- Biomedical Research (2016) Volume 27, Issue 3
Evaluation of the relationship between thromboembolic risk score (CHA2DS2-VASc) and inflammation and coagulation markers in patients with non-valvular atrial fibrillation in emergency department.
Fatih Nazmi Yaman1, Birol Civelek2, Bunyamin Yavuz3, Mustafa Yilmaz4*, Metin Atescelik4, Mustafa Sahan5, Mehmet Cagri Goktekin4
1Department of Emergency Medicine, Faculty of Medicine, Sutcu Imam University, Kahramanmaras, Turkey
2Department of Plastic and Reconstructive Surgery, Kecioren Teaching and Research Hospital, Ankara, Turkey
3Department of Cardiology, Kecioren Teaching and Research Hospital, Ankara, Turkey
4Department of Emergency Medicine, Faculty of Medicine, Firat University, Turkey
5Department of Emergency Medicine, Faculty of Medicine, Mustafa Kemal University, Hatay, Turkey
- *Corresponding Author:
- Mustafa Yilmaz
Department of Emergency Medicine
Firat University Faculty of Medicine
Turkey
Accepted Date: February 26, 2016
Abstract
Objective: To evaluate the relationship between CHA2DS2-VASc score and inflammation and coagulation markers in patients admitted to Emergency Department (ED) with non-valvular Atrial Fibrillation (AF).
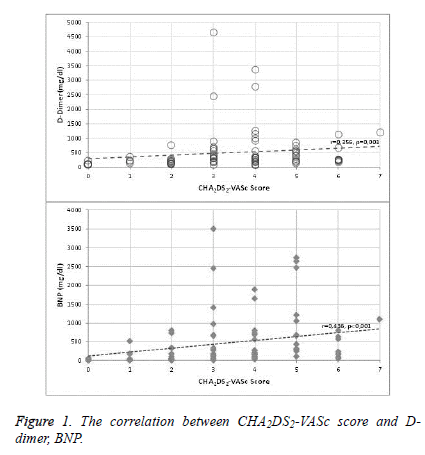
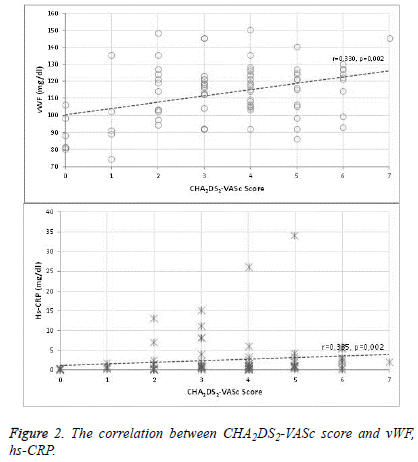
Methods and Results: Eighty-four patients with non-valvular AF were included in the study. CHA2DS2- VASc scores were calculated for these patients. In addition, plasma levels of BNP, hs-CRP, CRP, vWF and D-dimer were measured. The relationship between CHA2DS2-VASc score and these parameters were evaluated. Eleven (13%) patients were considered to be at low-risk due to CHA2DS2-VASc score being<2 and 73 (87%) patients were considered to be at high risk due to CHA2DS2-VASc score being ≥ 2. The mean age of patients was 68 ± 13 years and 50 (60%) of patients were male. Plasma BNP, hs-CRP, CRP, vWF and D-dimer levels were significantly higher in high-risk group. In addition, a significant positive correlation was found between CHA2DS2-VASc score and BNP (r=0.436, p<0.001), D-Dimer (r=0.356, p=0.003), hs-CRP (r=0.335, p=0.002), CRP (r=0,331, p=0.002), vWF (r=0.330, p=0.002) and patient age (r=0.573, p<0.001).
Conclusion: It was found that BNP, hs-CRP, CRP, vWF and D-dimer levels increase significantly and that there is a positive correlation between CHA2DS2-VASc and these markers in high-risk patients with CHA2DS2-VASc score ≥ 2.
Keywords
Atrial fibrillation, BNP, CHA2DS2-VASc score, D-Dimer, hs-CRP, vWF.
Introduction
Atrial Fibrillation (AF), seen in 1-2% of the general population, is the most common arrhythmia among cardiac arrhythmias and causes five-fold increase in the risk of stroke. The prevalence of AF is expected to double due to aging of the population [1-3]. Studies are being conducted towards the use of clinical classification and certain biochemical markers to determine the risk of stroke in patients with AF [4]. CHA2DS2- VASc classification is one of the classifications made to demonstrate the risk of stroke development. CHA2DS2-VASc [Congestive heart failure, Hypertension, Age ≥ 75 years (double), Diabetes Mellitus, Prior Stroke or TIA or thromboembolism (double), Vascular disease, Age 65-74 years, Sex category (female)] classification is a scoring table, recommended at the 2010 European Society of Cardiology (ESC) Management of Atrial Fibrillation guideline for use in determining the treatment and risk of thromboembolism in patients with non-valvular AF, including many up to date risk factors and a scoring scheme ranging between 0 and 9 points. Oral anticoagulation therapy (OAC) is recommended in patients with CHA2DS2-VASc score ≥ 2, unless there is a contraindication [5].
Brain Natriuretic Peptide (BNP), C Reactive Protein (CRP), plasma von Willebrand Factor (vWF) and plasma D-dimer levels have been used to evaluate cardiovascular functions and determine the risk of thrombosis in many cardiovascular diseases such as heart failure, atherosclerotic heart disease [6-12]. Plasma BNP levels have been found to be very sensitive in identifying left ventricular dysfunction in patients with Congestive Heart Failure (CHF) and increased BNP levels have been reported with increased severity of left ventricular dysfunction [6]. BNP level has also been found to be associated with atrial pressure increase [7]. CRP, an acute phase reactant synthesized in the liver, is one of a very sensitive marker of acute and chronic inflammation. Due to studies indicating increased levels of hs-CRP in Coronary Artery Disease (CAD), the role of hs-CRP in the ethiopathogenesis of other cardiovascular diseases has been investigated. As a result of the studies, chronic inflammation has been reported to be effective in the ethiopathogenesis of AF [4].
Elevated plasma vWF levels has been shown in inflammatory and atherosclerotic vascular diseases, in which there is the possibility of endothelial damage [8]. Plasma D-Dimer levels, best biochemical markers of coagulation activity [9], shows the prothrombotic state and thromboembolic risk [10]. It has been stated that D-dimer level increases in the presence of left atrial thrombus and that it is correlated with the volume of thrombus [11]. Although the clinical classifications and biomarker levels were investigated separately in the development of thrombosis, there are not enough studies found in the literature that investigate the relationship between CHA2DS2-VASc score and inflammation and coagulation markers. Therefore, we aimed to evaluate the relationship between CHA2DS2-VASc score and inflammation and coagulation markers in patients who admitted to emergency department with non-valvular AF.
Materials and Methods
The study was initiated following obtaining the approval of the local ethics committee and 84 patients, who were admitted to Emergency Department (ED) with non-valvular AF, were included. Biochemical tests, cardiovascular disease history, risk factors, waist circumference, height measurements and physical examinations of the patients were performed in a detailed manner. Patients with the following characteristics, which may cause contradictions in determining the relationship between CHA2DS2-VASc score and inflammation and coagulation markers and determining the CHA2DS2-VASc score, were excluded from the study:
1. History of previous venous or systemic thromboembolism in the last 3 months
2. History of valvular heart disease and prosthetic heart valve
3. Patients on Warfarin
4. History of previous myocardial infarction in the last 3 months
5. History of previous inflammatory or infectious disease in the last 1 month
6. History of previous surgery in the last 3 months
7. Patients with a history of malignancy
8. Patients under 18 years of age
9. Patients with connective tissue disease
10. Patients with a history of active tuberculosis (TB)
11. Patients with a history of hyperthyroidism and hypothyroidism
The points were summed up according to the criteria in CHA2DS2-VASc scheme and CHA2DS2-VASc score of each patient was calculated, ranging from 0 to 9. Patients were divided into two groups, as high-risk group with score ≥ 2 and as low-risk group with score<2. AF diagnosis was made by clinical signs and marked irregular RR intervals and absolute absence of P waves on electrocardiogram. In order to detect the presence of atrial thrombi, all patients in the study underwent transthoracic echocardiography. Blood samples were collected from the antecubital veins into VACUETTE® gel vacuum tubes (Greiner Bio-One, Austria). Plasma samples were stored at -70 °C, no more than 6 months. BNP concentrations were determined with IMMULITE® 2000 immunoassay system (Siemens, Germany) by electrochemiluminescence immunoassay (ECLIA) method.
Normal range for BNP was 0-100 pg/ml. vWF and D-dimer levels were measured with AMAX 190® coagulometer (Sigma Diagnostics, UK) by using an immuno-turbidimetric method. Normal ranges for D-dimer and vWF were 0-250 ng/ml and 60-150%, respectively. hs-CRP was measured with IMMAGE® immunochemistry system (Beckman Coulter, USA). The lower limit of hs-CRP detection was 0.2 mg/L. SPSS 15.0 statistical software package was used for the evaluation of variables and tests. While numerical variables with normal distribution and without normal distribution were expressed as mean ± standard deviation and median (minimum-maximum), respectively, categorical variables were expressed as percentage. Analysis of variance (ANOVA) method was used for the comparison of the mean in numerical variables with normal distribution. Mann-Whitney U test was used for the comparison of the median in the numeric variables without normal distribution. Spearman's Rank Correlation was used for two-way analysis and linear regression analysis was used for multivariate analysis of factors affecting the CHA2DS2-VASc score. p <0.05 was considered significant in statistical analysis.
Results
In the study, 50 (60%) of 84 patients were male and the mean age of patients was 68 ± 13 years. CHA2DS2-VASc score was found to increase with increased age (r=0.573, p<0.001). Hypertension, diabetes mellitus, CAD, previous Cerebrovascular Accident (CVA) and CHF was present in 77.4%, 26.2%, 39.3%, 14.3% and 22.6% of patients, respectively. Twenty-seven point four percent of patients were smokers and 2.4% were alcohol users (Table 1). While 12 (14.3%) patients had paroxysmal AF, 72 (85.7%) had permanent AF. The number of patients based on CHA2DS2- VASc scores was determined as follows: 0 (n=6), 1 (n=5), 2 (n=12), 3 (n=17), 4 (n=21), 5 (n=13), 6 (n=9) and 7 (n=1). Significant positive correlation was found between CHA2DS2- VASc score and BNP (r=0.436, p<0.001), D-Dimer (r=0.356, p=0.003), hs-CRP (r=0.335, p=0.002), CRP (r=0.331, p=0.002) and vWF (r=0.330, p=0.002) (Figure 1 and Figure 2). Patients were divided into 2 groups according to CHA2DS2-VASc scores. Eleven (13%) patients were found to be at low-risk and 73 (87%) patients were found to be at high-risk. Plasma BNP (p<0.001), D-Dimer (p=0.008), plasma hs-CRP (p=0.002), CRP (p=0.003) and vWF (p<0.001) levels of patients with high-risk were statistically significantly higher compared to low-risk group (Table 2). Multivariate linear regression analysis of inflammation and coagulation markers that affect CHA2DS2-VASc score revealed only BNP (beta=0.372, T=3.562, p=0.001) and vWF (beta=0.216, T=2.066, p=0.042) as independent correlates.
| Data | Patients with low-risk (CHA2DS2-VASc score<2) | Patients with high-risk (CHA2DS2-VASc score =2) |
|---|---|---|
| N (F/M) | 11 (2/9) | 73 (48/25) |
| Age (Mean ± SD) | 49 ± 9.78 | 71 ± 10.48 |
| Hypertension (n (%)) | 1 (1.2%) | 64 (76.2%) |
| Diabetes (n (%)) | 0 (0%) | 22 (26.2%) |
| Heart Failure (n (%)) | 1 (1.2%) | 18 (21.4%) |
| Previous CVA (n (%)) | 0 (0%) | 12 (14.3%) |
| CAD (n (%)) | 1 (1.2%) | 32 (38.1%) |
| Smoker (n (%)) | 8 (9.5%) | 15 (17.9%) |
| Alcohol use (n (%)) | 2 (2.4%) | 0 (0%) |
Table 1: The demographic characteristics of patients.
| Parameters | Patients with low-risk (CHA2DS2-VASc score<2) | Patients with high-risk (CHA2DS2-VASc score =2) | P |
|---|---|---|---|
| N (F/M) | 11 (2/9) | 73 (48/25) | - |
| BNP (mg/dl) | 12 (3-518) | 250 (8,5-3500) | <0.001 |
| vWF (mg/dl) | 89 (74-135) | 118 (86-150) | <0.001 |
| D-Dimer (mg/dl) | 129 (76-349) | 287 (66-4637) | 0.008 |
| hs-CRP (mg/dl) | 0,3 (0,1-1.7) | 1,0 (0.3-34) | 0.002 |
| CRP (mg/dl) | 0,4 (0,1-1.4) | 1,1 (0.1-28) | 0.003 |
Table 2: Inflammation and coagulation markers in low and high-risk patients.
Discussion
AF is an arrhythmia associated with hemostatic abnormalities and an increased risk of thromboembolic events [12,13]. Thromboembolism recurrence rates and the frequency of cardiovascular events are increasing due to AF [3]. Identification of risk factors for stroke in patients with AF and initiation of OAC treatment to patients at high-risk have a privileged position. CHA2DS2-VASc scoring is used to identify stroke risk factors. One-year event rate of patients with a CHA2DS2 score of 0 ranges as follows: 0.84% (CHA2DS2- VASc score=0), 1.75% (CHA2DS2-VASc score=1), 2.69% (CHA2DS2-VASc=2), and 3.2% (CHA2DS2-VASc=3) [14]. In addition to risk scoring in patients with AF, some biomarkers have also been used to determine the risk of stroke. In the literature, elevated plasma BNP levels were reported in nonvalvular AF patients with thromboembolism episodes [15]. In another study, plasma BNP levels in AF have been shown to increase in the acute phase of CVA and decrease within 1 month [16]. Plasma BNP levels have been suggested to be a promising effective biomarker in distinguishing high-risk AF from low-risk AF. However, it has not been reported whether BNP is predictive before thromboembolic events in patients with atrial fibrillation [17]. High BNP levels have been shown in patients with congestive heart failure and stroke in the literature [16,18]. There are not enough studies examining the relationship between BNP and CHA2DS2-VASc score in the literature. In our study, we have identified significantly higher plasma BNP levels in high-risk group compared to low-risk group and a positive correlation between CHA2DS2-VASc score and BNP.
Plasma inflammatory markers have been reported to be associated with prognosis after ischemic stroke and cardiac events [19]. Plasma hs-CRP levels have been concluded to be a predictor of carotid atherosclerosis, stroke and CAD [20-23]. But the role of increased inflammatory markers in determining the prognosis after first ischemic stroke is not clear [21]. In the last statement made by European CRP Pooling Project, it has been concluded that there is insufficient data in the relationship between plasma hs-CRP levels in stroke patients [21]. In another study, significant association was found between CHADS2 score and systemic inflammation, left atrial thrombus formation and cardiovascular events in patients with nonvalvular atrial fibrillation. As a result of this study, a significant relationship was found between plasma CRP levels and CHADS2 score [24]. A positive correlation was also found between CHA2DS2-VASc and CRP, hs-CRP levels in our study. As a result of our study similar to the above study, plasma CRP and hs-CRP levels were significantly higher in patients with a CHA2DS2-VASc ≥ 2 compared to those with a score <2. In our study, as patients with inflammatory and infectious diseases, collagen tissue diseases, active TB, malignancy and patients on Warfarin were excluded, CRP and hs-CRP levels were unaffected by these factors and this did not affect our study negatively.
vWF levels in patients with AF have been shown to be significantly higher compared to patients with sinus rhythm [25]. vWF levels have been identified to increase in women with AF, but no similar association was found in men [26]. Stroke and vascular events are known to occur due to endothelial dysfunction [27]. In his study, Roldan V et al. [4], have determined significantly higher vWF levels in AF patients with CHADS2 ≥ 2. In our study, vWF levels in patients with CHA2DS2-VASc score ≥ 2 were significantly higher than the low-risk group. In addition to the increased hypercoagulability in patients with AF, fibrinolytic system is impaired [28]. Plasma D-Dimer levels have been guiding in determining the risk of thromboembolism and deciding to start antithrombotic treatment in AF [28]. Elevated levels of plasma D-Dimer in patients with AF have been associated with increased thromboembolic and cardiovascular events [28]. Further, combined with clinical risk factors, plasma D-dimer levels have been concluded to be useful in risk scoring classification [18]. Prothrombotic state in AF is caused by vascular endothelial dysfunction, stasis and thrombus formation in the left atrium and low fibrinolytic functions [29]. These causes lead to thromboembolism and the embolism activates the coagulation systems, which in turn increases levels of plasma D-dimer, which is fibrin degradation product [29]. In clinical trials, warfarin use has been shown to reduce plasma D-Dimer levels [30]. Plasma D-Dimer levels in the high-risk group were also found to be higher than the low-risk group in our study. As we excluded the patients on warfarin from our study, the plasma D-dimer levels were not affected by warfarin and this increased the accuracy of the results of our study.
Conclusion
In conclusion, the relationship between CHA2DS2-VASc risk score and inflammation (CRP, hs-CRP) and coagulation (BNP, D-dimer, vWF) was found to be significant. In addition to CHA2DS2-VASc risk score, plasma CRP, hs-CRP, BNP, Ddimer, vWF levels may help in identification of risk factors for stroke and decision making for starting anticoagulation therapy in patients with AF.
References
- Stewart S, Hart CL, Hole DJ, McMurray JJ. Population prevalence, incidence, and predictors of atrial fibrillation in the Renfrew/Paisley study. Heart 2001; 86:516-521.
- Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001; 285: 2370-2375.
- European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 2010; 31:2369-2429.
- Roldán V, Marín F, García-Herola A, Lip GY. Correlation of plasma von Willebrand factor levels, an index of endothelial damage/dysfunction, with two point-based stroke risk stratification scores in atrial fibrillation. Thromb Res 2005; 116: 321-325.
- Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'Gara P, Rubin GD. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography. JAmColl Cardiol 2010;56: 1864-1894.
- Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, Ganiats TG. ACC/AHA Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult. Circulation 2001; 104: 2996-3007.
- Munagala VK, Burnett JC, Redfield MM. The natriuretic peptides in cardiovascular medicine. Curr Probl Cardiol 2004; 29: 707-769.
- Blann AD, Lip GY. The endothelium in atherothrombotic disease: assessment of function, mechanisms and clinical implications. Blood Coagul Fibrinol 1998; 9: 297-306.
- Sie P. The value of laboratory tests in the diagnosis of venous thromboembolism. Haematologica 1995; 80: 57-60.
- Hager K, Platt D. Fibrin degeneration product concentrations (D-dimers) in the course of ageing. Gerontology 1995; 41: 159-165.
- Hayashi I. Laboratory diagnosis of left atrial thrombi in patients with mitral stenosis. Fukuoka igaku zasshi=Hukuoka acta medica 1991; 82: 550-561.
- Go AS, Hylek EM, Chang Y, Phillips KA, Henault LE, Capra AM, Jensvold NG. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA 2003; 290: 2685-2692.
- Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Annal Internal Medicine 2007; 146: 857-867.
- Olesen JB, Torp-Pedersen C, Hansen ML, Lip GY. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0-1: a nationwide cohort study. Thromb Haemost 2012; 107: 1172-1179.
- Shimizu H, Murakami Y, Inoue S, Ohta Y, Nakamura K, Katoh H, Sakne T. High plasma brain natriuretic polypeptide level as a marker of risk for thromboembolism in patients with nonvalvular atrial fibrillation. Stroke 2002; 33: 1005-1010.
- Shibazaki K, Kimura K, Okada Y, Iguchi Y, Terasawa Y, Aoki J. Heart failure may be associated with the onset of ischemic stroke with atrial fibrillation: a brain natriuretic peptide study. J Neurol Sci 2009; 281: 55-57.
- Sadanaga T, Kohsaka S, Mitamura H, Ogawa S. Elevated B-type natriuretic peptide level as a marker of subsequent thromboembolic events in patients with atrial fibrillation. Heart Vessels 2011; 26: 530-535.
- Sadanaga T, Sadanaga M, Ogawa S. Evidence that D-dimer levels predict subsequent thromboembolic and cardiovascular events in patients with atrial fibrillation during oral anticoagulant therapy. J Am Coll Cardiol 2010; 55: 2225-2231.
- Elkind MS, Tai W, Coates K, Paik MC, Sacco RL. High-sensitivity C-reactive protein, lipoprotein-associated phospholipase A2, and outcome after ischemic stroke. Arch Internal Med 2006; 166: 2073-2080.
- Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. Eng JMed 1997; 336: 973-979.
- Di-Napoli M, Schwaninger M, Cappelli R, Ceccarelli E, Di-Gianfilippo G, Donati C, Emsley HC. Evaluation of C-reactive protein measurement for assessing the risk and prognosis in ischemic stroke: a statement for health care professionals from the CRP Pooling Project members. Stroke 2005; 36: 1316-1329.
- Kistorp C, Raymond I, Pedersen F, Gustafsson F, Faber J, Hildebrandt P. N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. JAMA 2005; 293: 1609-1616.
- Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO 3rd, Criqui M, Fadl YY. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003; 107: 499-511.
- Maehama T, Okura H, Imai K, Yamada R, Obase K, Saito K, Hayashida A. Usefulness of CHADS2 score to predict C-reactive protein, left atrial blood stasis, and prognosis in patients with nonrheumatic atrial fibrillation. J Am Cardiol 2010; 106: 535-538.
- Friberg L, Hammar N, Rosenqvist M. Stroke in paroxysmal atrial fibrillation: report from the Stockholm Cohort of Atrial Fibrillation. Eur J Heart 2010; 31: 967-975.
- Conway DS, Heeringa J, Van Der Kuip DA, Chin BS, Hofman A, Witteman JC, Lip GY. Atrial fibrillation and the prothrombotic state in the elderly: the Rotterdam Study. Stroke 2003; 34: 413-417.
- Conway DS, Pearce LA, Chin BS, Hart RG, Lip GY. Prognostic value of plasma von Willebrand factor and soluble P-selectin as indices of endothelial damage and platelet activation in 994 patients with nonvalvular atrial fibrillation. Circulation 2003; 107:3141-3145.
- Roldán V, Marín F, Marco P, Martínez JG, Calatayud R, Sogorb F. Hypofibrinolysis in atrial fibrillation. J Am Heart 1998; 136: 956-960.
- Freestone B, Lip GY. The endothelium and atrial fibrillation. The prothrombotic state revisited. Hamostaseologie 2008; 28: 207-212.
- Lip GY, Lowe GD, Rumley A, Dunn FG. Increased markers of thrombogenesis in chronic atrial fibrillation: effects of warfarin treatment. Br Heart J 1995; 73: 527-533.