Research Article - Biomedical Research (2017) Volume 28, Issue 20
Drug utilization pattern of upper respiratory tract infections in pediatric at Najran university hospital, KSA
Saad Ahmed Alkahtani*
Department of Clinical Pharmacy, College of Pharmacy, Najran University, Najran, Kingdom of Saudi Arabia
- *Corresponding Author:
- Saad Ahmed Alkahtani
Department of Clinical Pharmacy
College of Pharmacy
Najran University
Kingdom of Saudi Arabia
Accepted date: October 30, 2017
Abstract
Upper Respiratory Tract Infections (URTIs) constitute the most common type of acute infections among children. Administration of antibiotics is the standard treatment option for most of the URTIs. However, antibiotics may be misused or overused in the URTIs treatment. The main objective of this observational study is to assess the drug utilization patterns in the treatment of URTIs among children referred to the pediatric of Najran University Hospital, Najran, Kingdom of Saudi Arabia. The subjects of the study consisted of 370 children of both genders (male and female) aged 0-14 y old who were referred to the out-patient department of the Hospital during July to November 2015. The most common prescribed antibiotic was azithromycin (38.66%), followed by cefixime (24.16%), and amoxicillin in combination with clavulanic acid (15.61%). Among the various drugs administered for the treatment of URTIs, analgesic and antipyretics (30.27%) were the most common class of drug, followed by the antihistamines (27.83%), expectorant (19.18%) and nasal decongestants (5.67%). The findings extended our understanding to optimize the rational use of medications for URTIs in paediatric and helped to establish the prescribing pattern.
Keywords
Antibiotics, Pediatrics, Upper respiratory tract infections, Drug utilization pattern
Introduction
Upper Respiratory Tract Infections (URTIs) are among the most prevalent clinical conditions and one of the most common reasons for pediatric consultations in the primary health care system [1,2]. These infections impose significant burden on the health care system of a country and one of the major reason for absenteeism of children from school and absenteeism of work for their parents [1]. The infection of upper respiratory tract mainly comprises the infections of the nose, tonsils, nasopharynx, eustachian tube, paranasal sinuses and adenoids [3]. URTIs account for the most frequent visits to physicians than any other infectious diseases among children [2]. URTIs include the diseases like the common cold, acute rhinitis, laryngitis and pharyngitis/tonsillitis [4]. Most URTIs are viral in origin with only 10% of them attributable to bacterial etiology [5]. Viral URTIs can be managed by symptomatic treatments such as antihistamines, antipyretics, anti-inflammatory agents, anti-tussive, expectorants and decongestants. The common bacterial pathogens responsible for such infections were include S. pneumoniae (25%), H. influenzae (20%), Moraxella catarrhali (12%) and others with 13%. Among these, the infections caused by S. Pneumonia are considered to be a major cause of morbidity and mortality among children [6]. For the treatment of the common cold, antimicrobial agents are not required unless the infection is complicated by tonsillitis, sinusitis, acute otitis media with effusion as well as infection of lower respiratory tract [7]. The treatments of URTIs commonly involve the use of antibiotics. Antimicrobials are the second leading therapeutic drug categorically prescribed by the physicians. According to the Center for Disease Control (CDC) guidelines, irrational use of antimicrobials in family practice in the United States revealed 79% of prescriptions were unnecessary [8]. In most of the cases of URTIs, antimicrobial prescribed are usually misused or over-use of antibiotic therapy [9,10]. The current trends to prescribe irrational antibiotics, particularly in pneumonia indicate that therapy is effective in reducing the complicated symptom. However, the antibiotic should be rationally prescribed only if the symptoms persist for 10-14 d [11]. Various factors are usually associated with the misuse of antibiotics at both pediatrician and patient level, but irrational antibiotic use still considered to be appropriate management in case of URTIs [12]. However, conducting comprehensive studies on Drug Utilization (DU) would facilitate the identification of the existed or emerging trends of drug prescription and practice more scientific and systematic [13].
DU study is an important aspect of medical review and plays a substantial role in pharmaco-epidemiological investigation and describes the practice of prescription written by physicians [14]. Multiple drugs practice or polypharmacy are not only imposing economy burden on patient and healthcare system but also adversely affects in terms of side-effects [15,16]. Such studies aid the identification of superfluous and irrational prescription, which increases the cost of treatment as well [17]. Although awareness of the consequences of antibiotic misuse is increasing, over prescribing practice steadily increases. It is mainly due to the patient demand, time constrain on physicians and diagnostic uncertainty. Clinicians must be judicious and more careful while prescribing antimicrobial agents, if the improvements in the treatment of infectious diseases are to be well-preserved [18-21]. The current investigations explore the recent prescription patterns of drugs used in the treatment of URTIs. The aim of the present study was to assess the trends in drug prescription, average number of drugs per prescription and WHO core indicators for drug utilization against UTRIs among paediatrics. Outcomes of the study are likely to provide appropriate and useful feedback to practitioners for rationale use of antibiotics.
Methods
DU study is an important aspect of medical review and plays a substantial role in pharmaco-epidemiological investigation and describes the practice of prescription written by physicians [14]. Multiple drugs practice or polypharmacy are not only imposing economy burden on patient and healthcare system but also adversely affects in terms of side-effects [15,16]. Such studies aid the identification of superfluous and irrational prescription, which increases the cost of treatment as well [17]. Although awareness of the consequences of antibiotic misuse is increasing, over prescribing practice steadily increases. It is mainly due to the patient demand, time constrain on physicians and diagnostic uncertainty. Clinicians must be judicious and more careful while prescribing antimicrobial agents, if the improvements in the treatment of infectious diseases are to be well-preserved [18-21]. The current investigations explore the recent prescription patterns of drugs used in the treatment of URTIs. The aim of the present study was to assess the trends in drug prescription, average number of drugs per prescription and WHO core indicators for drug utilization against UTRIs among paediatrics. Outcomes of the study are likely to provide appropriate and useful feedback to practitioners for rationale use of antibiotics.
A total of 370 URTIs paediatric patients of both genders (male and female) and age 0-14 y of paediatric OPD were included in the study with exclusion of mentally retarded and unconscious patients. The data were collected from the record room and recorded on a Drug Utilization Review (DUR) form as per WHO guidelines and weekly diary cards. Data on drug details (name of the drugs, dosage form, dose frequency and duration) and patient demographics (age, sex) were recorded. The total number of drugs prescribed, average number of drugs per prescription, and average number of antibiotics per prescription were determined. The observations were determined in the form of mean and percentage.
Results
A total of 1324 children visited Najran University Hospital (Najran, KSA) in paediatric OPD over the five-month period of this study. On the basis of inclusion and exclusion criteria, 370 children were selected for the study. Out of 370 children, 53.24 % were male (n=197) and 46.75% female (n=173). The majority of the children were from the 0-2 years of age (44.05%) while 12-14 y age group only 0.81% (Table 1).
| Age (y) | Male | Female | Total patients |
|---|---|---|---|
| 0-2 | 81 | 83 | 163 |
| 2-4 | 55 | 30 | 83 |
| 4-5 | 31 | 29 | 60 |
| 6-8 | 7 | 21 | 28 |
| 8-10 | 11 | 7 | 18 |
| 10-12 | 10 | 3 | 25 |
| 12-14 | 2 | 1 | 3 |
| Total | 197 | 173 | 370 |
| % of patients | 53.24% | 46.76% | - |
Table 1: Distribution of age and gender of the subjects of the study.
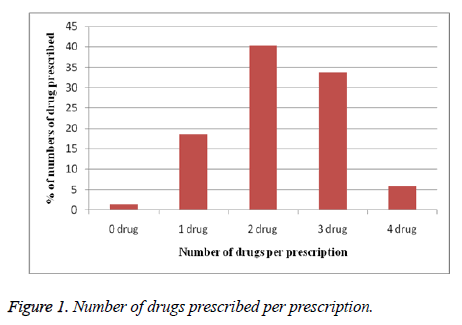
Of total patients, 40.27% (n=149) prescribed with two drugs per prescription, followed by 33.78% of patients (n=125) prescribed with three drugs per prescription (Figure 1).
The antibiotic was prescribed in 72.70% (n=269) of total prescription which is found to be 0.727 antibiotics per prescription and discuss (Table 2). Furthermore, the total number of drugs prescribed was found to be 830 while average of number of drugs per prescription is 2.27. It was found that 25.94% of children (n=96) received symptomatic treatment only while 72.7% of children (n=269) received both antibiotic as well as symptomatic treatment. However, 1.35% of children (n=5) did not receive any medication (Table 2).
| Parameters | Number |
|---|---|
| Total number of prescriptions analysed | 370 |
| Total number of drugs prescribed | 830 |
| Total number of prescriptions without drugs | 5 |
| Total number of prescriptions without antibiotics | 96 |
| Average number of drugs per prescription | 2.24 |
| Total number of prescriptions containing antibiotics | 269 |
| Average number of antibiotics per prescription | 0.727 |
| Percentage of medicine prescribed by generic name | 62.79% |
| Percentage of encounters with cough& cold preparations | 19.18% |
| Percentage of encounters with antihistaminic preparations | 27.83% |
| Percentage of encounters in which antibiotics are prescribed | 72.70% |
| Percentage of encounters without medications | 1.00% |
| Percentage of encounters with an injection prescribed | 0.00% |
Table 2: Details of prescribing indicators.
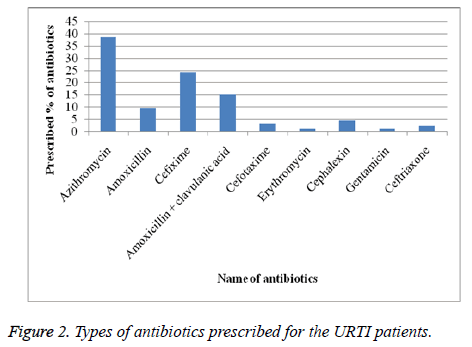
Azithromycin was the most common prescribed antibiotic with 38.66% (n=104) of total prescribed antibiotic followed by cefixime (24.16%), amoxicillin in combination with clavulanic acid (15.61%), amoxicillin (9.66%), cephalexin (4.46%), ceftriaxone (2.23%), erythromycin (1.11%) and gentamycin (1.11%) prescribed (Figure 2).
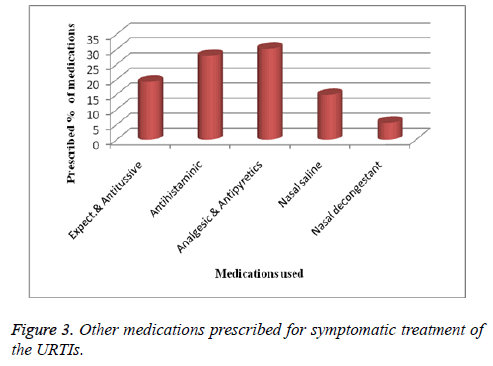
The results showed that the physicians also provided symptomatic treatment and prescribed 30.27% of total prescription in form of analgesics and antipyretics followed by antihistaminic (27.83%), expectorant (19.18%) and nasal decongestants (5.67%) (Figure 3).
Furthermore, regarding the route of administration of prescribed drugs, 95.6% of prescribed drug were found to be administered orally with syrup dosage forms being the most common dosage forms followed by tablet dosage forms. However, no medicine was prescribed for parenteral route of drug administration. The dose and frequency of the administered dosage forms was found to be varied according to the age of the patient as well as type of antibiotic or medication prescribed.
Discussion
This study investigated the drug utilization patterns for URTIs treatment among children referred to the pediatric unit of a major hospital in Najran, Kingdom of Saudi Arabia. It was prescription-based observational study which has been reported as an effective methodological design used by physicians to assess the prescribing pattern of medicine in URTIs among pediatrics. The WHO drug prescribing indicators was used to achieve the purpose of study. The adherence to these indicators can be used as feedback to monitor and help in encouraging rational drug treatment. It has been reported that lesser number of drug prescribed in prescription resulted into the increase in compliance, decreased risk of drug interactions and lower cost of therapy [22].
The majority (44.05%) of patients in current investigation were age of 0-2 y which resulted due to their poor development of immunity and more susceptible to infections. The similar trend of findings was reported by Sawalha et al. in their investigation on in-patients of URTIs (78%) while Joshi et al. reported on out-patients of URTIs (49%) having <5 y of age [23,24]. This study included a higher percentage of male children (53.24%) than females (46.77%). While sex is a significant epidemiological factor for several diseases, it does not seem to have a role in the development and outcome of a variety of infections, except for those of the urinary tract [25]. However, another study conducted in the United States reported that males are more susceptible to some types of URTIs in all age groups, including both adults and children [25].
In our study, an average, 2.24 drugs were prescribed per patient. Similar trend reported in studies conducted by Joshi et al. as well as Das et al. and found that the mean number of drugs per prescription to be 2.81 and 2.37 respectively [23,26]. The present investigation also found that >50% of total patients were prescribed with two or more medicines. This is mainly because of combination of cough syrups, analgesics and saline drop preparation are prescribed along with or without antimicrobials for the treatment of URTIs [27]. Uncomplicated URTIs ( like pharyngitis, sinusitis, bronchitis and otitis media) treated with antibiotics contributes to poor outcomes such as bacterial infections are thought to be the cause of the illness in a small number of cases, unnecessary and excessive use of antibiotic associated with side effects, allergic reactions and with broader consequences to society, including increased costs and bacterial resistance [28-31]. The result of this study showed that the practice of irrational use of antibiotic in the management of different URTIs in clinical settings. The prevalence of antibiotics prescribed in the treatment of URTIs was 72.7%. This rate was higher than the rates reported for the other developed and developing countries. In this regard, the proportion of URTIs treated with antibiotics was 68.4% in Malaysia, 67.5% in Saudi Arabia and 64% in Canada [1,32,33]. The main reason for the higher prevalence of antibiotic used in the treatment of URTIs could be the low level of awareness of antibiotic use among the prescribers. The high prescription rate of antibiotics was an important concern. This is because most of URTIs caused by viral agents and cases treated empirically. Therefore, the majority of the prescribed antibiotics for URTIs in the hospitals have been reportedly irrational [34,35].
A total of 9 types of antibiotics, mainly belong to four different classes (Penicillin, cephalosporin, macrolides, and aminoglycosides) were commonly used in the treatment of URTIs. The most frequently prescribed antibiotics were found to be macrolides class (39.77%.). However, Azithromycin was the most frequently prescribed antibiotics among the Macrolide class and account for 38.66% of total macrolide prescribed. Next to the macrolide, the other most frequently prescribed antibiotic was Cefixime and account for about 24.2% of total prescribed antibiotic. However, in Malaysia, penicillins were prescribed in 59.4% cases of URTIs while amoxicillin and ampicillin found to prescribe in 42.6% and 10.4% case of URTIs respectively [1]. A study conducted in Saudi Arabia reported prescribing pattern of penicillin specially amoxicillin and ampicillin and accounted for 50.5% of total antibacterial agents prescribed for URTIs cases [32]. A similar investigation conducted in India also reported the results in similar trends [36].
With regard to the frequency of prescription, the most commonly prescribed drugs in our study were the analgesics and antipyretics (paracetamol/ibuprofen) and account for 30.27% of the total prescribed drug. This result is expected since most of the children with URTIs may need an anti-pyretic agent because likely to have a fever. The other group of drugs commonly prescribed was anti-histamines with both first generation (diphenhydramine) as well as second generation anti-histamine (loratadine). Although they provide symptomatic relief, there is no convincing evidence that may shorten the duration of symptoms. The use of anti-histamine for the common cold reports very little literature evidence [37]. Few studies supported the preparations for cold to relieve symptoms of runny nose and sneezing in adolescents. However, it is not recommended for children younger than five years of age. In our study nasoclear drops were also very commonly used and has been found to reduce the symptoms in URTIs [24].
Combating URTIs by symptomatic treatment without antibiotics must be encouraged. Accurate diagnosis of the disease and its treatment requires main aspects of patient care and even more important in paediatrics. The most URTIs are viral in origin. Therefore, strict guidelines should be followed for prescribing the antibiotics.
Conclusion
In Saudi Arabia, approximately 43% of populations are under the age of 15 years old. Therefore, provision of appropriate healthcare to this population indirectly reflects the healthcare set-up of the country [38]. The present observational study was conducted to determine the drug utilization pattern in pediatric patients suffering from URTIs. Paracetamol and anti-histamines were found to be the most common prescribed drugs and confirm to the rational prescribing practices in URTIs. However, prescribed antibiotics in present investigation and accounted for 72.7% of total prescribed drug URTIs, which is too high. The treatment pattern of URTIs in the Hospital shows the presence of irrational administration of antibiotics with high prevalence of overall antibiotic prescribed. Rational drug utilization needs training and education of doctors and other health care professionals to ensure appropriate therapy. There is a need for education of doctors, patients and parents regarding the risk-benefit of antibiotics or other drugs for the self-limiting condition. The present investigations are regularly needed to study the drug prescribing practices so that appropriate criticism and awareness will be generated. Moreover, prescribing patterns also reflects the capability of prescriber in terms of choosing such drugs which are prescribing safe, effective and affordable drugs that give maximum benefit to the patients. Thus, to ensure the rationality of the prescribed therapy, time to time prescription monitoring is important as changes in health related behavior usually take longer to achieve. The findings of this study highlight the important strategies to optimize the rationale use of medication for URTIs in paediatric and helped to establish the prescribing pattern.
Acknowledgements
The authors are thankful to the Deanship of Scientific Research and all health care professionals of Najran University Hospital, Najran, KSA for their valuable support.
Conflict of Interest
Authors have no conflict of interest on publishing this paper.
References
- Cheong LT, Kwok CL, Syed MA, Molly C. Antibiotic prescription in upper respiratory tract infections, Asia Pac Fam Med 2004; 3: 38-45.
- Karen C, Larry R. Microbiology and laboratory diagnosis of upper respiratory tract infections. Clin Infect Dis 996; 23: 442-81.
- Behrman RE, Kliegman RM, Jenson HB. Infection of upper respiratory tract. Nelson Textbook of Paediatrics. W.B. Saunders Company, Philadelphia 2000; 1261.
- Feld LG, Hyams JS. Respiratory tract infections in children: new developments in in diagnosis and treatment. Cons Pediatr 2009; 1: 1-46.
- Schappert SM. Vital health statist. Maryland: National Centre for Health Statistics 1994; 13.
- Tom F, Nigel S, Toby T. Systematic review of the treatment of upper respiratory tract infection. Arc Dis Child 1998; 79: 225-230.
- Susan SH, Sheryl LR, Ken K, Jamie K, Nancy S, Christopher JS, Ron S, Jonathan AF. Parental knowledge about antibiotic use: results of a cluster-randomized, multi community intervention. Pediatrics 2007; 119: 698-706.
- Scott JG, Cohen D, DiCicco-Bloom B, Orzano AJ, Jaen CR, Crabtree BF. Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Pract 2001; 50: 853-858.
- Belongia EA, Naimi TS, Gale CM, Besser RE. Antibiotic use and upper respiratory infections: a survey of knowledge, attitudes, and experience in Wisconsin and Minnesota. Prev Med 2002; 34: 346-352.
- Cebotarenco N, Bush PJ. Reducing antibiotics for colds and flu: a student-taught program, Health Educ Res 2008; 23: 146-157.
- Jain N, Lodha R, Kabra SK. Upper respiratory tract infections. Ind J Pediatr 2001; 68: 1135-1138.
- Rosenstein N, Phillips WR, Gerber MA, Marcy SM, Schwartz B, Dowell SF. The common cold Principles of judicious use of antimicrobial agents. Pediatrics 1998; 101: 181-184.
- Richer M, Deschenes M. Upper respiratory tract infections; pharmacotherapy and pathological approach (5th Edn.) 2015; 1869-1872.
- Loureiro A, Cristovao A, Caria T. Between external prescription and local practice. The uses of official knowledge by adult education professionals in Portugal. Eur J Res Educ Learn Adults 2013; 4: 65-80.
- Karande S, Sankhe P, Kulkarni M. Patterns of prescription and drug dispensing. Indian J Pediatr 2005; 72: 117-121.
- Nandimath MK. Drug prescribing pattern in upper respiratory tract infection in children aged 1-14 years. Int J Pharm Biol Sci 2012; 3: 299-308.
- Dhamija P, Bansal D, Srinivasan A, Bhalla A, Hota D, Chakrabarti A. Patterns of prescription drug use and incidence of drug-drug interactions in patients reporting to medical emergency. Fund Clinic Pharmacol 2013; 27: 231-237.
- Dowell SF, Schwartz B, Phillips WR. Appropriate use of antibiotics for URIs in children: Part I. Otitis media and acute sinusitis. The Pediatric URI Consensus Team. Am Fam Phys 1998; 58: 1113-1118.
- Dowell SF, Schwartz B, Phillips WR. Appropriate use of antibiotics for URIs in children: Part II. Cough, pharyngitis and the common cold. The Pediatric URI Consensus Team. Am Fam Phys 1998; 58: 1335-1342.
- Watson RL, Dowell SF, Jayaraman M, Keyserling H, Kolczak M, Schwartz B. Antimicrobial use for pediatric upper respiratory infections: reported practice, actual practice, and parent beliefs. Pediatrics 1999; 104: 1251-1257.
- Joseph N, Bharathi DR, Sreenivasa B, Nataraj GR, George N, Safdar M. Prescribing pattern of drugs in upper respiratory tract infections in pediatric out patients. Int J Contemp Pediatr 2016; 3: 1006-1008.
- Sharma S, Agrawal G. A study on drug prescribing pattern in upper respiratory tract infections among children aged 1-12 years. Int J Bas Clin Pharmacol 2016; 5: 406-410.
- Joshi U, Hishikar R, Agrawal S, Halwai A, Kirtania L, Kurrey K. Study of drug use in outdoor pediatric patients of upper respiratory tract infections in a tertiary care hospital. Int J Bas Clin Pharmacol 2015; 4: 1004-1008.
- Sawalha A, Al-Bishtawi G, Al-Khayyat L, Sweileh W, Al-Ramahi R, Jaradat N. Pattern of parenteral antimicrobial prescription among paediatric patients in Al-Watani Government Hospital in Palestine. An-Najah Univ J Res 2006; 20: 191-206.
- Falagas ME, Mourtzoukou EG, Vardakas KZ. Sex differences in the incidence and severity of respiratory tract infections. Resp Med 2007; 101: 1845-1863.
- Das B, Sarkar C, Majumder AG. Medication use for pediatric upper respiratory tract infections. Fund Clin Pharmacol 2006; 20: 385-390.
- NICE. Respiratory tract infections-Antibiotic prescribing. Prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care. National Institute of Health and Clinical Excellence, London, UK 2008; 1-122.
- Smith SS, Kern RC, Chandra RK, Tan BK, Evans CT. Variations in antibiotic prescribing of acute rhinosinusitis in United States ambulatory settings. Otolaryngol Head Neck Surg 2013; 148: 852-859.
- Roumie CL, BHalasa N, Edwards KM, Zhu Y, Dittus RS, Griffin MR. Differences in antibiotic prescribing among physicians, residents, and nonphysician clinicians. Am J Med 2005; 118: 641-648.
- Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. J Am Med Assoc (JAMA) R 2003; 289: 719-725.
- Smith WM, Davidson TM, Murphy C. Regional variations in chronic rhinosinusitis, 2003-2006. Otolaryngol Head Neck Surg 2009; 141: 347-352.
- Irshaid YM, Al-Homrany MA, Hamdi AA. A pharmacoepidemiological study of prescription pattern for upper respiratory infections in a tertiary health care center. Saudi Med J 2005; 26: 1649-1651.
- Elinski S, Parfrey P, Hutchinson J. Antibiotic utilisation in community practices: guideline concurrence and prescription necessity. Pharmacoepidemiol Drug Safety 2005; 14: 319-326.
- National Institute for Health and Clinical Excellence/NHS/. Respiratory tract infections-antibiotic prescribing. Prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care. NICE Clinical Guideline 2008; 69.
- Arnold SR, To T, McIsaac WJ, Wang EE. Antibiotic prescribing for upper respiratory tract infection: the importance of diagnostic uncertainty. J Pediatr 2005; 146: 222-226.
- Joseph N, Bharathi DR, Sreenivasa B, Nataraj GR, George N, Safdar M. Prescribing pattern of drugs in upper respiratory tract infections in pediatric out patients. Int J Contemp Pediatr 2016; 3: 1006-1008.
- Luks D, Anderson MR. Antihistamines and the common cold; a review and critic of the literature. J Gene Int Med 1996; 11: 240-244.
- Park K. Preventive medicine in obstetrics, paediatrics and geriartics. Park’s Textbook of Preventive and Social Medicine (23rd edn.) 2015.