Research Article - Biomedical Research (2018) Artificial Intelligent Techniques for Bio Medical Signal Processing: Edition-II
Expression on MDR 1 gene in cord blood nuclear cells
Zhao Fuguang, Zhang Wenhui, Li Xiaoling and Hu Wei*
Jilin Agricultural University, PR China
Accepted on April 27, 2017
DOI: 10.4066/biomedicalresearch.29-17-696
Visit for more related articles at Biomedical ResearchAbstract
Chemotherapy is at present one of the most commonly used methods to treat malignant tumors, but along with the killing of the tumor, normal tissue cells and bone marrow cells are also damaged, which would ruin the effectiveness of chemotherapy. Currently focuses on chemotherapy research are overwhelming the side effects and ensure the smooth conduct and efficacy of chemotherapy. In this paper human umbilical cord blood mononuclear cells were used as target cells. MDR 1 was inserted into the adenovirus vector. Recombinant adenovirus plasmid pHVa MDR 1 was constructed. And exogenous MDR 1 could be effectively transferred into the umbilical cord blood nuclear cells by the method of concentrated virus supernatant. The result shows that umbilical cord blood nuclear cells which can express P-gp. P-gp expressed is used to transfer exogenous MDR 1 gene into umbilical cord blood cells by concentrated virus supernatant transfection method.
Keywords
MDR 1 gene, Cord blood nuclear cells, Concentration-recombined virus, P-gp.
Introduction
Malignant tumor is a systemic and heterogeneous disease. Systemic chemotherapy has a pivotal status in the comprehensive treatment of malignant tumors. But in clinical therapy, the effects of chemotherapy are often unsatisfactory. Research found MDR 1 genes are expressed excessively in tumour cells, resulting in large amounts of P-gp which leads to the resistance. This is the main mechanism of drug resistance. Located on the cell membrane, P-gp can pump out drugs from the cell and reduce drug concentration within the cell. Taking advantage of the knowledge of this mechanism, people use Pgp monoclonal antibodies and some novel technologies and therapy to reverse the tumor cell expression of P-gp. However, due to the side effects, it is difficult to use clinically. Experiment shows that the bone marrow cells’ P-gp expression is extremely low, and due to the sensitivity to chemotherapy drugs, it is easy to lead to bone marrow restraint. Therefore, if MDR 1 gene is induced into bone marrow hematopoietic cells and P-gp is highly expressed, this can strengthen bone marrow hematopoietic cells’ chemotherapy toleration. The patients then can tolerate higher and more doses during the whole course of chemotherapy. The above study confirmed that the human MDR 1 gene can be transfected into various types of cells with stable P-gp expression.
Methods
The supernatant preparation of concentration
According to adenovirus kit instructions, the supernatant preparation of concentration was recombined with virus and the determination of titer of recombined virus.
The separation of cord blood nuclear cells (CBNC)
Two-step separation of umbilical cord blood components: Separate whole blood and Process white film which is rich of nucleated cells.
CPD (S-200) anticoagulation umbilical blood and centrifuge 2000 rpm 20~30 min were used to absorb plasma slowly by plasma exhaust tube or sucker. It was then put it into a nonbacterial bottle. Multiple umbilical plasma (including A, B, O and AB blood group of two or more) samples were collected after mixing and cryopreservation spare. Absorb white film; put it into a tube for further process. Cryopreserve the remaining erythrocyte.
5 ml of umbilical cord blood 5 ml was taken and 4°C precooled erythrocyte lysis buffer was added to a volume of 50 ml. It was left for 10 min after mixing, centrifugated and the liquid supernatant was discarded. It was then washed twice and the resulting suspension of CBNC was stored.
Transfected CBNC by supernate of concentrated viral
The heparinized CBNC layer into 1 × 107/ml was separated and prepared. The CBNC mentioned above was taken. Transfection system was used; it had 24 holes 1ml in size. In each hole, 1 × 107 cells, 3% L-Glu for 10 μl. 2-ME 5 μl (10-4 mol), polyberene 30 μl (200 μg/ml), 10% BSA 0.1 ml, EPO 40 μl (50 U/ml), IL-3 50 μl (2000 U/ml), IL-6 50 μl (100 ng/ml), SCF 50 μl (2000 U/ml) was added. Then wet incubate with 20 percent FBS’s IMDM complement was added to 1 ml at 37°C 5% CO2.
To detect the insertion of gene MDR 1 in CBNC by the method of PCR
Transfected and untransfected culture cells were taken on the 2nd, 4th and 6th day; around 6 × 106/ml was taken and the conventional method was used to extract DNA. Phenolchloroform extraction DNA of cells was assayed. 25 μl amplification system (including distilled water 17 μl, primer P1 P2 each 0.5 μl, buffer 2.5 μl, Taq enzyme 0.5 μl, DNA touched plate 2 μl, dNTPs 0.5 μl, MgCl2 1.5 μl) was used. Cycling conditions: 94°C 5 min; 94°C 45 s, 58°C 45 s, 72°C 60 s, a total of 35 cycles, 72°C 10 min; Primer sequences: justice chain"5’-CCCATCATTGCAATAGCAGG", antisense chain "5’-GTTCAAACTTCTGCTCCTCA”. A rubber board was used to carry 10% ethidium bromide to show color 10min. it was observed and photographed by ultraviolet methods.
To determine the transfection rate of exogenous genes MDR 1 transfected CBNC by the method of immunohistochemistry
Transfected cells and untransfected cells were collected on the 2nd, 4th and 6th day, and washed with PBS with a centrifugal. Cell concentration was adjusted to about 1 × 107/ml with PBS. Smears were prepared with centrifugal smear machine; 20°C acetones were used to dry them; they were washed three times with PBS and then soaked in 75% ethanol. Finally, they were stored at -20°C for immunohistochemistry. The first antibodies are P-gp monoclonal antibody; the second antibodies are biotin mark antibodies. Cell membrane and the cytoplasm which are both not responders are designated (-). The cytoplasm and cell membrane which are shallow brown coloured are designated (+). The cytoplasm and cell membrane which are light brown coloured are designated (++). The cytoplasm and cell membrane which are dark brown coloured are designated (++ +). The cell membrane which contained dark brown particles and the cytoplasm which was dark brown coloured was designated (++++).
Detection on P-gp positive rate of Exogenous MDR 1 gene transfected CBNC
Cultured cells to be tested were separated into 2 × 106/ml suspensions. Adding Daunorubicin (DNR) into each tube, the final concentration is 7.5 μg/ml. Then incubating them at 37°C, 5% CO2 for 10 min. After the function of termination of the pump by verapamil ingot, the concentration is 10 μg/ml. They were then washed twice with PBS before observing and counting them under a fluorescence microscope.
Determination on P-gp expression of the CBNC by indirect ELISA
Our experiment collected cell culture of 293 transfected cells on the 2nd, 4th and 6th day under the condition of -20°C; they were thawed before using. At same time, a comparison was made between the collected transfected cells and 293 normal cells. This was done by centrifuging them overnight with 5000 r for 10 min to coated microtiter plates and then adding to each 50 μl 18% of formaldehyde at 37°C for 30 min. Then, remove the coating buffer; it was closed with 3% gelatin at 37°C for 1 h and washed 3 times with lotion which contains 0.5 ml/L Tween-20 PBS (Ph7.2) for 3 min each time. After this, MdrC McAb (1:200 ascites) for 2 h was added, it was rewashed three times, goat anti-mouse secondary antibody (1:4000) with the HPR label was added, a sense was made for 2 h and it washed three times. Finally, chromogenic substrate solution was dropped and OD490 values were measured.
Detection of biological characteristics of the cord blood cell cycle of transfected MDR 1 gene
The cultured cells to be tested were made into 2 × 105/ml single cell suspensions, and washed two times with PBS. Collected cells were centrifuged for 5 min under 1500 rpm. The 0.1 μg/ml RNase solution was left in a 37°C water bath for 30 min, propidium iodide working solution dark stain at 4°C was added at 30 min, and then detection with flow cytometry was conducted. This produced 293 normal human lymphocyte cells as controls.
Results
Virus titer was determined. Recombinant adenoviral vector was diluted by dilution method; 293 cells were infected. TCID50 was calculated by using the Karber formula. The titer is about 4 × 109 PFU/ml.
The cells growth conditions after the MDR 1 gene transfected CBNC. CBNC were transfected by MDR 1 in vitro and half of the medium was changed every other day. Observation by an inverted microscope revealed that the group of cells that had been transected for 2 to 4 days was growing well. The cells were homogeneous and transparent. The group of cells that had been transected for 4 days produced a large number of cell colonies. The cell number in every hole increased to 1.0 × 106~1.5 × 106 from 2.0 × 105~5.0 × 105. However, the group of cells that had been transected for 6 days did not grow well. The contrasts of the cell contour were enhanced. Grains and vacuoles were appearing in the cytoplasm.
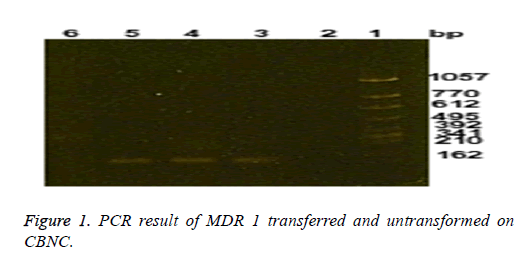
Integration and expression results of exogenous MDR 1 gene in CBNC. Application of MDR 1 plasmid transfected CBNC using specific primers for PCR amplification of the MDR 1 yielded the result shown in Figure 1. From the results it can be seen that specific amplified product bands appeared on 157 bp in cells, but not in negative control and untransformed cells. This proves successful integration of exogenous genes into the DNA of target cells.
Transfection ratio on exogenous MDR 1 transfection CBNC by immunohistochemical
CBNC were cultured for two, four and six days respectively. Transfected MDR 1 group and untransfected group showed immunohistochemical results; P-gp expression is shown in Table 1, (293 cells as the positive control). As seen from Table 1, the transferred group and untransfected were compared on the same day with P<0.01; transfection ratio increased in transfected group with time, P<0.01.
| Transferred time and division groups | P-gp level | Transfected rate (%) | ||||
|---|---|---|---|---|---|---|
| + | ++ | +++ | ++++ | |||
| 2 d | Transfected group | 9 | 6 | 2 | 0 | 17* |
| Untransfected group | 1 | 0 | 1 | 0 | 2 | |
| 4 d | Transferred group | 10 | 12 | 5 | 3 | 30* |
| Untransfected group | 0 | 1 | 1 | 0 | 2 | |
| 6 d | Transfected group | 12 | 13 | 8 | 5 | 38* |
| Untransfected group | 0 | 1 | 0 | 0 | 1 | |
| 293 cells as positive control | 20 | 40 | 30 | 10 | 100 | |
Table 1. Transfection ratio of MDR 1 transferred and untransfected in CBNC on different time.
Positive rate determination of P-gp on exogenous MDR 1 transfected CBNC and comparison between groups
CBNC were cultured on 2nd, 4th and 6th days. Transfected MDR 1 group and untransfected group showed that P-gp was expressed (293 cells as the positive control). The results are shown in Table 2. Seen from the Table 2, through statistical analysis, difference in P-gp expression was statistically significant between transfected MDR 1 group and untransfected group (P<0.05). It is clearly seen that the more days the group is transfected, the higher the transfection ratio.
| Transferred time and division groups | P-gp level | The positive ratio of cellular DNR | ||||
|---|---|---|---|---|---|---|
| + | ++ | +++ | ++++ | |||
| 2 d | Transferred group | 9 | 6 | 2 | 0 | 68** |
| Untransferred group | 1 | 0 | 1 | 0 | 94 | |
| 4 d | Transferred group | 10 | 12 | 5 | 3 | 55** |
| Untransferred group | 0 | 1 | 1 | 0 | 95 | |
| 6 d | Transferred group | 12 | 13 | 8 | 5 | 24** |
| Untransferred group | 0 | 1 | 0 | 0 | 95 | |
| 293 cells as positive control | 20 | 40 | 30 | 10 | 0 | |
Table 2. Positive rate determination of P-gp on exogenous MDR 1 transfected CBNC and comparison between groups.
Test results of biological characteristics of the MDR 1 gene transfected cord blood cells
In the transfection group, umbilical cord blood cells in the proliferative phase (G2-M+S) cells accounted for 6.13%, quiescent (G0-G1) cells accounted for 93.87%. The untransfected cord blood cells in the proliferative phase (G2-M +S) cells accounted for 5.38%, quiescent (G0-G1) cells accounted for 94.62%; there was no aneuploidy, debris or accumulation in the body. The difference in biological characteristics was not statistically significant between the two groups of cell cycle by χ2. (P>0.05), the results are shown.
Discussion
When cancer patients are receiving chemotherapy, the effects of chemotherapy can be influenced and it cannot be implemented on schedule for its damage to normal cells and bone marrow cells. Currently, the factors which affect hematopoietic growth are used to shorten the duration of neutropenia after chemotherapy in clinical treatments. Ingredient transfusion and other supportive therapy are used to reduce bone marrow suppression after chemotherapy. However, chemotherapy-induced myelosuppression cannot be prevented. Repetitive chemotherapies may also cause normal bone marrow hematopoietic cell reserves to decrease, even causing bone marrow failure. In this study, cord blood nucleated cells were transfected by adenovirus-mediated MDR 1, to enhance their resistance to chemotherapeutic drugs. They were expected to overcome the injury of bone marrow cells and leukocytes during cancer chemotherapy. This plays an important role in improving the efficacy of chemotherapy. The study also intends to explore a way which can resist the cytotoxic effects of anticancer drugs during treatment. It aims to learn to increase the dose of chemotherapy drugs without the damaging hematopoietic cells, thereby enhancing the effects of chemotherapy.
Target cells of gene transfection should have the functions of self-renewal, proliferation and differentiation. Cells with these functions are known to be none other than stem cells. Therefore, pluripotent stem cells are often used for transplantation and for gene therapy research as target cells [1]. CBNC which is rich in hematopoietic stem/progenitor cells was used as target cells for gene transfection. Reasons that CD34+ stem/progenitor cells were not purified are as the follows: (1) the great loss of stem/progenitor cell in purification process; (2) the decay of interaction between cells; (3) the damage of micro-environment in which cord blood stem/progenitor cells stay.
Some scholars believe that cord blood cell cytokines may be provided independently in the form of paracrines, which support stem/progenitor cell proliferation. Therefore, this experiment is about how MDR 1 gene was transfected into CBNC of proliferating exuberant. The result of stem/progenitor cell proliferation was also shown at the end. After 6 days of culturing, cells counting per well in 24-well plate grew from 1 × 106 to (1~2) × 107. The MDR 1 gene transfection rate was 30%.
The MDR 1 gene was imported into cord blood hematopoietic cells after reinfusion to make colonies; also to exert its function after its reinfusion and colonization. The key is how to improve MDR 1 gene transfection efficiency in vitro and colonization rate of transfected bone marrow hematopoietic cell. This makes a search for choosing MDR 1 gene transfect cord blood nuclear cells, discussing feasibility, efficiency and stabilized condition of transfection MDR 1 gene, while it is the base to further the establishment of MDR 1 gene transfected autologous cell transplantation model and chemotherapy experimental in vivo.
High efficiency and stable transfection system in vitro are the prerequisites for the successful application in vivo. There are three key factors in transfection system, namely, the carrier, transfection conditions (mainly refers to a combination of cytokines), and the target cells. MDR 1 gene is not only the resistance gene of tumor cells, but also a protection gene for normal cells from foreign body violation [2]. But in the bone marrow, P-gp expression is lower than tumor tissue, making it prone to myelosuppression in chemotherapy. To increase protection of hematopoietic cells in chemotherapy, we chose human MDR genes to transfect into human umbilical cord blood hematopoietic cells. Research has shown that the addition of IL-3, IL-6 and SCF is the best for improving transfection efficiency. Our study chose the combination of IL-3, IL-6, SCF, EPO, GM-CSF to induce growth of umbilical cord blood nuclear cells from hematopoietic stem/progenitor cells which are rich of CD34+ in vitro. The purpose is to facilitate the integration of the target gene while prompting stem/progenitor cells amplification in vitro [3].
Conclusion
The recombinant adenovirus is used to transfer exogenous MDR 1 gene into umbilical cord blood cells by concentrated virus supernatant transfection method, and P-gp is expressed.
Acknowledgements
The authors would like to give their thanks to Changchun Science and Technology Bureau (NO.14KG056), National Nature Fund (NO.31572372), Jilin Education and Science Institute (ZD15050) for their financial and technical support.
References
- Eridani S, Mazza V, Massaro P. Cytokine effect on ex vivo expansion of haemopoietic stem cells from different human sources. Biotherapy 1998; 43: 291-296.
- Cairos WJE. Placental and/or umbilical cord blood: an alternative source of hematopoietic stem cells for transplatation. Blood 1997; 90: 4665-4676.
- Shtil AA. Signal transduction pathways and transcriptional mechanisms as targets for prevention of emergence of multidrug resistance in human cancer cells. Curr Drug Targets 2001; 2: 57-77.