Research Article - Biomedical Research (2017) Volume 28, Issue 18
General movements and electroencephalogram as a predictive tool of highrisk neonatal neurodevelopmental outcome
Juntan Feng1, Yiyan Ruan1, Qi Cao2*, Yan Chen1, Xiaozhu Liang1
1Department of Pediatrics, Guangxi Women and Children Health Hospital, Nanning, Guangxi, PR China
2Department of Pediatrics, Fifth Affiliated Hospital of Guangxi Medical University, Nanning City, Guangxi, PR China
- *Corresponding Author:
- Qi Cao
Department of Pediatrics
Fifth Affiliated Hospital of Guangxi Medical University, PR China
Accepted on August 7, 2017
Abstract
Background: To investigate the predictive value of General Movements (GMs) and Electroencephalogram (EEG) on high-risk neonatal neurodevelopmental outcome.
Methods: One hundred and ten high-risk new-borns were enrolled in this study. The qualitative general movements were assessed twice and EEG was examined one time within one month after birth. They were given neurological examination to determine whether they suffered from cerebral palsy at the correct age of 1 y old. A comparative analysis of the effect of GMsEEG and GMs+EEG was applied to predict high-risk neonatal neurodevelopmental outcome.
Results: Among the 110 high-risk cases, 38 cases showed abnormal GMs, 72 cases had normal GMs; Abnormal EEG was recorded in 29 cases, while 81 cases showed normal EEG. The sensitivity, specificity, positive predictive value and negative predictive value of qualitative assessment of GMs for predicting high-risk neonatal neurodevelopmental outcome were 83.87%, 84.81%, 68.42% and 93.06% respectively. For EEG, the sensitivity, specificity, positive predictive value and negative predictive value were 70.97%, 91.14%, 75.86% and 88.89% respectively. For GMs+EEG, the sensitivity, specificity, positive predictive value and negative predictive value were 90.48%, 95.45%, 86.36% and 96.92%.
Conclusions: Both the qualitative assessment of GMs and EEG examination can be used to predict highrisk neonatal adverse neurodevelopmental outcome. Combining GMs with EEG examination is instrumental in improving the predictive effect on high-risk neonatal neurodevelopmental outcome.
Keywords
Nervous system malformations, Cerebral palsy, General movements, Electroencephalogram, Psychomotor disorders.
Introduction
With the development of medical technology, the survival rate of new born is greatly improved. According, long-term neurodevelopmental disability rate of high-risk new-born is increased, such as Cerebral Palsy (CP), which is the major disability. The central nervous system is the most plastic at young age. So, early detection, accurate diagnosis and offering appropriate and timely intervention can offer an opportunity for suffered children a [1].
Prechtl's GM assessment technique was introduced in the early 1990s to predict neurodevelopmental impairments. General Movements (GMs), spontaneous movement patterns, show the variable movements of neck, arms, legs and trunk. The intensity and speed of GMs change when the nervous system is damaged. It is usually used to predict brain dysfunction.
Studies showed that fidgety movements improved our ability to predict later neurodevelopmental outcomes in term born children with neonatal hypoxic ischemic encephalopathy. Abnormal, absent, or sporadic fidgety movements indicate an increased risk for later neurological dysfunction, whereas normal FMs are highly predictive of normal development.
The analysis of GMs was also used to predict later neurodevelopmental outcome for new-borns [2-4]. Electroencephalogram (EEG) records the spontaneous brain activities from patients, which is associated with behavior, cognition and consciousness. It is widely used to examine and predict abnormal nervous system in clinics and laboratories [5].
Studies also showed that neonatal EEG surveillance exhibited a good specificity and a good positive likelihood ratio for neurodevelopmental outcomes in very preterm infants assessed at 2 y of corrected age [6].
In this study, we enrolled high-risk new-borns and analysed the sensitivity, specificity of GMs, EEG and GMs with EEG in predicting neonatal neurodevelopmental outcome.
Materials and Methods
Clinical material
This prospective cohort study was conducted in Third Affiliated Hospital of Guangxi Medical University. The study was approved by clinical ethics committee of Third Affiliated Hospital of Guangxi Medical University. One hundred and ten high-risk new-borns were enrolled in this study from 2012 January to 2013 June, including 71 males and 39 females. For gestational age (w), 65 cases were in 28-37 w. 35 cases were in 37-40 w. 10 cases were more than 40weeks. Etiology diagnosis included premature delivery (65 cases), ubependymal hemorrhage (SHE) (25 cases), asphyxia (22 cases), Hypoxic Ischemic Encephalopathy (HIE) (11 cases), hypoglycemia (11 cases), cerebral injury (6 cases), Intracranial Hemorrhage (ICH) (5 cases), purulent meningitis (5 cases), bilirubin encephalopathy (2 cases), neonatal seizures (2 cases), neuro syphilis (2 cases) and periventricular leukomalacia (1 case).
Inclusion criteria and exclusion criteria
Inclusion criteria included new-borns with cerebral injury, such as premature delivery, asphyxia, ICH, HIE and hyperbilirubin encephalopathy. Exclusion criteria were that the new-born was diagnosed inherited metabolic disease and the last menstrual period of mother's is not clear.
General movements
GMs assessment was examined in one month after delivery for two times. The internal was at least one week. Ten to twenty min video recording was made of the spontaneous motility of each infant. The infant was in the supine position in the warm boxes. The diapers should be removed from premature infants to decrease the restriction.
The recording was made during periods of active wakefulness, and crying, agitating, feeding and persistent hiccups were avoided. The video recordings were evaluated by two paediatricians, who received GMs assessment training.
General movements included twisting motion stage and unease motion stage. The performance of each stage is different. In twisting motion stage, the performance included normal, PR (Poor Repertoire) and CS (Cramped-Synchronized). In unease motion stage, it included normal and F-(Absent fidgety movement). For predicting cerebral palsy, we calculated the positive predictive value, and negative predictive value, sensitivity and specificity of poor repertoire, crampedsynchronized and absent fidgety movement.
Electroencephalogram
EEG was also examined at the same day of GMS assessment. Electroencephalograph (NT9200-H, Beijing Xintuo) was used to record EEG. Disc electrode 16 guide was placed according to international 10/20 system. The two ear electrodes were used as reference electrodes. To make sure that at least one complete wakefulness-active sleep-quiet sleep period was monitored, the time of collection was 2-3 h. High Shelf was set as 30 Hz, time constant was 0.1 s and sensitivity was 10 μv/mm. Characteristics of background activities (discontinuous figure, alternate figure or continuous figure) and the corresponding brain waves on both sides of the cerebral hemisphere (spike waves, sharp waves, θ waves and δ waves were recorded.
Gesell developmental scale assessment
The development quotient (DG) of different functional areas, including strength exercises, fine moment, language, adaptive behavior and social behavior were calculated.
Statistics analysis
All statistical analyses were conducted using 17.0 SPSS. Chi-square test was used to analyse the count data. Significance for the analyses was set at P<0.05.
Results
Among the new-born at the corrected age of 1 y old, there were 4 cases (3.64%) of cerebral palsy, 27 cases (24.55%) of psychomotor developmental retardation and 79 normal cases (71.82%) (Table 1). For predicting cerebral palsy, the positive predictive value of poor repertoire, cramped-synchronized and absent fidgety movement was 2.9%, 50% and 75% respectively. The negative predictive value of poor repertoire, cramped-synchronized and absent fidgety movement was 96%, 98.1% and 99% respectively. The sensitivity was 25%, 50% and 75% respectively. The specificity was 68.9%, 98.1% and 99%. For predicting psychomotor developmental retardation, the positive predictive value of poor repertoire, crampedsynchronized and absent fidgety movement was 64.7%, 25% and 25% respectively. The negative predictive value was 93.4%, 75.5% and 75.5% respectively. The sensitivity was 81.5%, 3.8% and 3.7% respectively. The specificity was 85.5%, 96.4% and 96.4% respectively (Table 2).
| Twisting motion stage | Unease motion stage | ||||
|---|---|---|---|---|---|
| Normal | PR | CS | Normal | F- | |
| Cerebral palsy | 1 (1.4) | 1 (2.9) | 2 (50) | 1 (0.9) | 3 (75) |
| Psychomotor developmental retardation | 5 (6.9) | 22 (64.7) | 1 (25) | 27 (25.5) | 1 (25) |
| Normal | 66 (91.7) | 11 (32.4) | 1 (25) | 78 (73.6) | 0 (0) |
| Total | 72 (100) | 34 (100) | 4 (100) | 106 (100) | 4 (100) |
| PR: Poor Repertoire; CS: Cramped-Synchronized; F-: Absent Fidgety Movement. | |||||
Table 1. Predictive values of GMs in different stages on high-risk neonatal neurodevelopmental outcome (N=110) (%).
| Cerebral palsy | Psychomotor developmental retardation | |||||
|---|---|---|---|---|---|---|
| PR | CS | F- | PR | CS | F- | |
| Positive predictive value | 2.9 | 50 | 75 | 64.7 | 25 | 25 |
| Negative predictive value | 96 | 98.1 | 99 | 93.4 | 75.5 | 75.5 |
| Sensitivity | 25 | 50 | 75 | 81.5 | 3.8 | 3.7 |
| Specificity | 68.9 | 98.1 | 99 | 85.5 | 96.4 | 96.4 |
| PR: Poor Repertoire; CS: Cramped-Synchronized; F-: Absent Fidgety Movement. | ||||||
Table 2. The sensitivity, specificity, positive predictive value and negative predictive value of qualitative assessment of GMs in different stages on high-risk neonatal neurodevelopmental outcome.
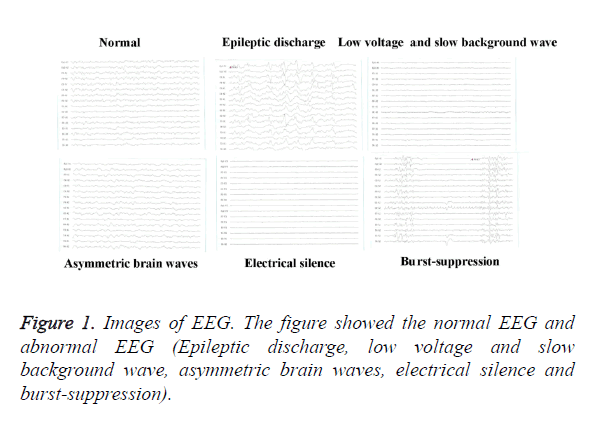
Among the 110 high-risk cases, 38 cases showed abnormal GMs, 72 cases had normal GMs; Abnormal EEG was recorded in 29 cases, while 81 cases showed normal EEG (Table 3). The abnormal EEG included epileptic discharge, low voltage and slow background wave rate, asymmetric brain waves, electrical silence and burst-suppression (Figure 1). The sensitivity, specificity, positive predictive value and negative predictive value of qualitative assessment of GMs for predicting high-risk neonatal neurodevelopmental outcome were 83.87%, 84.81%, 68.42% and 93.06% respectively. For EEG, The sensitivity, specificity, positive predictive value and negative predictive value were 70.97%, 91.14%, 75.86% and 88.89% respectively. For GMs+EEG, The sensitivity, specificity, positive predictive value and negative predictive value were 90.48%, 95.45%, 86.36% and 96.92% (Table 4).
| GMs | EEG | GMs+EEG | ||||
|---|---|---|---|---|---|---|
| Normal | Abnormal | Normal | Abnormal | Normal | Abnormal | |
| Cerebral palsy | 0 (0) | 4 (10.5) | 0 (0) | 4 (13.8) | 0 (0) | 4 (18.2) |
| Psychomotor developmental retardation | 5 (6.94) | 22 (57.9) | 9 (11.1) | 18 (62.1) | 2 (3.07) | 15 (68.2) |
| Normal | 67 (93.1) | 12 (31.6) | 72 (88.9) | 7 (24.1) | 63 (96.9) | 3 (13.6) |
| Total | 72 (100) | 38 (100) | 81 (100) | 29 (100) | 65 (100) | 22 (100) |
| GMs: General Movements; EEG: Electroencephalogram. | ||||||
Table 3. Predictive values of GMs and EEG on high-risk neonatal neurodevelopmental outcome (N=110) (%).
| Examination methods | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|
| GMs | 83.87% (26/31) | 84.81% (67/79) | 68.42% (26/38) | 93.06% (67/72) |
| EEG | 70.97% (22/31) | 91.14% (72/79) | 75.86% (22/29) | 88.89% (72/81) |
| GMs+EEG | 90.48% (19/21) | 95.45% (63/66) | 86.36% (19/22) | 96.92% (63/65) |
| GMs: General Movements; EEG: Electroencephalogram. | ||||
Table 4. The sensitivity, specificity, positive predictive value and negative predictive value of qualitative assessment of GMs and EEG in predicting high-risk neonatal neurodevelopmental outcome.
Discussion
Brain damage for new-borns is easily to be misdiagnosed, because some new-borns have no obvious clinical feature or it is attributed to immature development. In fact, Central nervous system is the most plastic at young age. So, timely intervention can offer an opportunity for suffered children. General Movements (GMs) are spontaneous movement patterns for fetus and neonate. The movements firstly appear at 9 w of pregnancy and last into five to six months after birth. According to the developmental process, GMs include stage before full term, twisting motion stage and unease motion stage. The normal motion for stage before full term and twisting motion stage is the variable movements of neck, arms, legs and trunk. New-borns are in these stages. If Poor Repertoire (PR) and Cramped-Synchronized (CS) appear in this stage, we should pay more attention to it. During unease motion stage, absent fidgety movement is abnormal.
The intensity and speed GMs always change when the nervous system is damaged, so GMs are effective in assessing the function of nervous system for infants. It is widely used to make early identification for cerebral palsy and other movement disorders [7,8]. In this study, we found that the sensitivity, specificity, positive predictive value and negative predictive value of qualitative assessment of GMs for predicting high-risk neonatal neurodevelopmental outcome were 83.87%, 84.81%, 68.42% and 93.06% respectively. Studies showed that qualitative assessment of GMs were not same. Yang et al. reported that positive predictive value, the negative predictive value, the sensitivity and specificity of qualitative assessment of GMs in stage before full term and twisting motion stage were 50%, 95%, 83% and 78% [9]. Gong et al.’s study showed that positive predictive value, the negative predictive value, the sensitivity and specificity of qualitative assessment of GMs in predicting cerebral palsy were 70%, 94.1%, 87.5% and 84.2, which was consistent with our results [10]. Sustersic et al. reported that GMs in twisting motion stage for premature infant, the sensitivity in predicting nerve damage was 86% and the specificity for term infant was 24% and the specificity in three month was 21%, which was lower than present results [11].
The GMs of different stages have different prediction value. We found that CS and F- have higher positive predictive value, the negative predictive value, the sensitivity and specificity than PR. F- was also higher than CS in positive predictive value, the negative predictive value, the sensitivity and specificity. The results were consistent with other reports [12]. Sustersic et al. found that GMs in twisting motion stage for premature infant, the sensitivity in predicting nerve damage was 86%, while it is 100% s in unease motion stage. F- has a high prediction value [11]. Ferrai et al.’s study showed that PR had low prediction value, while CS specifically predicted cerebral palsy. PR, which concentrated on monotonicity of the movement, and reflected mental status [13]. CS shows stiffness of the movement and synchronous spasm. F- shows lack of subtle movement. So CS and F can be used to predict cerebral palsy.
For predicting psychomotor developmental retardation, we found that there was no difference between CS and F-. However, the positive predictive value, the negative predictive value, the sensitivity and specificity for PR were higher than CS and F-, which was similar to Beccaria’s study [14].
EEG is a very important toll to predict brain damage for new-borns. It is widely used to assess the development of brain and brain dysfunction. The functional damage for brain is prior to the damage of brain structure [15]. Abnormal EEG for newborns includes 1) abnormal background activities, such as lack of variability, electrical silence, low voltage, burst suppression and out of synchron; 2) paroxysmal abnormality, such as single rhythmic discharge, focal discharge and multiple locals discharge; 3) abnormal sleep structure and maturity, such as the change of sleep structure and delayed maturity [16,17]. The background activities of EEG give higher predicted value in assessing brain function and prognosis. The typical abnormality includes delayed maturity, lack of variability, low voltage, burst suppression, which suggests poor prognosis for neurodevelopment. Wong et al. also reported that abnormal EEG, especially abnormal background, had a poor prognosis [18]. In our study, the positive predictive value, the negative predictive value, the sensitivity and specificity for EEG in predicting outcome for neurodevelopment were 75.86%, 88.9%, 70.97, 91.14%, which suggested that EEG also had a higher value in predicting neurodevelopment for new-borns.
Our results showed that there was no obvious difference between GMs and EEG in predicting neurodevelopment, including the positive predictive value, the negative predictive value, the sensitivity and specificity. Studies showed that GMs preferred to predict nerve damage of movement dysfunction, such as cerebral palsy [19]. In our study, we found that the combination of GMs and EEG had higher the positive predictive value, the negative predictive value, the sensitivity and specificity than GMs or EEG alone. In other words, GMs and EEG can complement each other in predicting neurodevelopment. If both GMs and EEG remind poor neurodevelopment, timely prevention should be done to reduce the burden of the family and the society.
Conclusion
In conclusion, we found that GMs and EEG can be used to predict neurodevelopment for high-risk new-borns. Combination GMs and EEG has a higher positive predictive value, the negative predictive value, the sensitivity and specificity than GMs and EEG alone. For predicting cerebral palsy using GMs, CS and F- have higher positive predictive value, the negative predictive value, the sensitivity and specificity than PR. For predicting psychomotor developmental retardation, PR is a better indicator than CS and F-. Early diagnosis and timely intervention will offer an opportunity for suffered children.
Acknowledgements
This study was supported by Self-raising funded research subject of Guangxi health department Z2012200.
Competing Interests
None
References
- Giovanni C, Giulia D, Andrea G. Perinatal brain damage in children: Neuroplasticity, early intervention, and molecular mechanisms of recovery. Prog Brain Res 2011; 189: 139-154.
- Einspieler C, Prechtl HF. Prechtls assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment Retard Dev Disabil Res Rev 2005; 11: 61-67.
- Hamer EG, Bos AF, Hadders-Algra M. Assessment of specific characteristics of abnormal general movements: does it enhance the prediction of cerebral palsy? Dev Med Child Neurol 2011; 53: 751-756.
- Soleimani F, Badv RS, Momayezi, Biglarian, Marzban. General movements as a predictive tool of the neurological outcome in term born infants with hypoxic ischemicencephalopathy. Early Hum Dev 2015; 91: 479-482.
- Fingelkurts A, Bagnato S, Boccagni C, Galardi G. Prognostic value of resting-state electroencephalography structure in disentangling vegetative and minimally conscious states: a preliminary study. Neurorehabil Neural Repair 2013; 27: 345-354.
- Périvier M, Roze JC , Gascoin G ,Hanf M, Branger B, Rouger V, Berlie I, Montcho Y, Péréon Y, Flamant C, Nguyen The Tich S. Neonatal EEG and neurodevelopmental outcome in preterm infants born before 32 weeks. Arch Dis Child Fetal Neonatal Ed 2016; 101: 253-259.
- Mutlu A, Livanelioglu A, Korkmaz A. Assessment of general movements in high-risk infants by prechtl analysis during early intervention period in the first year of life. Turk J Pediatr 2010; 52: 630-637.
- Adde L, Helbostad JL, Jensenius AR, Taraldsen G, Grunewaldt KH, Støen R. Early prediction of cerebral palsy by computer-based video analysis of general movements: a feasibility study. Dev Med Child Neurol 2010; 52: 773-778.
- Yang H, Shi W, Shao XM. Study of predictive validity and reliability of qualitative general movement’s assessment for neurological outcome in high risk neonates. China J Evid Based Pediat 2007; 2: 172-180.
- Gong CD, Yang H, Shi W, Wang Y, Shao X, Christa E, Wang W. Significance of prechtls qualitative general movements assessment (GMs) and brainstem auditory evoked potential (BAEP) in predicting of cerebral palsy. Chinese J Child Health Care 2011; 19: 403-405.
- Sustersic B, Sustar K, Paro-Panjan D. General movements of preterm infants in relation to their motor competence between 5 and 6 years. Eur J Paediatr Neurol 2012; 16: 724-729.
- Einspieler C, Marschik PB, Bos AF, Ferrari F, Cioni G, Prechtl H. Early markers for cerebral palsy: Insights from the assessment of general movements. Fut Neurol 2012; 7: 709-717.
- Ferrari F, Cioni G, Einspieler C. Cramped synchronized general movements in preterm infants as an early marker for cerebral palsy. Arch Pediatr Adolesc Med 2002; 156: 460-467.
- Beccaria E, Martino M, Briatore E. Poor repertoire General Movements predict some aspects of development outcome at 2 years in very preterm infants. Early Hum Dev 2012; 88: 393-396.
- Jin HZ, Huang DM, Guan XJ. Practical neonatology (3 Ed). Peoples Med Publ H, Beijing 2002; 297-405.
- Li JM, Wu BQ. Progress of application and features of electroencephalogram in neonates. J Appl Clin Pediatr 2007; 22: 145-147.
- Douglass LM, Wu JY, Rosman NP, Stafstrom CE. Burst suppression electroencephalogram pattern in the newborn: predicting the outcome. J Child Neurol 2002; 17: 403-408.
- Almubarak S, Wong PK. Long-term clinical outcome of neonatal EEG findings. J Clin Neurophysiol 2011; 28: 185-189.
- Bosanquet M, Copeland L, Ware R, Boyd R. A systematic review of tests to predict cerebral palsy in young children. Develop Med Child Neurol 2013; 55: 418-426.