Research Article - Journal of Medical Oncology and Therapeutics (2016) Volume 1, Issue 1
Concordant Versus Discordant Ultrasound Guided Breast Biopsy Results: How They Effect Patient Management?
Imrana Masroor*, Saira Naz Sufian, Shaista Afzal, Saba Sohail, Hafsa Qayyum
Department of Radiology Aga Khan University Hospital Karachi, Pakistan.
- *Corresponding Author:
- Imrana Masroor
Radiology Department, Aga Khan University Hospital
Karachi, Pakistan.
Tel: +09203008287762
E-mail: imrana.masroor@aku.edu
Accepted date August 23, 2016
DOI: 10.35841/medical-oncology.1.1.24-29
Visit for more related articles at Journal of Medical Oncology and TherapeuticsAbstract
Background: To determine concordant or discordant breast biopsy results and see their effect on patient management and outcome.
Material and methods: This descriptive analytical study was conducted at the department of Diagnostic Radiology Aga Khan University Hospital Karachi Pakistan from January to December 2013. All patients fulfilling our selection criteria were included. A concordant result was defined when the imaging and pathology results concluded same diagnosis and a discordant result when they did not match. All histopathology results were reviewed and a decision was made regarding concordant/discordant biopsy results and recommendations given for further management of all patients.
Results: A total of 282 patients underwent core biopsy of lesions in the breast. The mean age was 47.87 ± 13.99 years. Out of 282 lesions biopsied, 172 were concordant malignant and 105 were concordant benign. Two lesion out of 282 were borderline or high risk, one case was discordant benign and 2 cases discordant malignant. The appropriate management for all cases was recommended after radiology-pathology correlation.
Conclusion: Cautious Radiology-Pathology co relation is indispensable in addition to appropriate post biopsy management for managing a successful core breast biopsy program. This practice identifies a substantial number of false negative results of core biopsy by identifying discordant results avoiding delays in diagnosis of breast cancer.
Keywords
Concordant breast biopsy, Discordant breast biopsy, Breast carcinoma, Management
Introduction
Despite an acceptable accuracy of mammography, it is vital to obtain a tissue diagnosis of breast cancer before proceeding for definitive management and surgery [1,2]. Even though fine needle aspiration cytology (FNAC) is initially the first method of biopsy at many centers [1,2] it is not reliable and is prone to sampling errors [2]. The gold standard for diagnosis is surgical biopsy but it is associated with morbidity, high cost, aesthetic problems and interference with definite surgery for cancer [2,3] therefore it is not the initial biopsy method of choice. Image guided percutaneous Core Needle Biopsy (CNB) could avoid all the previously stated limitations, and decrease any post-operative scarring that may hinder diagnostic accuracy of a mammogram [4]. When possible image guided CNB has become accepted as an alternative to surgical biopsy for the diagnosis of non- palpable image detected lesions. It is less invasive, more cost effective [5-8], and has a lower complication rate than open surgical biopsy [9].
The success of an image guided core breast biopsy depends on the post biopsy management as well as the performance of the biopsy procedure [10]. A core biopsy may fail to sample the targeted lesion, resulting in benign histopathology result, despite optimization of technique [11]. Even though there are methods such as specimen radiography or post biopsy mammography to confirm lesion retrieval after performing a core biopsy, they often provide incomplete information, especially in lesions visualized.
The purpose of this study was to calculate concordance and discordance of imaging and pathology results among selected sample size after an ultrasound guided core biopsy, and to discuss selected cases for discordant results, which will help in providing guidance for further future management.
Materials and Methods
The study was conducted at Radiology Department of Aga Khan University Hospital. It was a descriptive analytical study and all patients who underwent breast biopsy under ultrasound guidance during the study period were included. The study period was between Januarys to December 2013. Exemption was granted from Ethical Review Committee of Aga Khan University Hospital (ERC # 3179-Rad-ERC-14). All patients had consented to for core biopsy and had signed the pre-designed hospital consent form. They were counseled in detail by the primary surgeon as well as the radiologist before the performance of procedure about the nature of biopsy the method and its purpose and all associated complications.
The inclusion criteria were a lesion reported as BI-RADS category 3, 4 or 5 on ultrasound or BIRADS 2 if the biopsy was requested by referring breast surgeon. The exclusion criteria were patients with incomplete medical records, those patients whose imaging and biopsy was done from here but they had histopathology from outside or those patients who had imaging and biopsy from here and further management was done outside the institution.
Functional Definitions of Concordance/Discordance
The imaging and pathology concordance is considered when the pathology results provided an acceptable explanation for the imaging features and discordant when they do not.
Pariek and Tickman [12] have described 5 categories, of imaging pathology correlation and suggested corresponding managements.
Category 1: Concordant malignancy
Lesion has malignant features on imaging (Breast Imaging Reporting and Data System {BI-RADS} category 4 or 5) and is confirmed as malignancy on histopathology is a concordant malignancy in this scenario appropriate action should be taken without delay. The radiologist should inform the referring physician of the results and the patient should be informed and referred to a surgeon or oncologist for further management.
Category 2: Discordant malignancy
A lesion with benign imaging features (i.e., BI-RADS category 2 or 3) but proves to be malignant at core biopsy falls into this category; management should be done as for a concordant malignancy.
Category 3: Concordant benign
A lesion with benign features on imaging (i.e.BI-RADS CATEGORY 2, 3 or 4a) and shows benign histopathology is included. In this case a follow up ultrasound will be recommended because of delayed false negative results after core biopsy.
Category 4: Discordant benign
A lesion suspicious for malignancy at imaging (i.e., BIRADS category 4 or 5), but shows benign pathologic results after core biopsy. The findings are discussed with referring physician and pathologist, a repeat biopsy in form of open surgical biopsy should be done.
Category 5: Border line or high risk
The biopsied lesion is not malignant but has an increased life time risk of malignancy like atypical ductal hyperplasia, lobular neoplasm, etc. a case to case approach should be done and a surgical biopsy should be recommended regardless of concordance, because of relatively high upgrade rate to malignancy.
All ultrasound scans were performed on Aplio 400 with a linear high frequency probe by a radiologist with more than 5 years of experience in breast imaging. All biopsies were performed using local anesthesia with a 14 G automated gun, on average 3 to 5 cores were taken from every lesion and the samples were sent to histopathology. Using open Epi a sample size of 231 was calculated using breast cancer prevalence of 28.4% with 95% confidence interval and 80% study power. For each lesion the side, site and size was recorded and frequencies were calculated. The imaging findings were correlated with histopathology results. The management of all discordant lesions based on imaging criteria will be discussed. Statistical analysis was done on SPSS version.
Results
A total of 282 breast lesions were biopsied. The mean age was 47.87 ± 13.99 years. The patients presenting complaints are given in Table 1. It shows that maximum number of patient (91.5%) presented with breast lumps. The distribution of lesion according to side and quadrant within each breast is tabulated in Table 2; majority of patients had abnormal findings in upper outer quadrant (46.5) and predominantly in right breast (53.5%). All lesion underwent ultrasound examinations and their ultrasound characteristics were recorded (Table 3).
| S.No. | Clinical Indication | n (%) |
|---|---|---|
| 1 | Routine Checkup | 8 (2.8) |
| 2 | Lump | 258(91.5) |
| 3 | Nipple Discharge | 8(2.8) |
| 4 | Family History | 8(2.8) |
Table 1. The patients presenting complaints
| S.No. | Distribution of Lesions | n (%) |
|---|---|---|
| 1 | Right Breast | 151(53.5) |
| 2 | Left Breast | 131(46.1) |
| 3 | Upper Outer Quadrant | 131(46.5) |
| 4 | Lower Upper Quadrant | 25(8.9) |
| 5 | Upper Inner Quadrant | 97(34.4) |
| 6 | Lower Inner Quadrant | 29(10.3) |
Table 2.Distribution of lesion according to side and quadrant within each breast
| S.No. | Ultrasound Characteristics | n (%) |
|---|---|---|
| A | Texture | |
| 1 | Hypoechoic | 234 (83) |
| 2 | Isoechoic | 4 (1.4) |
| 3 | Hyperechoic | 8 (2.8) |
| 4 | Hyperechoic | 36 (12.8) |
| B | Margins | |
| 1 | Well defined | 73(25.9) |
| 2 | Lobulated | 36(12.8) |
| 3 | Ill defined | 47(16.7) |
| 4 | Irregular | 106 (37.6) |
| 5 | Spiculated | 20 (7.1) |
Table 3.Ultrasound examinations and their ultrasound characteristics
Out of 282 biopsies, there were 172 concordant malignant. All underwent definitive treatment in the form of breast conservation or mastectomy followed by radiotherapy and chemotherapy depending upon the staging of disease. Concordant benign were 105, out of which 3 were reported as BIRADS II however the clinician wanted surety about their benign nature because of family history of breast cancer or age of patient. In one of BIRADS II case patient wanted to establish benignity of the lesion. The remaining 102 were reported as BIRADS III (n=50) or 4a (n=52). After biopsy results all the images were reviewed or patients were recalled for a second look ultrasound by radiologist, all of them were than categorized as concordant benign. All the 102 lesions were reported on histopathology as benign fibrocystic changes or fibroadenomas. All the 102 lesions were followed by ultrasound at six month and then at one year to establish their benignity.
There were two cases labeled as high risk one was reported as borderline phylloides and second as suspicious for phylloides on histopathology and we recommended an excision biopsy. Both lesions underwent excisional biopsy and were reported on subsequent histopathology as phylloides both patients were kept on close follow up for 18 months with ultrasound even after excision to watch for recurrence.
Out of remaining three cases, one was reported as discordant benign and the other two as discordant malignant. In the case reported as discordant benign patient was status lumpectomy two years back for malignant lump, she had been given radiotherapy and chemotherapy. On ultrasound a hypoechoic irregular area was found at 12 o'clock position in right breast measuring 12 × 11 mm, the lumpectomy was done from upper outer quadrant of right breast. The histopathology showed benign fibrosis patient was recalled for a second biopsy, on relook ultrasound of the area found at 12 O’ clock, ultrasound showed that it was continuous with the scar edge so a re-biopsy was not performed and patient was put on close follow up for 18 months with ultrasound.
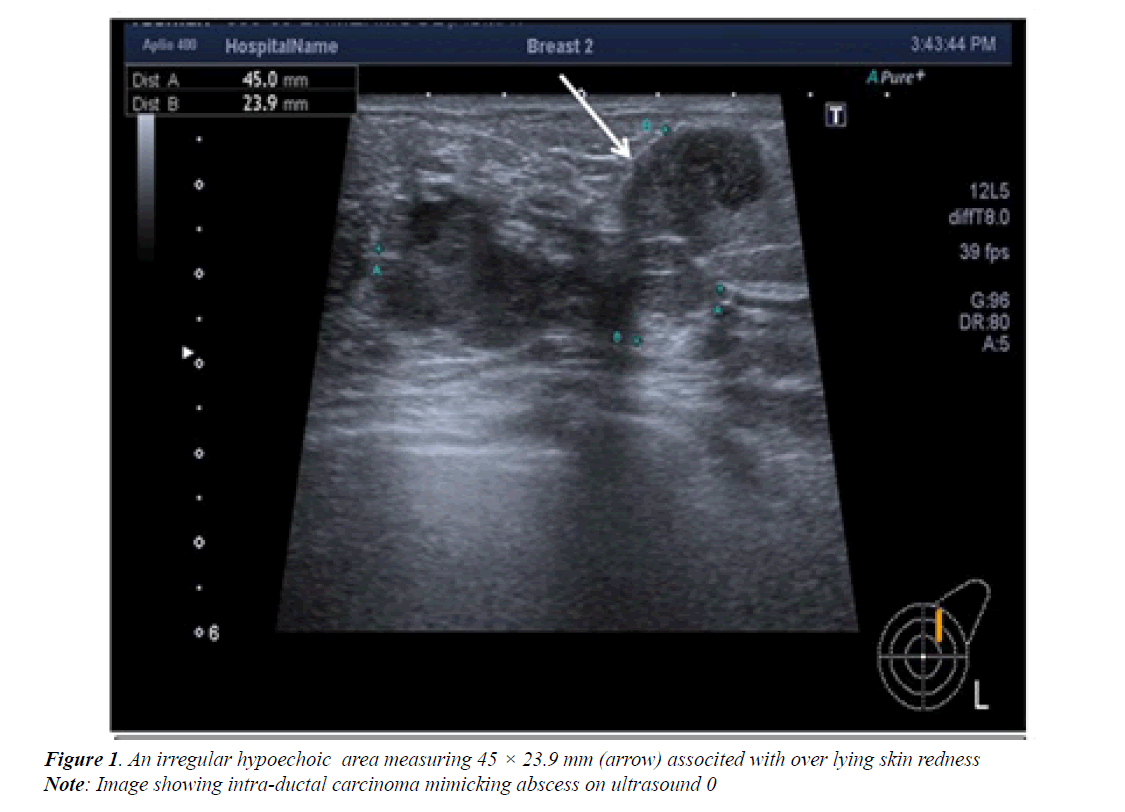
The last follow up at 18 month showed the lesion to be unchanged and was part of scar tissue. The patients reported as discordant malignant, one of them had an irregular hypoechoic area measuring 45 × 23 mm in left breast at 1’o clock position (Figure 1), the overlying skin was warm and red. On ultrasound it was reported as an abscess and follow up was advised after a course of antibiotics, repeat ultrasound showed persistence of the area so an aspiration was done using ultrasound guidance.
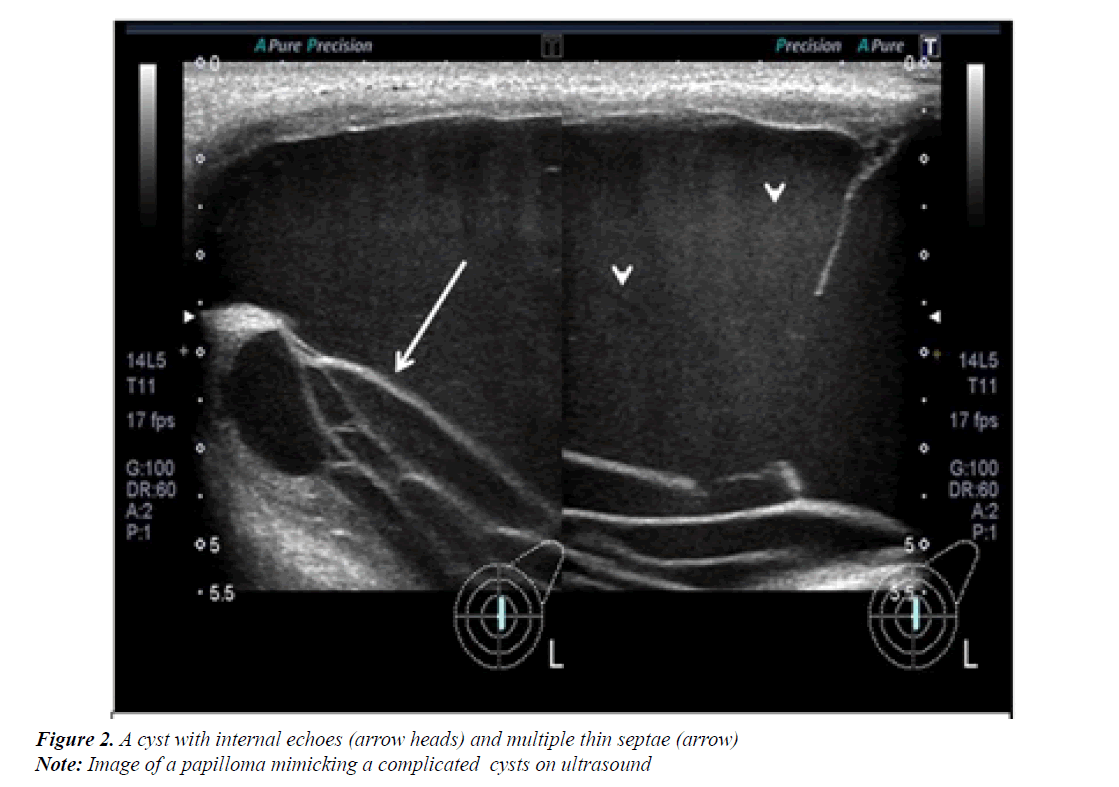
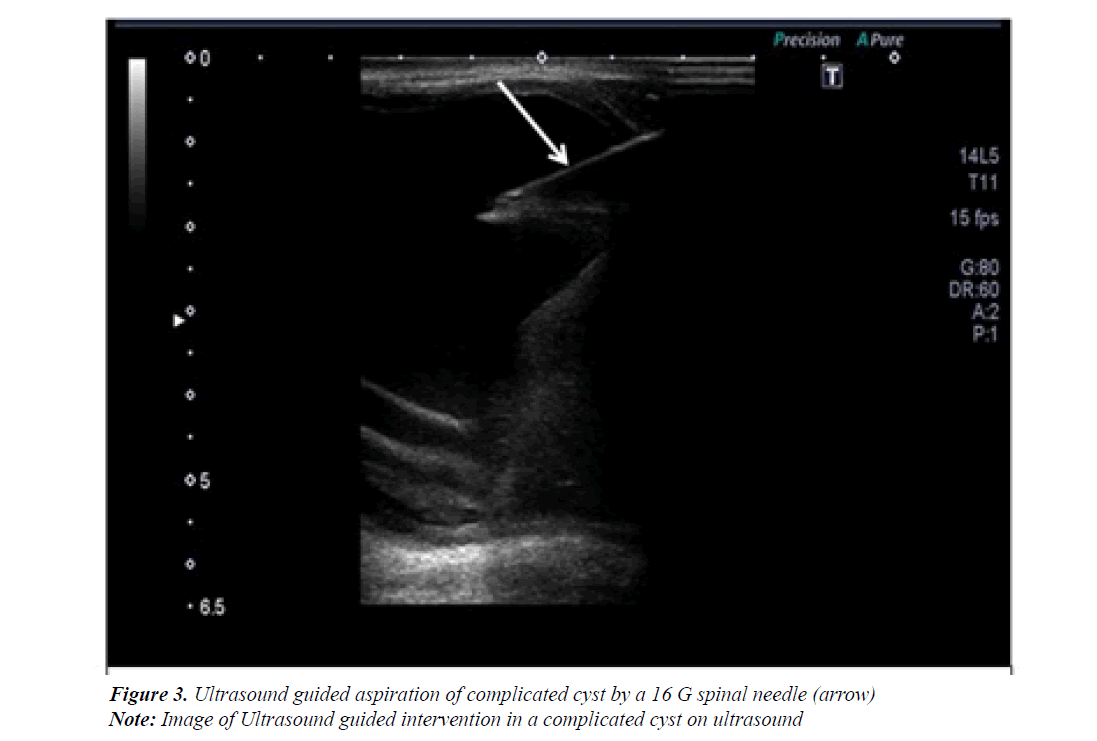
As aspiration was attempted no pus could be aspirated so a core biopsy was done. This was reported on histopathology as intraductal carcinoma. Patient underwent appropriate management. The second patient was reported as having a cystic lesion measuring 4 × 5 cm in left breast (Figure 2) because of its size aspiration was done (Figure 2) followed by biopsy of its wall. Both turn out to be benign however the cyst reformed a respiration was done and the fluid at histology was again negative. The cyst reformed third time and a surgical excision was done, the histopathology showed papilloma (Figure 3).
Discussion
The success of a core breast biopsy program depends upon good communication between radiologist, pathologist and breast surgeon. All core biopsy results should be reviewed by radiologist and a note added regarding concordant/ discordant results, recommendation for follow up/rebiopsy should also be included in the note. The radiologist making recommendations in the report should be the one who has done the biopsy and can also see that the proper lesion was targeted and can also have direct assessment of technical adequacy of biopsy.
Since its introduction in 2003 for ultrasound BI-RADS, has been reported to have a good performance for reporting malignant features and likelihood of malignancy in evaluation of sonographically detected breast masses [13-15]. Based on BI-RADS categorization the indication for doing a biopsy of a lesion can be justified. A category 3 lesion has a 2% probability of being malignant. Biopsy is justified if this is patient or physician preference, as was the case in our study.
A few of our cases were categorized as BI-RADS category 2 still biopsy was done due to patient preference, as our hospital is a tertiary care private hospital and so the cost is born by the patients. In cases of BI-RADS category 3 lesions biopsy was done on patient request or the clinician thought patient was high risk on clinical grounds for risk of breast cancer; this practice is followed in routine all over the world [16].
A recommendation in the fourth addition of BI-RADS is for category 4 to be subdivided internally into three subgroups (4a, 4b and 4c) on the basis of the probability of malignancy; this is regarded as optional [17]. The BI-RADS did not set out specific guidelines with respect to what was the risk of malignancy for each of subcategories. The guidance range recommended [18] for likelihood of malignancy should be 2-10% for category 4a,11-50% for category 4b, and 51-95% for category 4c.The fact that use of subcategories is optional and the clinical data is limited, management is not standardized.
Based on BI-RADS [17], the benign core biopsy results can be regarded as concordant benign and malignant core biopsy results as discordant malignant for category 4a lesions. This is true for our study as 52 lesions were reported as 4a, their histopathology turned out to be benign fibrocystic changes, benign epithelial changes etc. All patients were followed up for 18 month with ultrasound and were put in Category 2. One case of discordant malignant was also put on follow up and the lesion disappeared after one year on follow up ultrasound. The two cases of discordant malignant both underwent proper management according to stage of disease. Careful imaging–pathology co relation allowed detection of false negative results immediately after core biopsy results are received by pointing out discordant lesions prospectively, thereby avoiding delays in diagnosis of carcinoma.
The communication between radiologist and pathologist is backbone of imaging-pathology correlation but is subject to radiologist experience in establishing concordance. The decision to recommend further biopsy or short term follow up depends on radiology histology concordance, a decision which is part of radiologist responsibility if she or he performs breast biopsy [18]. Therefore the radiologist performing the biopsy must be familiar with the imaging features of a vast majority of pathologic breast lesions and must be able to correlate with each other.
There are a few limitation of our study as this is a new practice; lot of literature is not available to compare our results with previously done studies. The number of discordant benign and discordant malignant cases is less so the results cannot be applied to larger population group.
The latest literature is reporting that short-term imaging follow-up in Women with histologically proven concordant benign breast disease followed up closely after biopsy does not contribute to improved breast cancer detection, as all subsequent cancers were detected on annual mammography [19]. But as our study was done in 2013 there we followed the previous protocol of following concordant results on biopsy for 18 months to 2 years. In a recent study conducted by Johnson et al. [20] no significant difference was found between stage, tumor size or nodal status after benign stereotactic or ultrasonography guided core breast biopsy in between patients with short term follow up and those who return to annual follow up.
Conclusion
Cautious Radiology-Pathology co relation is indispensable in addition to appropriate post biopsy management for managing a successful core breast biopsy program. This practice identifies a substantial number of false negative results of core biopsy by identifying discordant results avoiding delays in diagnosis of breast cancer.
Conflict of Interest
None
Funding Source
None
References
- Dennison G, Anand R, Marker SH, et al. A prospective study of the use of fine needle aspiration cytology and core biopsy for breast cancer. Breast J 2003; 9: 491-493.
- Osanai T, Gomi N, Wakita T. Ultrasound guided core needle biopsy for breast cancer: Preliminary report.Jpn J ClinOncol 2000; 30: 56-57.
- Fishman JE, Milikowski C, Ramsinghani R, et al. US-guided core- needle biopsy of breast: How many specimens are necessary? Radiology 2003;226:779-782.
- Wiratkapun C, Wibulpholprasert B, WongwaisayawanS, et al. Non-diagnostic core needle biopsy of the breast under imaging guidance: Results of re biopsy. J Med Assoc Thai 2005;88:350-357.
- Burkhardt JH, Sunshine JH. Core needle and surgical breast biopsy: Comparison of three methods of assessing cost. Radiology 1999;212:181-188.
- Lee CH, Egglin TE, Philpotts L. Cost effectiveness of stereotactic core needle biopsy: Analysis by way of mammographic findings. Radiology 1997; 202: 849-854.
- Liberman L, Feng TL, Dershaw DD. US guided core biopsy use and cost effectiveness. Radiology 1998; 208:717-723.
- Hrung JM, Langlotz CP, Orel SG, et al. Cost effectiveness of MR imaging and core?needle biopsy in the preoperative work up of suspicious breast lesions. Radiology 1999; 213:39-49.
- Parker SH, BurbankF, Jackman RJ. Percutaneous large core breast biopsy: A multi-institutional study. Radiology 1994; 193: 359-64.
- Andersson I, Janzon L. Reduced breast cancer mortality in women under age 50: Updated results from the Malmo Mammographic screening program. J Natl Cancer InstMonogr 1997;22:63-67.
- Tabar L, Vitak B, Hsiu-His TC, et al. Beyond randomized control trials: Organized mammographic screening substantially reduces breast carcinoma mortality. Cancer 2001;91:1724-1731.
- Parikh J, TickmanR. Image guided tissue sampling: where Radiology meets pathology. Breast J 2005;11:403-409.
- Kim EK, Ko KH, Oh KK, et al. Clinical application of the BI-RADS final assessment to breast sonography in conjunction with mammography. AJR Am J Roentgenol. 2008;190: 1209-1215.
- Lazarus E, Mainiero MB, Schepps B, et al.BI-RADS lexicon for US and mammography: Inter-observer variability and positive predictive value.Radiology. 2006;239: 385-391.
- Raza S, Chikarmane SA, Neilsen SS. BI-RADS 3, 4 and 5 lesions: Value of US in management ?follow-up and outcome. Radiology. 2008;248:773-781.
- Lee HJ, Kim EK, Kim MJ, et al. Observer variability of breast imaging reporting and data system (BI-RADS) for breast ultrasound. Eur J Radiol 2008;65:293-298.
- American College of Radiology. Breast imaging reporting and data system-mammography. In: American College of Radiology, ed. Breast imaging reporting and data system,4th ed. Reston, VA: American College of Radiology. 2003.
- Christopher PH, Jennifer EG, Kristen AA, et al. Interactive case review of radiologic and pathologic findings from breast biopsy: Are they concordant? How do I manage results? Radiographics 2013; 33: E149-E152.
- Adams MC, Falcon S, Mooney BP, et al. Short-term imaging follow-up of patients with concordant benign breast core needle biopsies: Is it really worth it? DiagnIntervRadiol 2014; 20:464-469.
- Johnson JM, Johnson AK, O?Meara ES. Breast cancer detection with short-interval follow-up with return to annual screening in patients with benign stereotactic or US-guided breast biopsy results. Radiology 2015; 27:54-60.