Research Article - Biomedical Research (2017) Volume 28, Issue 7
Core decompression with bone grafting combined with arterial perfusion in treating early osteonecrosis of the femoral head
Da-Shou Wang1*, Qian Chen1, Feng-Jun Cai3, Ben-Sen Tang2, Qi Pan1 and Meng He11Department of Pain Medicine, Guizhou Provincial Orthopedics Hospital, Guiyang, PR China
2Department of Orthopedics, Guizhou Provincial Orthopedics Hospital, Guiyang, PR China
3Department of Pain Medicine and Intervention, Xixiu District People’s Hospital, Anshun, PR China
- *Corresponding Author:
- Da-Shou Wang
Department of Pain Medicine
Guizhou Provincial Orthopedics Hospital, PR China
Accepted on December 26, 2016
Abstract
This study aims to evaluate the clinical efficacy of core decompression with bone grafting combined with perifemoral arterial infusion (CDBG-AI) in treating stage I-II osteonecrosis of the femoral head (ONFH). A total of 40 patients (40-70 years old) with stage I-II ONFH were enrolled. Initially, these patients underwent core decompression plus implantation of allogeneic bone and CaSO4 particles; 5-7 days later, they received arterial perfusion of a thrombolytic drug and vasodilator into the exterior and interior femoral circumflex arteries, obturator artery, and inferior gluteal artery; the perfusion was repeated at the 3rd, 6th, and 12th postoperative month. Imaging changes in the femoral head were observed 1 year later; the visual analogue score (VAS) was used to evaluate symptom improvement, and the Harris score was used to evaluate function. Among the 40 patients, signs of necrosis disappeared in four cases, 32 cases showed no changes on imaging, and four cases progressed to stage III; the VAS scores showed symptom relief in 36 cases, but four cases showed either no relief or aggravated symptoms; the Harris scores showed improvement in 36 cases, and worsening condition in four cases. Routine CDBG-AI could effectively improve the prognosis of less than stage II ONFH and delay its progression.
Keywords
Osteonecrosis of the femoral head, Core decompression, Arterial perfusion therapy.
Introduction
Osteonecrosis of the femoral head (ONFH) is a devastating multifactorial disease that affects 20,000 persons each year in the United States [1]. Although the etiology of ONFH has not been definitely delineated, the risk factors include corticosteroid administration, alcohol consumption, trauma, and coagulation abnormalities [2]. In 2003, as one of the important treatments for severe acute respiratory syndrome (SARS), high-dose corticosteroid therapy also caused many cases of ONFH, which then was defined as a severe sequela of SARS. A retrospective study, which included 539 cases, revealed that 24% of the patients administered corticosteroid therapy was diagnosed with ONFH [3].
According to the suggestions of the Association Research Circulation Osseous (ARCO) [4], ONFH can be divided into 5 stages: in stage 0-stage II, patients mostly have mild to moderate pain with imageological changes; however, in stage III-stage IV, collapse of the femoral head is typical, and ultimately requires a standard total hip arthroplasty (THA) [5].
In the past, patients with less than stage II ONFH received medication and closed treatment to relieve pain; many treatments have been developed, including pharmacologic agents and physical therapy. Among the pharmacologic agents, statins were used in the early 21st century [6,7], followed by anticoagulants [8,9], prostacyclin [10,11], bisphosphonates (Bps) [12-14], aspirin (which was found to be able to prevent disease progression in young adults in one prospective cohort [15]), and osteonecrosis (which might be a promising therapy for early stages) [16]. Physical therapy is also used to improve prognosis in ONFH; extracorporeal shock-wave therapy (ESWT) [14] and electromagnetic therapy [17] both showed effectiveness in early ONFH due to increased ingrowth of neovascularization and new bone formation. Hyperbaric oxygen treatment is also effective in preserving the hip joint in stage I and II ONFH [18].
Based on prior studies, we used core decompression plus artificial bone implantation, followed by routine perfusion of an antispasmodic and vasodilator as well as thrombolytic therapy in the FH arterial blood supply, aiming to both reduce the pressure on the femoral head and to improve the FH blood supply. The study achieved certain effects as reported herein.
Methods and Materials
Clinical data
Inclusion criteria: patients with hip pain, limited range of motion, and aggravated condition because of climate change; inguinal midpoint tenderness, and a positive test; computed tomography (CT) showing no stenosis in cystic joint spaces; magnetic resonance imaging (MRI) with abnormal signals in the FH burdening area; articular cavity hydrops greater than on the healthy side; normal erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) level, and white blood cell counts; and visual analogue score (VAS): 4-6 points. Exclusion criteria: patients with peri-hip bone a cell counts, and signs of infection or tuberculosis when the neutral region was >70%.
A total of 40 patients with stage I-II ONFH confirmed by symptoms, signs, and imaging results at our department from January 2009 to December 2013 were included. Twenties seven patients are stage I and seventeen patients are stage II in total forty patients, the patients were 40-70 years old and included 18 male and 22 female patients; disease causes: 12 cases of hormone use, 10 cases of alcohol consumption, six cases of sprains, and 12 cases of unknown cause. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of X Provincial Orthopedics Hospital. Written informed consent was obtained from all participants.
Core decompression
The patient first underwent continuous epidural anesthesia, and was then placed in position with the uninjured limb on top and flexed and with the injured limb straight; a C-arm position-guided knife was then used to make a 4 mm incision about 3 cm under the greater femoral trochanter. A solid-center 4 mm bone drill was then used to break the cortical bone; a puncture needle core was then inserted and progressed to the base of the femoral neck; a hollow drill was then used to continue drilling the necrotic base until live cancellous bone was removed. Finally, the solid-center drill was used to drill the necrotic tissue until the subchondral bone was reached; the cancellous bone inside the hollow drill was then implanted into the subchondral bone, and gelatin sponge was used to fill the remaining bone puncture channel after CaSO4 particles and allogeneic bone were implanted.
Perfusion of femoral blood supply artery
The uninjured femoral artery was first punctured and a 5 F arterial sheath was inserted; a C3 opacification catheter was used to penetrate into the opposite side. A Terumo microcatheter was then used to super selectively penetrate to the exterior femoral circumflex artery, medial femoral circumflex artery, and obturator artery; 30 mg of papaverine, 20 mg of alprostadil, 80 mg of sodium ozagrel, and 200,000 U of urokinase were diluted in 120 ml and pumped into the above three arteries (40 ml, 30 ml, and 20 ml, respectively). The remaining 30 ml was pumped into the gluteal artery.
Observation indicators
MRI and CT were performed to observe imaging changes of the FH at the 6th and 12th postoperative month; the VAS scoring system was used to evaluate pain relief at the 1st week, 3rd month, 6th month, and 12th month postoperatively; the Harris scoring system was used to evaluate hip function at the 1st week, 3rd month, 6th month, and 12th month postoperatively.
Statistical analysis
SPSS 16.0 software was used for statistical analysis. The counting data were analyzed using the t test; the measurement data were expressed as mean ± standard deviation, using the chi-square test, with α=0.05 and P<0.05 considered as a statistical difference and P<0.01 as a statistically significant difference.
Results
Observation indicators
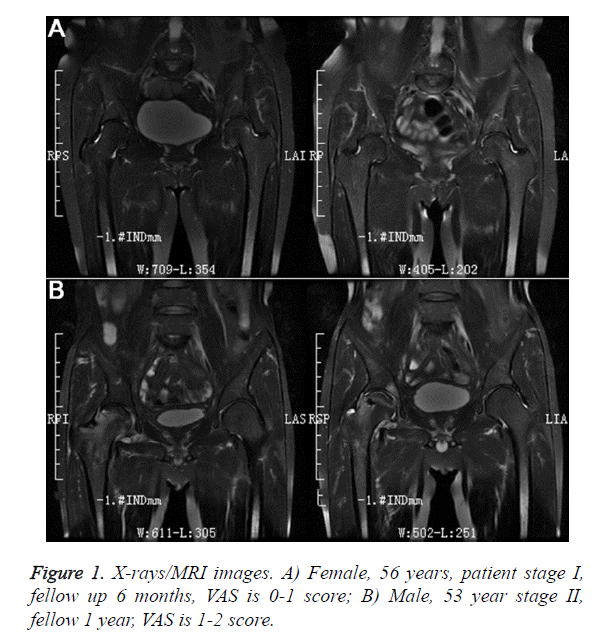
The observation indicators are shown in Table 1. The MRI results showed improvement in 4 cases and remained stable in 32, while in the other 4 cases, progression was shown at 6 and 12 months of follow-up; the Harris function score improved within 1 week postoperatively, and remained stable for the entire year; the change in VAS score was similar, showing improvement within 1 week postoperatively, and remained stable for the next 12 months (Figure 1).
| Indicator | Before surgery | Postoperative 1st week | Postoperative 3rd month | Postoperative 6th month | Postoperative 12th month |
|---|---|---|---|---|---|
| MRI | 40 | - | - | 36 (0.90) | 36 (0.90) |
| Harris | 54 ± 7 | 73 ± 12* | 82 ± 10* | 79 ± 9* | 80 ± 11* |
| VAS | 5 ± 1.5 | 2 ± 1.1* | 2 ± 1.5* | 2 ± 1.3* | 2 ± 1.5* |
| Note: *P<0.05, compared with before surgery. | |||||
Table 1. Changes of femoral head during treatment, including MRI/Harris/VAS.
Statistical analysis
The Harris scores exhibited statistically significant increases at the 1st week, 3rd month, 6th month, and 12th month postoperatively, compared to the scores before surgery (P<0.01); the scores remained stable after the 3rd postoperative month, with an increase compared to the 1st postoperative week; however, the difference was not statistically significant (P>0.05). Compared with severity before surgery, pain in the 1st week, 3rd month, 6th month, and 12th month postoperatively was significantly alleviated, and the difference was statistically significant (P<0.01). The disease remained stable after surgery, and pain showed no significant recurrence after relief; the difference showed no statistical significance (P>0.05).
Discussion
ONFH is a progressive disease characterized by reduced local blood flow and death of osteocytes and bone marrow [19], and can lead to persistent destruction of bone architecture, subchondral fracture, extensive hip pain, and loss of joint function [20]. Several studies indicated that hemostatic abnormalities caused by administration of corticosteroids were related to the development of ONFH [21]. Vasospasm and blood flow reduction, particularly microcirculation flow reduction, could cause microvascular thrombosis, venous reflux pressure reduction, reflux disorder, oxygen supply reduction, FH metabolic rate reduction, anaerobic metabolism enhancement, and metabolic product-elimination disorder; these cause increased pressure in the FH and create a vicious cycle, followed eventually by avascular necrosis of the FH [22]. Therefore, relieving FH vascular spasm, dilating blood vessels, and increasing vascular perfusion pressure could improve blood flow in the femoral head.
One study showed that core decompression via multiple small drill holes could allow postoperative load-bearing with similar or even better clinical outcomes without prolonged use of an expensive tantalum implant [23]; this was consistent with the findings of a meta-analysis including four randomized controlled trials and two controlled clinical trials of 323 hips with 24-48 months of follow-up, suggesting that core decompression showed a trend toward favorable results, in contrast to other conservative treatment. This could be effective for preventing femoral collapse during short-term follow-up, but an even higher success rate could be expected with biophysical stimulation [24]. Consistent with the above studies, not only core decompression but also simultaneous implantation of cancellous bone, allogeneic bone, and CaSO4 could stimulate angiogenesis. One study enrolled 10 patients for mesenchymal stromal cell transplantation, and thereafter demonstrated the feasibility and safety of a multiplex rehabilitation program [25].
After the pressure was reduced, the vicious cycle of femoral head necrosis could be broken, thus promoting the gradual elimination of metabolites [26]. From this observation, it was apparent that pain was significantly relieved after core decompression, and hip function improved; after arterial injection of high concentrations of an anticoagulant, a vasodilator, and a thrombolytic drug, the blood circulation in the femoral head was further improved, the oxygen supply improved, metabolism increased, and new blood vessels were induced. The clinical efficacy was stable. This observation also revealed that the postperfusion efficacy was relatively stable after core decompression. However, the reasons for ONFH vary, especially in trauma-induced ONFH; whether trauma caused organic injury in the FH blood vessels remained unclear. Furthermore, smoking and drinking habits in some patients were not completely corrected after surgery, with continued damage to microvessels; finally, the conditions in elderly patients were partially related to atherosclerosis. All the above factors might lead to poor outcomes and even further aggravation. Among the four aggravated cases of ONFH, one patient initially exhibited pain relief, but progressed to stage III and required femoral head replacement due to continued heavy drinking. Two cases had persistent pain after trauma; after core decompression, the pain was briefly relieved but the condition became aggravated and progressed. One patient was older than 70 years; pain worsened after core decompression, and a secondary femoral neck fracture occurred. Some studies adopted a porous tantalum rod combined with endoscopy, curettage, autologous bone grafting, and bone marrow aspiration from the iliac crest; among 49 patients (58 hips), 38 hips were in stage II, and no patient developed a serious intraoperative or postoperative complication; the 5-year survival based on conversion to THA was 93.1%, and the rate based on disease progression was 87.9%, which was an encouraging outcome [27].
Limitations
Because the number of clinical cases was small, with a large age range and complex comorbidities, efficacy requires on-going monitoring.
References
- Luo RB, Lin T, Zhong HM, Yan SG, Wang JA. Evidence for using alendronate to treat adult avascular necrosis of the femoral head: a systematic review. Med Sci Monit 2014; 20: 2439-2447.
- Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 2014; 22: 455-464.
- Guo KJ, Zhao FC, Guo Y, Li FL, Zhu L, Zheng W. The influence of age, gender and treatment with steroids on the incidence of osteonecrosis of the femoral head during the management of severe acute respiratory syndrome: a retrospective study. Bone Joint J 2014; 96-B: 259-262.
- Sun W, Wang BL, Li ZR; Association Research Circulation Osseous (ARCO). Chinese specialist consensus on diagnosis and treatment of osteonecrosis of the femoral head. Orthop Surg 2011; 3: 131-137.
- Mont MA, Seyler TM, Marker DR, Marulanda GA, Delanois RE. Use of metal-on-metal total hip resurfacing for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am 2006; 88: 90-97.
- Pritchett JW. Statin therapy decreases the risk of osteonecrosis in patients receiving steroids. Clin Orthop Relat Res 2001; 386: 173-178.
- Wang GJ, Cui Q, Balian G. The Nicolas Andry award. The pathogenesis and prevention of steroid-induced osteonecrosis. Clin Orthop Relat Res 2000; 370: 295-310.
- Wang Y, Yin L, Li Y, Liu P, Cui Q. Preventive effects of puerarin on alcohol-induced osteonecrosis. Clin Orthop Relat Res 2008; 466: 1059-1067.
- Glueck CJ, Freiberg RA, Sieve L, Wang P. Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin Orthop Relat Res 2005; 435: 164-170.
- Jager M, Tillmann FP, Thornhill TS, Mahmoudi M, Blondin D, Hetzel GR, Zilkens C, Krauspe R. Rationale for prostaglandin I2 in bone marrow oedema-from theory to application. Arthritis Res Ther 2008; 10: R120.
- Disch AC, Matziolis G, Perka C. The management of necrosis-associated and idiopathic bone-marrow oedema of the proximal femur by intravenous iloprost. J Bone Joint Surg Br 2005; 87: 560-564.
- Chen CH, Chang JK, Lai KA, Hou SM, Chang CH, Wang GJ. Alendronate in the prevention of collapse of the femoral head in nontraumatic osteonecrosis: a two-year multicenter, prospective, randomized, double-blind, placebo-controlled study. Arthritis Rheum 2012; 64: 1572-1578.
- Young ML, Little DG, Kim HK. Evidence for using bisphosphonate to treat Legg-Calve-Perthes disease. Clin Orthop Relat Res 2012; 470: 2462-2475.
- Vulpiani MC, Vetrano M, Trischitta D, Scarcello L, Chizzi F, Argento G, Saraceni VM, Maffulli N, Ferretti A. Extracorporeal shock wave therapy in early osteonecrosis of the femoral head: prospective clinical study with long-term follow-up. Arch Orthop Trauma Surg 2012; 132: 499-508.
- Albers A, Carli A, Routy B, Harvey EJ, Séguin C. Treatment with acetylsalicylic acid prevents short to mid-term radiographic progression of nontraumatic osteonecrosis of the femoral head: a pilot study. Can J Surg 2015; 58: 198-205.
- Dong Y, Li Y, Huang C, Gao K, Weng X. Systemic application of teriparatide for steroid induced osteonecrosis in a rat model. BMC Musculoskelet Disord 2015; 16: 163.
- Windisch C, Kolb W, Röhner E, Wagner M, Roth A, Matziolis G, Wagner A. Invasive electromagnetic field treatment in osteonecrosis of the femoral head: a prospective cohort study. Open Orthop J 2014; 8: 125-129.
- Koren L, Ginesin E, Melamed Y, Norman D, Levin D, Peled E. Hyperbaric oxygen for stage I and II femoral head osteonecrosis. Orthopedics 2015; 38: e200-205.
- Seamon J, Keller T, Saleh J, Cui Q. The pathogenesis of nontraumatic osteonecrosis. Arthritis 2012; 2012: 601763.
- Mont MA, Seyler TM, Plate JF, Delanois RE, Parvizi J. Uncemented total hip arthroplasty in young adults with osteonecrosis of the femoral head: a comparative study. J Bone Joint Surg Am 2006; 88: 104-109.
- Tektonidou MG, Malagari K, Vlachoyiannopoulos PG, Kelekis DA, Moutsopoulos HM. Asymptomatic avascular necrosis in patients with primary antiphospholipid syndrome in the absence of corticosteroid use: a prospective study by magnetic imaging. Arthritis Rheum 2003; 48: 732-736.
- Moriya M, Uchiyama K, Takahira N, Fukushima K, Yamamoto T, Hoshi K, Itoman M, Takaso M. Evaluation of bipolar hemiarthroplasty for the treatment of steroid-induced osteonecrosis of the femoral head. Int Orthop 2012; 36: 2041-2047.
- Miao H, Ye D, Liang W, Yao Y. Effect of Osteonecrosis Intervention Rod Versus Core Decompression Using Multiple Small Drill Holes on Early Stages of Necrosis of the Femoral Head: A Prospective Study on a Series of 60 Patients with a Minimum 1-Year-Follow-Up. Open Orthop J 2015; 9: 179-184.
- Hong YC, Zhong HM, Lin T, Shi JB. Comparison of core decompression and conservative treatment for avascular necrosis of femoral head at early stage: a meta-analysis. Int J Clin Exp Med 2015; 8: 5207-5216.
- Aoyama T, Fujita Y, Madoba K, Nankaku M, Yamada M, Tomita M, Goto K, Ikeguchi R, Kakinoki R, Matsuda S, Nakamura T, Toguchida J. Rehabilitation program after mesenchymal stromal cell transplantation augmented by vascularized bone grafts for idiopathic osteonecrosis of the femoral head: a preliminary study. Arch Phys Med Rehabil 2015; 96: 532-539.
- van der Jagt D, Mokete L, Pietrzak J, Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 2015; 23: 69-70.
- Pakos EE, Megas P, Paschos NK, Syggelos SA, Kouzelis A, Georgiadis G, Xenakis TA. Modified porous tantalum rod technique for the treatment of femoral head osteonecrosis. World J Orthop 2015; 6: 829-837.