Research Article - Biomedical Research (2018) Volume 29, Issue 12
Fall risks factors among home-based health care patients in the Aseer province: Observational study
Faisal Y. Asiri1*, Adel Alshahrani2, Mohamed Faia Aseeri3, Mohammed Mehtab Alam1, Sabri M. Ataalla3, Mohammad A. AlMohiza4 and Irshad A. Abdulhamed1
1Department of Medical Rehabilitation Sciences, College of Applied Medical Sciences, King Khalid University, Abha, Saudi Arabia
2Department of Medical Rehabilitation Sciences, College of Applied Medical Sciences, Najran University, Najran, Saudi Arabia
3Home Health Care, Ministry of Health, Kingdom of Saudi Arabia
4Department of Medical Rehabilitation Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia
- *Corresponding Author:
- Faisal Y. Asiri
Department of Medical Rehabilitation Sciences
College of Applied Medical Sciences
King Khalid University, Abha, Saudi Arabia
E-mail: fasiri@kku.edu.sa
Accepted on May 21, 2018
DOI: 10.4066/biomedicalresearch.29-18-654
Visit for more related articles at Biomedical ResearchAbstract
Purpose: To describe the prevalence of fall risks factors using the Missouri Alliance for Home Care’s fall risk assessment tool (MAHC-10) on home-based health care (HHC) patients in the Aseer region, southern Saudi Arabia. Also, to highlight the process of care, and physical therapy utilization among home health care beneficiaries.
Method: 242 patients’ information were retrieved and reviewed. Patients in our study received various healthcare services including physical therapy, nursing and physicians’ visits between October and December 2017. We used the MAHC-10, which was designed for assessing multifactorial fall risks among home-based health care patients.
Results: 43% of patients were male, and 57% were female. Males received care within an average of 8 d of a referral date, whereas female patients received care within an average of 15 d. Majority of patients are functionally dependent (78%) of patients. Nursing visits were the highest number of professionals that provided HHC visits for both patients’ risk groups. The impairment of functional mobility had the highest fall risk factor among patients receiving HHC services, and fall history factor was the lowest prevalent fall risk factor among patients.
Conclusion: Health care utilization is very important, and it should start early enough to decrease the risk of fall especially physical therapy visits. The level of functional mobility was also a most prevalent factor across all home health care patients in our study, and it is an essential element for predicting the likelihood of a fall in the older adult Aseer population.
Keywords
Fall risks, Home health care, Physical therapy.
Introduction
The consequences of falls are a serious public health burden as they put a huge burden on health care and health care costs, and older people are more susceptible to suffering a fall. It becomes a major health issue for people who are 65 y of age or older, where up to 40% of community-dwelling elderly people have suffered a fall [1,2]. Regarding fall-related injuries, around 10% of falls result in serious injury to the elderly, such as a hip fracture, any other forms of fracture, hematoma, head trauma, and a variety of other injuries that require hospital care; also, 95% of hip fractures in older adults are due to falls that increase the risk of disability. Unfortunately, hip fractures can eventually lead to moving to a nursing home for longerterm care, usually for the rest of the person’s life [3].
Falls are a very serious problem because they are the 5thleading cause of death [4]. In the United States, every 15 s a patient arrives in an emergency room because of a fall, and every 30 min an elderly American dies because of a fall [2]. The definition of a fall is “unintentionally ending up on the ground or other lower level not because of fainting, sudden illness, the act of man, or act of nature” [5]. Around 35% of adults over the age of 65 and 50% of adults over the age of 80 have a fall each year [6]. Falls affect the quality of life and independence of an individual, significantly. More than half of those who suffer a fall experience decreased social and physical activity, while 15% of this population are seriously restricted in their mobility, and quality of life is compromised [3].
In Saudi Arabia, the population of older people is expected to have doubled by 2020; this will lead to the increase of 4% to 7% of the elderly making up the population. This means the number of people likely to experience a fall will increase if we do not apply the proper tools, which can predict the risk of falls for older patients so the number of incidents can be minimized [7].
As a consequent of a fall, the possibility or risk of ending up in a nursing home is very high, and most people do not prefer that as an option. People who have fallen before may well have already developed a gait and balance problem, have vision or cognitive impairment, have medical issues such as diabetes, incontinence, dizziness, depression, dementia, arthritis, or pain, or who may already take up to four different medicines a day, and are at high risk of falling again. The chance of a fall will rise as the number of these ailments increases. Tinetti studied a cohort of older people living in the community to establish the prevalence of risk factors for falls. They found that around 10% has no risk of falling and around 80% had four and more risk factors, which meant they had a greater possibility of falling [8].
Regarding the location of a fall, 56% of falls happened outside the home, such as on the street or in a public place. On the other hand, falls that occurred inside the home represented around 40%, usually happening in the bedroom or dining room [9].
As clinicians, we can help in reducing the risk of a fall by reducing the factors that increase the risk. This can be done through several methods, such as the person having regular exercise and physical therapy, medication reviews, regular check-ups and implementation of home safety measures [10-12].
Physical therapy plays an important role in decreasing the possibility of a fall through multiple approaches. One of these is a therapeutic exercise, which is challenging for people who are not used to it. However, exercise can improve muscle power, enhance balance and improve quality of life. Any form of exercise that improves muscle power and endurance will eventually improve balance and reduce the risk of a fall [13,14].
There is several assessment tools described and referred to in literature that measure fall risks and predict the likelihood of a fall in an older adult population. One of these tools is the Missouri Alliance for Home Care’s fall risk assessment tool- MAHC-10, which was designed for assessing multifactorial fall risks among home-based health care patients. The MAHC-10 was developed by the Missouri Alliance for Home Care Fall Preventive Initiative. The tool was tested and validated among the home-based health care population [15]. The main goal of the measure is to help home health care professionals to improve their patients’ outcomes and to reduce the number of falls. The MAHC-10 has fulfilled the requirements to meet OASIS-C criteria for a multifactorial, standardized, validated assessment form for home-based health care to provide clinicians with an easy method to evaluate fall risks. The MAHC-10 is an assessment form that gives home health care clinicians an evidence-based method to address fall risk for older home-based health care patients. It is a standardized and multifactorial tool that measures ten elements for each patient [15].
Little research has been done on fall risks among elderly members of the community in Saudi Arabia. This research aims to measure the prevalence of fall risks using MAHC-10 on home-based health care patients in the Aseer region, southern Saudi Arabia. The elements of this form include recording the person’s age, co-morbidities, and fall history, level of incontinence, number of drugs taken, visual impairment, impaired functional mobility, environments hazards, cognitive impairment, and pain. We will describe the prevalence of these risk factors, the process of care (timing of initiation of care), and physical therapy utilization. Examining fall risk factors and describing their elements is very important in providing better care to prevent falls and related injuries among home-based health care patients.
Methods
In this study, we reviewed 242 medical records of patients who received home-based health care services in the Aseer province, Saudi Arabia. The patients received HHC services and received the benefit of various healthcare services including physical therapy, nursing, and physicians’ visits. Data were retrieved from 23 home health care centres across the Aseer province. We selected patients who received the service between October and December 2017. The medical records in our study included patients’ characteristics (demographics, clinical, and health status) at the start of care and information obtained from the MAHC-10 tool. The patients’ records were de-identified by an honest broker and were sent to the King Khalid University to perform our research analysis.
The MAHC-10 is a valid and comprehensive single multifactorial tool that can identify fall risk for patients receiving home-based health care services. This tool assessed ten elements, as discussed, and the total scores ranged from 0 to 10, where 0 represented the least likelihood of a patient having a fall, and 10 represented that a patient was at the highest risk of having a fall. From the 10 elements in this tool, 4 elements correlated with fall incidence, which were: fall history for the previous 3 months, functional mobility, three-ormore co-existing diagnoses, and pain. From these 4 factors, a noticeable fall history is a primary factor.
It has been suggested that a score of 4 or more for the MAHC-10 is considered as a person having a high risk of fall. This tool has high sensitivity with 97% and low specificity with 13.3%. However, depending on the use of this tool, the cut-off value can be increased. With a cut-off of 6, the sensitivity is 69%, and specificity is 47%. So, a cut-off score of 6 might identify those patients with high fall risk. In our study, we used a cut-off of 4 for categorizing patients in the analysis section.
Results
242 patients received home-based health care services in the Aseer province’s HHC setting between October and December 2017. 43% of patients were male, and 57% were female. According to age group prevalence, patients between 75-85 y of age were the highest group with 34%, followed by 28% of patients who were 85 and above years of age, and 22% of patients were less than 65 y of age (Table 1). According to timely initiation of care for patients, males received care within an average of 8 d of a referral date, whereas female patients received care within an average of 15 d, an average of 22 d for patients aged between 75-85 y of age, and patients under 65 y of age received care within an average 10 d (Table 1). Regarding activities as a part of daily living (ADL), 70% of patients in our studies were dependent, 22% were independent, 4% needed aids equipment, and 3% needed assistance in their daily living activities (Table 1).
| Information | N (%) |
|---|---|
| Gender | |
| Male | 103 (42.6%) |
| Female | 139 (57.4%) |
| Age group | |
| Less than 65 | 52 (21.5%) |
| 65-75 | 40 (16.5%) |
| 75-85 | 82 (33.9%) |
| 85-Above | 68 (28.1%) |
| Timely initiation of care | |
| Gender | |
| Male | 8 d |
| Female | 15 d |
| Age group | |
| Less than 65 | 10 d |
| 65-75 | 5 d |
| 75-85 | 22 d |
| 85-above | 6 d |
| Type of service | |
| Physical therapy | 147 (60.7%) |
| Nursing | 235 (97.1%) |
| Social | 53 (21.9%) |
| Palliative care | 11 (4.5%) |
| Activities of daily living | |
| Aids | 9 (3.7%) |
| Bedridden | 1 (0.4%) |
| Dependent | 169 (69.8%) |
| Independent | 52 (21.5%) |
| Needs aids in ADLS | 1 (0.4%) |
| Needs assistance | 7 (2.9%) |
| Partially dependent | 3 (1.2%) |
| Fall risk category | |
| Low risk | 43 (18.1%) |
| High risk | 194 (81.9%) |
| HHC: Home Health Care. | |
Table 1. Demographic information of patients receiving HHC in the Aseer province.
When describing the distributions of total scores on the MAHC-10 tool, patients who had a score of 4 were the highest percentage (20%) among all patients, followed by a score of 5 in 17% of patients. More details related to the MAHC-10 tool distributions are described in Table 2. Based on the numbers of total visits of physicians, physical therapists and nurses by total scores, nurse’s visits were the highest number of professionals that provided HHC visits for both patients risk groups. The fall risk group was divided into two categories, low risk-those who were less likely to suffer a (who got 3 or less for their MAHC-10 score) and high risk-those who were more likely to suffer a fall (who got 4 or more for their MAHC-10 score). Patients with a high risk of falling made up 82% of the total number of patients in our study and only 18% of patients were in the low-risk category.
| Total scores | N | % |
|---|---|---|
| 0 | 1 | 0.004 |
| 1 | 5 | 0.021 |
| 2 | 18 | 0.074 |
| 3 | 20 | 0.083 |
| 4 | 49 | 0.202 |
| 5 | 40 | 0.165 |
| 6 | 39 | 0.161 |
| 7 | 33 | 0.136 |
| 8 | 26 | 0.107 |
| 9 | 7 | 0.029 |
| MAHC-10: The Missouri alliance for home care fall risk assessment tool. | ||
Table 2. Distribution of total scores on the MAHC-10 tool.
In Table 3 we have shown the number of the health care professionals’ visits according to patient risk category; low-risk patients had more nurses’ visits (29%), followed by physicians’ visits (24%), and fewest visits from physical therapists (12%). In high-risk patients, the numbers of visits by nurses were also the highest at 23% of patients, then physicians’ visits (21%) and again the fewest visits were from physical therapists (16%).
| Fall risk category | Physicians visits | Physical therapy visits | Nursing visits |
|---|---|---|---|
| (Mean, SD) | (Mean, SD) | (Mean, SD) | |
| Low risk patients (N=43) | 24 ± 17.7 | 12 ± 22.3 | 29 ± 21.3 |
| High risk patients (N=194) | 21 ± 18.8 | 16 ± 23.6 | 22 ± 18.5 |
Table 3. Number of health care professional visits based in the fall risk category.
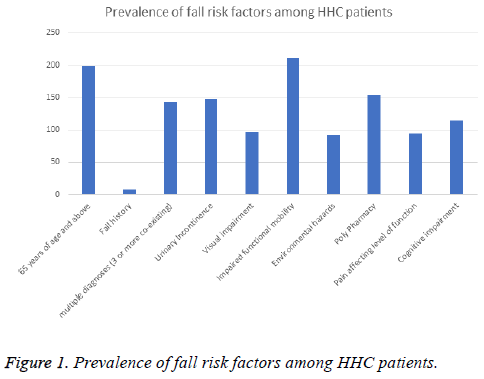
In Figure 1, we explained the overall distributions of fall risk factors in the MAHC-10 tool, including age, number of diagnoses, fall history, incontinence, and level of vision, functional mobility, environment, medication, cognition, and pain. The level of functional mobility was also a most prevalent factor across all home health care patients in our study and fall history factor was the lowest prevalent fall risk factor among patients.
Discussion
Although HHC services in Saudi Arabia are targeting all age groups, including children, elderly people represent 79% of total patients in our study. The most prevalent fall risk factors in our study were impaired functional mobility, followed by increasing age (above 65 y of age). This underlined the nature of our patients who were dependent on mobility or who required assistance to remain actively mobile. Regarding the timely initiation of care, male patients received their care within an average of 8 d of a referral date, while female patients received HHC services within an average of 15 d. The variance in days between males and females was due to cultural barriers that require caregivers’ availabilities.
Health care utilization, especially physical therapy services, is essential in reducing the number of falls and to improve the quality of home-based health care services. In our research, physical therapy appeared to have been underutilized, which was contradicted by the literature that emphasizes the importance of physical therapy interventions [5]. Physical therapists paid the fewest number of visits of all health care professionals for both low-risk and high-risk patients.
In this study, we utilized the MAHC-10 to identify patients who are at risk for fall. Several factors in MAHC-10 were suggested in the literature that has a major impact on falls; these were increasing age, number of illness diagnoses, fall history, incontinence, vision impairment, functional mobility limitations, environmental hazards, multiple medications, cognition impairment, and pain [15]. Most of these factors are consistent with the elements in the MAHC-10 that we utilized in our study. We described in our study the prevalence of these factors in patients receiving home-based health care services in the Aseer province (Figure 1). Level of functional mobility is considered as the most prevalent fall risk factor among our patients, and it underlines their dependency in mobility.
Medication management, which is one of the elements in the MAHC-10, may well help by eliminating the use of certain drugs and this should decrease the likelihood of the risk of a fall. If the patient takes four or more different medicines, the risk of a fall will rise. However, if the number of different medications taken decreases from four to two (under strict medical supervision), the possibility of a fall will decrease from 80% to 30% [1]. In our study, 63% of patients took four or more medicines, which means greater attention needs to be paid to drugs’ side effects (e.g., dizziness, fainting, etc.) and consultation would be advised to review the medicines taken.
Also Hazards relating to a patient’s immediate environment occurred with 38% of patients in our study. Home safety is very important for people who have fallen more than once. Taking care there is adequate lighting, electrical cords are kept out of the way, and removal of loose rugs is all very important measures. Moreover, bathroom safety is critical in the home environment. Grab rails, non-slip matting in a shower, non-slip flooring (carpet as opposed to ceramic tiling) and proper bathroom lighting can make a huge difference in preventing or minimizing fall hazards [3].
Older people need to have a regular medical check-up. This includes checking vision, joints and muscles, brain and cognitive function, feet, appropriate footwear, etc. which will have an impact on MACH-10 score. When there is a visual deficit, the correction will decrease the risk of a fall. Joints and muscles play an important role because elderly people suffer from arthritis and pain, plus associated physical weakness that all contribute to increasing the risk of falling. Moreover, foot examination and proper shoes can have a huge impact on balance and reduce the risk of a fall.
Fall history is one of the crucial elements that can predict the likelihood of falls among older people. Calys et al. addressed the importance of fall history as one fall in a 3-month period greatly increases the risk of another fall in the near [15]. They concluded that this is one of the most important factors for predicting the likelihood of falls. Although the prevalence of fall history in our study is 3%, it is necessary to educate clinicians and patients about the clear definition of a fall. According to the World Health Organization (WHO), a fall is defined as “inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest in furniture, wall or other objects”. This clear definition prevents any misinterpretations of a fall by clinicians or patients [16].
In literature, gait performance is considered as one of the strongest predictors of a fall, and mortality [17,18]. Also, it is the 6th (functional) vital sign, and every geriatric clinic should address this when examining older adults [19]. Gait speed or velocity has been shown in the literature to be a reliable and valid measure to predict the likelihood of a fall among older adults [17,19]. The functional mobility element in the MAHC-10 fall risk assessment tool is not specific for measuring gait speed and characteristics (e.g., stride length, step length, etc.). It is very important to add gait speed as one of the screening processes along with the MAHC-10 fall risk assessment tool when assessing older patients receiving homebased health care services.
There are several limitations in our study. One of these is the nature of the study design, which is a retrospective design. Heterogeneousness of diagnostic groups of patients might also limit the generalization of results to a specific group of patients. Also, we included in our study only patients that were still recipients of HHC, which automatically included a number who were receiving long-term help. Future studies must address these concerns and to assess the overall outcomes of a rehabilitation program on fall risks and falls among older adult people. Also, it is important to examine the short-term and long-term effects of rehabilitation on decreasing the likelihood of falls among the diagnostic groups.
Describing the prevalence of fall risk factors using MAHC-10 across HHC settings will provide clear insights into the nature of patients' health status, which is necessary to enhance the quality of care delivered to patients in their homes. However, we had limited information for some settings to make effective comparisons. Also, variations in timely initiation of care (how long the initiation of the process of patient care usually takes) among age groups might relate to heterogeneousness of medical conditions and comorbidities. Future studies should describe patient’s diagnoses and comorbidities along with other factors that might affect the care process. Also, future studies should address the rehabilitation program (supervised) designed for preventing falls in older adults. A supervised and standardized rehabilitation program dedicated to fall prevention may give us valuable and accurate information to help in minimizing the incidence of falls among the older adult Aseer population.
Conclusion
Health care utilization is very important, and it should start early enough to decrease the risk of a fall, especially through regular physical therapy visits. In our study, physical therapy was the least-used professional service, yet it is the most important care element when it comes to reducing the risk of a fall among older adults. Fall history should be taken into account since it can provide an indicator of the likelihood of a further fall among elderly people. The level of functional mobility was also a most prevalent factor across all home health care patients in our study, and it is an essential element for predicting the likelihood of a fall in the older adult Aseer population.
Conflicts of Interest Disclosures
The researchers claim no conflicts of interest.
References
- Rao SS. Prevention of falls in older patients. Am Fam Physician 2005; 72: 81-88.
- Stevens JA, Corso PS, Finkelstein EA. The costs of fatal and non-fatal falls among older adults. Injury Prevention 2006; 12: 290-295.
- Stevens JA, Olson S. Reducing falls and resulting hip fractures among older women. Home Care Provider 2000; 5: 134-141.
- Bergland A, Wyller TB. Risk factors for serious fall related injury in elderly women living at home. Injury Prevention 2004; 10: 308-313.
- Feder G, Cryer C, Donovan S. Guidelines for the prevention of falls in people over 65. Brit Med J 2000; 321: 1007.
- Leclerc BS, Bégin C, Cadieux É. A classification and regression tree for predicting recurrent falling among community-dwelling seniors using home-care services. Canadian J Public Health/Revue 2009; 263-267.
- Alsenany S. Student nurses attitudes and knowledge towards the care of older people in Saudi Arabia. Generation Rev Newsl Br Geriatrics Soc 2009.
- Tinetti ME, Speechley M, Ginter SF. Risk Factors for fall among elderly persons living in the community. New England J Med 1988; 319: 1701-1707.
- Campbell A, Borrie MJ, Spears GF. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 1990; 19: 136-141.
- Josephson KR, Fabacher D, Rubenstein L. Home safety and fall prevention. Clin Geriatr Med 1991; 7: 707-731.
- Blake A, Morgan K, Bendall M. Falls by elderly people at home: prevalence and associated factors. Age Ageing 1988; 17: 365-372.
- Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol 1989; 44: 112-117.
- Liu‐Ambrose T, Khan KM, Eng JJ. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: A 6‐Month Randomized, Controlled Trial. J Am Geriatr Soc 2004; 52: 657-665.
- Society AG, Society G, Prevention OF. Guideline for the prevention of falls in older persons. J Am Geriatr Soc 2001; 49: 664-672.
- Calys M, Gagnon K, Jernigan S. A validation study of the Missouri alliance for home care fall risk assessment tool. Home Health Care Management Pract 2013; 25: 39-44.
- World Health Organization. WHO global report on falls prevention in older age. World Health Organization, Geneva 2008.
- Montero-Odasso M, Schapira M, Soriano ER. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol 2005; 60: 1304-1309.
- Jaehyun L. Responsiveness of gait speed to physical exercise interventions in at-risk older adults: A systematic review and meta-analysis. Ann Geriatr Med Res 2017; 21: 17-23.
- Middleton A, Fritz SL, Lusardi M. Walking speed: the functional vital sign. J Aging Physical Activity 2015; 23: 314-322.