Research Article - Journal of Trauma and Critical Care (2017) Volume 1, Issue 1
Femoral neck fractures in the elderly: from risk factors to pronostic features for survival.
Santiago Luis Iglesias*, Luciano Gentile, Fernando Vanoli, Martin Marcelo Mangupli, Ignacio Pioli, Riikka EK Nomides, Bartolome Luis AllendeAllende Institute for Reconstructive Surgery of Members, Allende Sanatorium, Cordoba, Argentina
- *Corresponding Author:
- Santiago Luis Iglesias
Allende Institute for Reconstructive Surgery of Members
Allende Sanatorium
Argentina
Tel: 54 9 2302464499
E-mail: santiglesias07@hotmail.com
Accepted Date: June 26, 2017
Citation: Iglesias SL, Gentile L, Vanoli F, et al. Femoral neck fractures in the elderly: from risk factors to pronostic features for survival. J Trauma Crit Care. 2017;1(1):16-21
Abstract
Introduction: Proximal femur fracture is one of the more serious health problems that affect patients of advanced age. Few studies have reported the risk factors associated with increased mortality after arthroplasty for a femoral neck fracture in the elderly. The purpose of this study was to identify preoperative prognostic factors associated with survival probability and increased length of survival after hemiarthroplasty or total hip arthroplasty (THA) in elderly patients for femoral neck fracture. A secondary objective of this study was to perform a riskbenefit analysis of arthroplasty type on complication rate and patient survival. Materials and Methods: A retrospective, observational and descriptive study. Data was gathered from the medical records of all patients aged 60 years and older who underwent hemiarthroplasty or THA for a femoral neck fracture at our institution from 2010-2015. Data was supplemented by telephone interviews when necessary. Results: The average survival time was 33.9 months for THA and 19.07 months for hemiarthroplasty. Nineteen percent of study patient were deceased at final follow-up, with no difference in gender. Risk of mortality increased by 25% with increased age. The risk of mortality was 7 times greater in the group that underwent hemiarthroplasty. The presence of comorbidities diminish the likelihood of survival in patients subjected to hip surgery. This decrease was significantly greater after hemiarthroplasty, even when adjusting for age of the patient. There was no association between prosthesis and functional characteristics and quality of life post-operatively. Conclusions: The mean survival of patients undergoing hip surgery was less than 3 years and is influenced by the presence of comorbidities. The risk of mortality was significantly greater when the type of prosthesis is a hemiarthroplasty, even when adjusting for patient age. The quality of life after surgery was not related with the type of surgical procedure.Keywords
Femoral neck fracture, Arthroplasty, Comorbidities
Introduction
Proximal femur fracture is one of the more serious health problems that affects the elderly [1]. This population often has comorbidities that not only prolong recovery after surgery, but also increase the risk of post-operative morbidity and mortality [2]. The reported 30-day mortality rate after femoral neck fracture in the elderly is approximately 9.6% and increases to approximately 30% at one year. However the exact rate varies and may depend on fracture pattern, prior functional status, and baseline health prior to injury [3-5].
The combination of physiological age and wellbeing plays an important role in determining the likelihood of mortality after hip fracture. In this context, the term “fragility” is multifactorial and refers to the patient’s energy level, physical ability, cognition and general health. Patients that are fragile are more vulnerable to adverse events, such as post- operative complications and prolonged hospital stay, and increased mortality after surgery for a hip fracture [2,6].
Although femoral neck fracture in the elderly is known to be highly morbid, few studies have reported on conditions associated with increased mortality and morbidity after arthroplasty for femoral neck fracture in this high-risk population. In elderly patients that underwent surgery with multiple cannulated screws, hemiarthroplasty or total hip arthroplasty, Patel et al. [2] found 6 comorbidities in all three groups that independently modified mortality rates: functional mobility, pulmonary disease, renal insufficiency, malignancy, thyroid disease and altered mental status. Miller et al. found that age, body mass index (BMI), previous functional status, and early surgery were risk factors [4].
The Garden and Pauwel’s classifications have remained the mainstay for characterizing femoral neck fractures and guiding surgical treatment [7]. Nondisplaced fractures (Garden I and II) are generally managed with preservation of the hip, whereas displaced fractures (Garden III and IV) are typically treated with arthroplasty [4]. In mobile patients of advanced age, hemiarthroplasty or total hip arthroplasty (THA) are the treatments of choice. Hemiarthroplasty (unipolar or bipolar) is the most common, however THA is preferred in certain active elderly patients. The optimal option is still controversial; although THA results in improved function and pain relief, it also increases surgical time and blood loss, both of which enhance the risk of mortality [5].
Our hypothesis is that patients suffering from a fracture of the femoral neck have an increased risk of death after this event, and that presenting co-morbidities such as hypertension, cardiac disease, diabetes, renal insufficiency, mental illness and smoking are at a higher risk than those who not present.
The overall objective of this study was to identify and evaluate factors associated with survival and the length of survival from surgery until death in patients who underwent hemiarthroplasty or THA from 2010-2015 at our institution for femoral neck fracture. A secondary objective was to perform a risk-benefit analysis on the type of arthroplasty (hemi- vs total) in relation to complications and mortality.
Materials and Methods
A retrospective, observational and descriptive study was conducted. In this study, “elderly” was defined as patients 60 years of age and older [2]. The information was gathered from the medical records of all elderly patients aged 60 years and older who underwent hemiarthroplasty or THA at our institution between 2010 and 2015 for femoral neck fracture. These data were supplemented by telephone interviews when necessary. All patients were treated by the same surgical team (4 surgeons). Inclusion criteria were: patients of both sexes ≥ 60 years of age with a femoral neck fracture surgically treated with hemiarthroplasty or total hip arthroplasty between 2010 and 2015.
Exclusion criteria therefore were established as: patients under 60 years of age, patients with pathological fractures of the femoral neck and patients treated with multiple cannulated screws. A total of 107 patients (88 females, 19 males) with a mean age of 77.8 years were included in the study. The comorbidities evaluated were hypertension, cardiac disease, diabetes, renal insufficiency, mental illness and smoking.
Post-operative health status was analyzed using the EuroQol-5D questionnaire [8], which quantifies mobility, ability to complete activities of daily living, pain and depression. Age, gender, comorbidities, Garden classification, type of prosthesis (hemi- or total) and ASA class were recorded [9-13].
Results
Forty-four patients underwent hemiarthroplasty and 63 underwent THA. There were no patients with an ASA class of I, 62 were class II, 42 were class III and 3 were class IV. The average time to surgery was 1.5 days (0 - 10 days) and mean hospital stay was 6 days (0-17 days). The analyzed comorbidities were: hypertension (75 patients), cardiac disease (26 patients), diabetes (23 patients), renal insufficiency (11 patients), mental illness (13 patients) and smoking (40 patients).
Table 1 shows the sampling distribution of survival, by sex, of the 107 patients. For 19% of patients who died, no significant differences between sexes were observed (21% of men and 19% of women respectively; p=0.844).
Table 1. Survival distribution by gender (2010-2015).
| Survival | Male Female | Total | |
|---|---|---|---|
| Alive | 23 | 63 | 86 |
| Deceased | 6 | 15 | 21 |
| Total | 29 | 78 | 107 |
Table 2 shows the statistical summary of survival time (months) and age (years), by gender. It also presents, for reference, the values of the main percentiles (10, 30, 70 and 90) for both variables. Mean survival did not exceed 30 months (28.63 months, EE 2.12 months), however, both survival and age did not differ by sex (p=0.689 and p=0.252, respectively). In addition, it is noteworthy that the homogeneity observed in the percentile of survival by sex, except for the men and the 10th percentile, the value of which was zero (10% of the sample of men had no months of survival). Since age was similar between men and women, the overall risk of death was estimated. Thus, the relative risk of death related to age was equal to 1.25 (95% CI: 1.31 – 1.37, p<0.01), indicating that as age increased, the risk of death increased by 25% and does not differ between sexes.
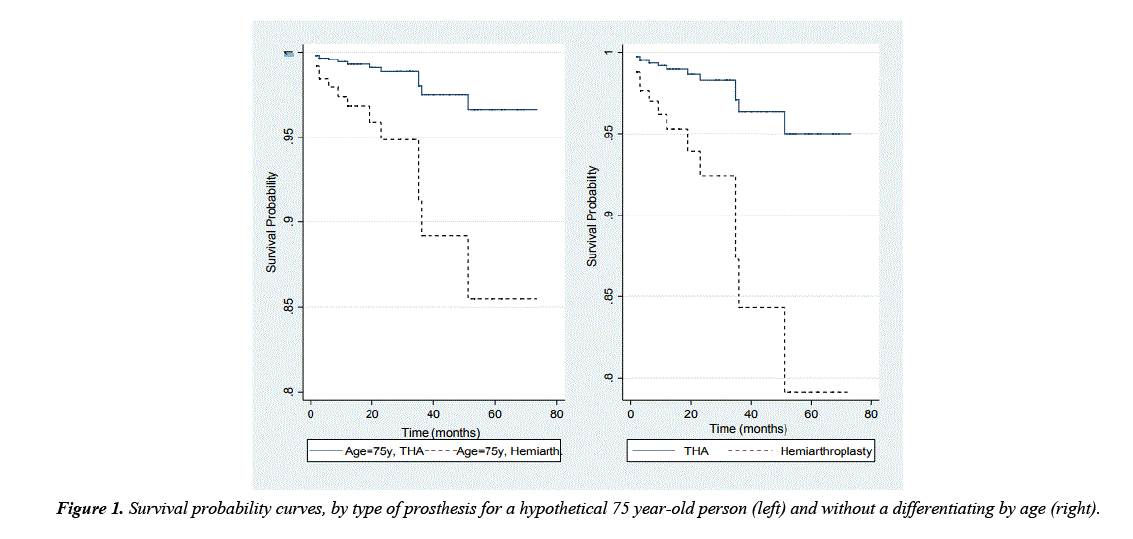
Mean age and survival was analyzed by sex and prosthesis type Table 2. Survival of patients that received a hemiarthroplasty was significantly lower than those that underwent THA (THA: mean 34.61 months, SE 2.5; hemi: mean 20.04 months, SE 2.6; p<0.05). However, when analyzed separately by gender, similar means of survival timesafter hemiarthroplasty vs. THA was observed in men (p=0.12) whereas a significant difference was obtained in women (p<0.05). When adjusting for age and sex, the relative risk of mortality for those receiving hemiarthroplasty was 7.24 (95%CI: 1.21 – 23.26, p<0.05). In other words, the risk of mortality was 7 times greater after hemiarthroplasty than after THA. Figure 1 illustrates differences between estimated probability of survival by prosthesis at age 75 years (which was 40% of the study population).
Table 2. Summary statisitics: mean, standard error (EE), and percentile (P) of survival (months) and age of patients, by sex (2010-2015).
| Men | ||||||
|---|---|---|---|---|---|---|
| Variables | Mean | SE | P10 | P30 | P70 | P90 |
| Survival (months) | 27.31 | 4.04 | 0 | 12 | 36 | 59 |
| Age (years) | 75.72 | 2.45 | 57 | 70 | 81 | 88 |
| THA/Hemiarthroplasty Survival (months) Age (years) |
||||||
| 31.75/17.44 | 3.32/2.34 | |||||
| 73.5/80.1 | 2.01/2.7 | |||||
| Women | ||||||
| Survival (months) | 29.11 | 2.40 | 2.00 | 12 | 40 | 61 |
| Age (years) | 78.53 | 2.10 | 66 | 72 | 82 | 89 |
| THA/Hemiarthroplasty Survival (months) Age (years) |
||||||
| 35.95/20.71 | 3.1/2.65 | |||||
| 73.88/84.23 | 1.12/0.52 | |||||
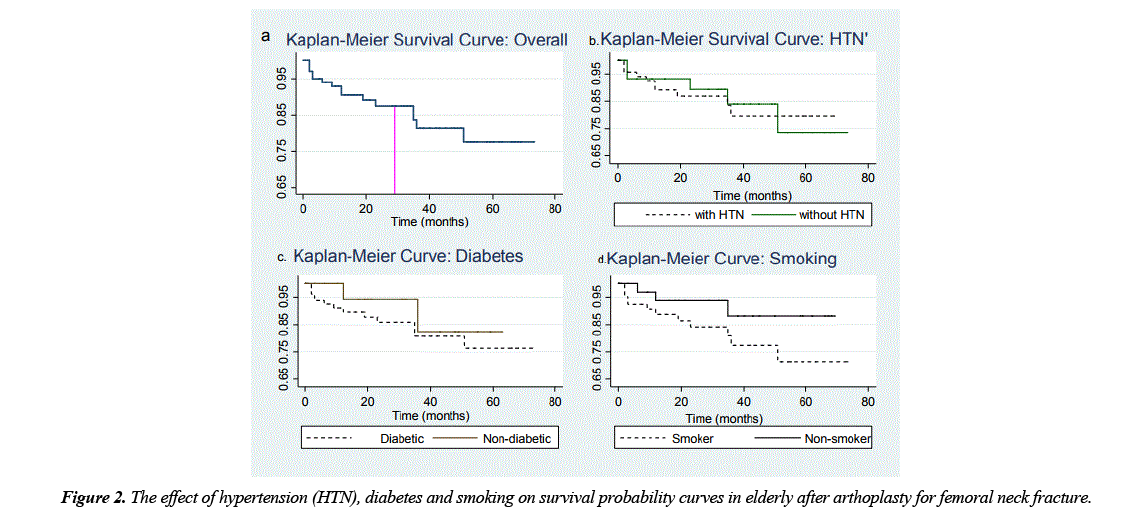
Kaplan-Meier survival curves were performed for (a) all patients, (b) those with hypertension (HTN) vs. without, (c) diabetics vs. non-diabetics and (d) smoker vs. non- smoker (Figure 2). The overall probability of survival at 29 months after surgery (average time estimated in this sample) was 88%, indicating that the risk of not surviving was greater than 12%. When this chance was evaluated considering comorbidities, the survival probability decreased strongly for HTN and diabetes (p=0.036 and p=0.08, respectively) as compared to those without the disease. Similarly, probability of survival is significantly reduced in patients who smoke as opposed to nonsmokers (Figure 2d).
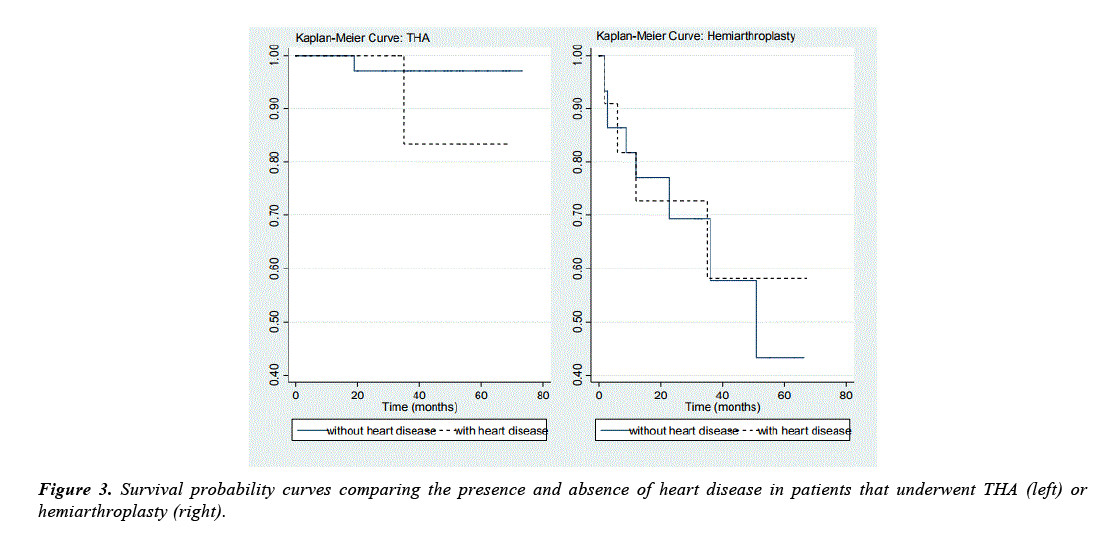
Survival times were not significantly different between patients with heart disease and those without (mean 30.70 months, SE 3.76 and mean 27.95 months, SE 2.43, respectively). Nor was there a difference in survival by gender (p=0.745). When modeling the probability of survival (adjusted for age), however, the relative risk of those with heart disease was 3.36 time greater than those without heat disease (95%CI: 1.05–17.39). This difference was even more profound when combined with the type of prosthesis (Figure 3).
In patients that underwent hemiarthroplasty, heart disease status increased risk of mortality by 9.40 times (95%CI: 1.64– 16.07, p=0.032), related to those who underwent THA and had no heart disease. The results were similar in patients with HTN and diabetes, though milder. Thus, the risk of death in patients with HTN or diabetes after hemiarthroplasty was significantly greater compared to those without HTN or diabetes and underwent THA (HTN: RR 4.45, p=0.033; Diabetes: RR 5.57, p=0.080).
Table 3 shows summary statistics for co-morbidities. Survival time was significantly lower after hemiarthroplasty, even when adjusting for patient age.
Table 3. Summary statistics of survival (months) by collected co-variables (2010- 2015).
| Variable* | Mean | Standard Error | N |
|---|---|---|---|
| HTN | |||
| 0 | 34.52 | 3.96 | 32 |
| 1 | 26.12 | 2.35 | 75 |
| Diabetes | |||
| 0 | 28.93 | 2.34 | 84 |
| 1 | 27.21 | 4.33 | 23 |
| Heart Disease | |||
| 0 | 27.95 | 2.32 | 81 |
| 1 | 26.00 | 1.23 | 26 |
| Smoking | |||
| 0 | 30.12 | 2,41 | 67 |
| 1 | 27.73 | 3.74 | 40 |
| ASA | |||
| 0 | 28.46 | 2.69 | 62 |
| 1 | 28.84 | 3.20 | 45 |
| Anemia | |||
| 0 | 30.07 | 2.25 | 78 |
| 1 | 30.20 | 6.45 | 15 |
Note: *0 = absent, 1 = present
The survival probability was also assessed by grouping ASA class category (1-2 vs. 3-4) and assessing for the complications related to anemia, such as requirement for transfusion or not (Table 3). Both characteristics showed no statistically significant difference between their categories (p=0.928 and p=0.983, respectively).
When analyzing the length of hospital stay, we can conclude that the length of survival (months) had no statistically significant relations (p=0.752) with days elapsed from admission to surgery.
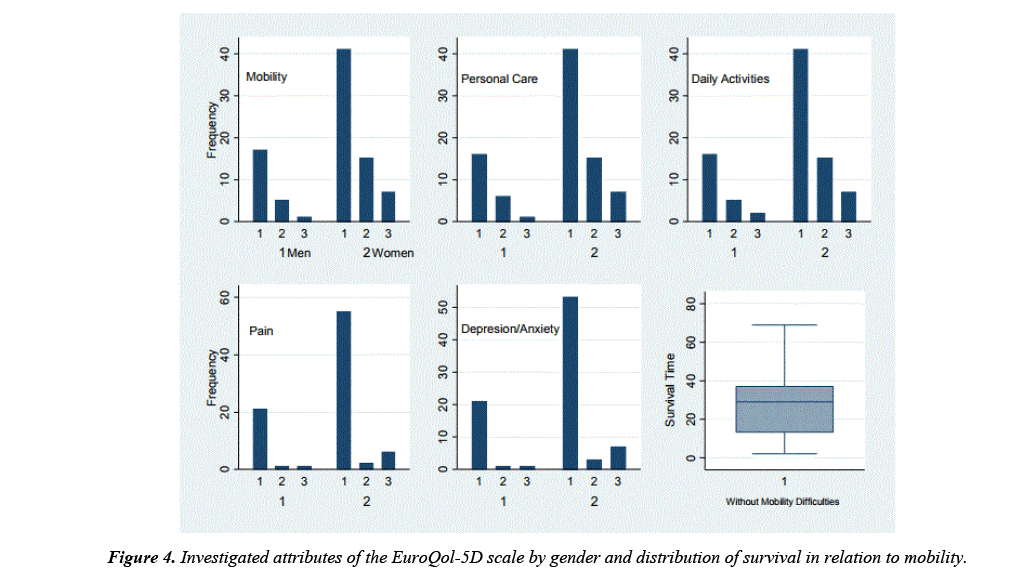
Mobility, self-care, activities of daily living, pain and mental health (specifically, anxiety and depression) were investigated as surrogates of quality of life using the EuroQol-5D questionnaire (Figure 4). All indicators had similar performance by gender as regards of the frequency of severity from mild or ‘without problem’ (categorized as 1) to extreme (category 3), in which ‘without problem’ was the most frequent response (Figure 4). ‘Without problem’ was also the most commonly selected response when stratified by type of prosthesis received (p=0.342).
Furthermore, each of the measures had similar mean survival times (months) were similar (p=0.759), namely: 29.39 (mobility), 30.23 (personal care), 29.84 (activities of daily living), 31.11 (pain) and 31.10 (depression/anxiety).
It is noteworthy that in the remaining categories of each variable of the EuroQol scale, the mean survival was greater. Taking the second category for example (those that presented in the second order of magnitude) in which patients had “some problems” with mobility, activities of daily living, personal care, moderate pain and moderate depression or anxiety had mean survival of 39.3, 37.3, 36.9, 44.7 and 48.1 months respectively.
Discussion
This study is one of the few analysis in the literature which assesses the risk factors associated with survival in patients with femoral neck fractures treated surgically with total hip arthroplasty (THA) or hemiarthroplasty. Our results demonstrated that 19% of patients who suffer a femoral neck fracture had a decreased survival rate to 30 months, indicating that femoral neck fracture, as an event, worsens the prognosis of survival in patients of advanced age.
Not only is hip fracture known to be one of the most serious health problems affecting elderly patients, but these patients often have preexisting comorbidities that augment the risk of morbidity and mortality [1,14,15]. Yet one aspect that is limited in the literature is the evaluation of the preoperative factors that influence the choice of treatment with hemiarthroplasty or total hip replacement [4].
An overall mortality rate of 20% to 30% is reported in the majority of the literature in patients that suffer a femoral neck fracture [3-5]. The present study reported a mean survival of 29 months and of the 19% of patients in this study who were deceased on follow-up, there was no difference by gender. In contrast, Diamond et al. [16] reported that men of advanced age who presented with a femoral neck fracture had a greater rate of mortality than women. Of note, the results of the present study were that 10% of study patients lived less than 2 months after hip fracture and 32% lived less than one year. Fransen et al. [17] reported that femoral neck fractures in men implied a greater risk of death or being institutionalized within 2 years after the fracture.
Our results also demonstrated that the risk of death increased by 25% as age increased, with no differences between sexes. Butler et al. [13] in their review of the literature demonstrated that age, gender, cognitive impairment and functional capacity prior to injury were associated with mortality rate. This was affirmed by Erickson et al [3], who found that 90% of the deaths in their population occurred in patients greater than 75 years of age.
In this study, the survival in patients who underwent hemiarthoplasty were significantly less than those who were treated with total hip arthroplasty. The patients undergoing hemiartoplasty are older than patients with THP. They also have more comorbidities that increase the risk of death. Miller et al. [4] found no significant differences between the mortality rates at 30 days with respect to either surgical option, but did consider that predictive factors for a hemiarthroplasty were age greater than 80 years, low body weight, functional dependence, renal insufficiency and hemiplegia.
This study also found that the probability of survival was significantly decreased In the presence of a comorbidity, diabetes and HTN being the most common but cardiac disease being associated with the lowest mean survival (26.0 months). Miller et al. [4] reported that only cancer and diabetes were predictive of having a complication but that sex, age, dependent functional status, dyspnea, preoperative sepsis, pneumonia, preoperative blood transfusion or renal insufficiency after hemiarthroplasty or THA were not. Radcliff et al. [10] however defined predictors of mortality as Caucasian race, advanced age, metastatic malignancy, mental deterioration, cardiac insufficiency, functional dependence prior to fracture and ASA grade – but not the type of prosthesis.
The present study did not find a significant association between post-operative complications and ASA grade. However, other publications [18] reported a greater utilization of blood transfusions in patients that had a total hip replacement (22.7%) versus a hemiarthroplasty (14.4%). This likely represents increased blood loss associated with preparation of the acetabulum during THA [4]. The risk of post-surgical complications is influenced by patient factors rather than type of procedure, however, patients that undergo THA have greater risk of requiring a blood transfusion in the immediate postoperative period [14].
Shiga et al., in their review of the literature on delay to surgery after hip fracture concluded that a delay of greater than 48 hours is associated with a medium and long- term increase in risk of mortality in elderly with hip fractures [19,20]. In the present study, however, no statistically significant difference was found in patient survival with respect to length of time from admission until surgery. However, it is important to consider that in the study population, the average length of time until surgery was 1.5 days, i.e., less than the 48 hour cutoff in the aforementioned study. In regard to the type of prosthesis, the association between this, patient function and post- operative quality of life were not significant. Burgers et al. [16] in their meta-analysis concluded that although THA for femoral neck fractures could lead to superior results per patient perspective, more randomized clinical trials were needed to provide strong evidence of quality of life in patients after one or the other surgery.
Conclusion
Femoral neck fracture can be considered a predisposing event of length of survival in patients of advanced age, since our results reflected a mortality rate of 32% at one year after femoral neck fracture. On the other hand, the presence of comorbidities diminish the chance of survival in patients undergoing hip surgery and this decrease was significantly more pronounced after hemiarthroplasty, even when adjusting for age. Finally, quality of life after surgery was not related to type of surgical procedure (hemi- or total arthroplasty).
References
- Lizaur UA, Serna BR, Lopez-Prats FA, et al. Early rehospitalization after hip fracture in elderly patients: Risk factors and prognosis. Arch Orthop Trauma Surg. 2015;135(12):1663-1667.
- Patel KV, Brennan KL, Brennan ML, et al. Association of a modified frailty index with mortality after femoral neck fracture in patients aged 60 years and older. Clin Orthop Relat Res. 2014;472(3):1010-1017.
- Erickson BJ, Nwachukwu BU, Kiriakopoulos E, et al. In-hospital mortality risk for femoral neck fractures among patients receiving medicare. Orthopedics. 2015;38(7):593-596.
- Miller CP, Buerba RA, Leslie MP. Preoperative factors and early complications associated with hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures. Geriatr Orthop Surg Rehabil. 2014;5(2):73-81.
- Maceroli MA, Nikkel LE, Mahmood B, et al. Operative mortality after arthroplasty for femoral neck fracture and hospital volume. Geriatr Orthop Surg Rehabil. 2015;6(4):239-245.
- Lowe JA, Crist BD, Bhandari M, et al. Optimal treatment of femoral neck fractures according to patient’s physiologic age: an evidence-based review. Orthop Clin North Am. 2010 ;41(2):157-66.
- Florschutz AV, Langford JR, Haidukewych GJ, et al. Femoral neck fractures: Current management. J Orthop Trauma. 2015;29 (3):121-129.
- Herdman M, Badia X, Berra S. El EuroQol-5D: A simple alternative for the measurement of the quality of life related to health in primary care. Primary Health Care. 2001;28(6):425-430.
- American Society of Anesthesiologists. Relative value guide. 2010.
- Cox DR. Regression models and life-tables. Journal of the Royal statistical Society B. 1972;34:187-220.
- Kalbeisch JD, Prentice RL. The statistical analysis of failure time data. John Wiley & Sons, Inc., New York. 1980.
- Royston P, Parmar MKB. Flexible parametric proportional hazards and proportional odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Statistics in Medicine. 2002;21(15):2175-2197.
- Skrondal A, Rabe-Hesketh S. Generalized latent variable modeling: Multilevel, longitudinal and structural equation models. Chapman & Hall, Boca Raton, FL. 2004.
- Radcliff TA, Henderson WG, Stoner TJ, et al. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90:34-42.
- Butler M, Forte ML, Joglekar SB, et al. Evidence summary: Systematic review of surgical treatments for geriatric hip fractures. J Bone Joint Surg Am. 2011;93:1104-1115.
- Diamond TH, Thornley SW, Sekel R, et al. Hip fracture in elderly men: prognostic factors and outcomes. Med J Aust. 1997;167(8): 412-415.
- Fransen M, Woodward M, Norton R, et al. Excess mortality or institutionalization after hip fracture: Men are at greater risk than women. J Am Geriatr Soc. 2002;50(4):685-690.
- Liodakis E, Antoniou J, Zukor DJ, et al. Major complications and transfusion rates after hemiarthroplasty and total hip arthroplasty for femoral neck fracture. J Arthroplasty. 2016;31(9):2008-2012.
- Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55(3):146-154.
- Burgers PT, Van Geene AR, Van den Bekerom MP, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: A meta-analysis and systematic review of randomized trials. Int Orthop. 2012;36 (8):1549-1560.