater reliability was excellent but this has not been quantified [3,4].
In our study, we found that among all the anthropometric indices, CANScore had a good sensitivity and specificity compared with BMI (86.2 % and 75% respectively, AUC: 0.853). The CANScore cut-off at this sensitivity and specificity was 22.
In their study, Mahalingam et al. too found that BMI had a good sensitivity and specificity compared with CANScore unlike the PI and MAC:HC [4]. Ahamed and Faheem et al. have demonstrated poor sensitivity with fair specificity of MAC:HC and PI when compared with CANScore in their studies [5,6].
BMI has been found to be a sensitive parameter for assessing nutritional status by Nair et al. in their study [7]. The other advantage of BMI for assessing nutritional status is that it can be used through the life of an individual starting from birth; hence a continuous and comprehensive assessment of nutritional status becomes easy. Recent studies have demonstrated the usefulness of BMI for nutritional assessment even in preterms [8].
More studies, particularly prospective ones, involving all the above scores and indices are needed to better evaluate fetal malnutrition. A recent study on nutritional assessment scores in pancreatic surgery found that none of the scores predicted postoperative complications though pre-operative nutritional status is known to have an impact on the clinical outcome [9,10]. Similarly, to assess fetal malnutrition too, long term follow up studies involving all the available anthropometric indices and nutritional scores are essential. Such studies only can help identify the most sensitive and specific index and its cut- off that is associated with the highest risk of the complications of fetal malnutrition.
Conclusion
The inter-observer reliability of CANScore is fair to good but not excellent. It has the best sensitivity and specificity when compared with the BMI, than with other anthropometric indices like MAC:HC or PI. Using CANscore alone to make a diagnosis of Fetal malnutrition may lead to error. Combining CANScore along with BMI may help in more accurate assessment of fetal malnutrition but more studies are required to confirm the same.
References
- Scott KK, Usher RH. Fetal malnutrition: Incidence, causes and effects. Amer J Obstetr 1966; 94: 951-963.
- Metcoff J. Clinical assessment of nutritional status at birth: Fetal malnutrition and SGA are not synonymous. Pediatr Clin North Am 1994; 41: 875-891.
- Mehta S, Tandon A, Dua T, et al. Clinical assessment of nutritional status at birth. Indian Pediatr 1998; 35: 423-428.
- Soundarya M, Basavaprabhu A, Raghuveera K, et al. Comparative assessment of fetal malnutrition by anthropometry and CAN Score. Iran J Pediatr 2012; 22: 70-76.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3448218/
- Faheem M, Saifuddeen AA. Comparative study of CANSCORE with anthropometry in the assessment of fetal malnutrition. Int J Med Health Sci 2014; 3: 184-189.
- Nair RB, Elizabeth KE, Geetha S, et al. Mid arm circumference (MAC) and body mass index (BMI)–the two important auxologic parameters in neonates. J Tropical Pediatr 2006; 52: 341-345.
- Ezenwa BN, Ezeaka VC. Is canscore a good indicator of fetal malnutrition in preterm newborn. Alexandria J Med 2017; 54: 57-61.
- Zakirhusain S, Pathak R. Revised Kuppuswamy and BG Prasad socio-economic scales for 2016. International J Comm Med & Public Health 2017; 4: 997-999.
- Probst P, Haller S, Bruckner T, et al. Prospective trial to evaluate the prognostic value of different nutritional assessment scores in pancreatic surgery (NURIMAS Pancreas). BJS 2017; 104: 1053-1062.