Research Article - Biomedical Research (2017) Volume 28, Issue 12
Comparison of dual-source computed tomography (CT) dual-energy angiography with conventional 3D imaging towards caudomedial vessels
Daowei Li, Na Liu, Qiang Ma and Dan He*
Department of Radiology, the People's Hospital of China Medical University and the People's Hospital of Liaoning Province, Shenyang, PR China
- *Corresponding Author:
- Dan He
Department of Radiology
People's Hospital of China Medical University and The People's Hospital of Liaoning Province, PR China
Accepted date: April 28, 2017
Abstract
We aim to analyse the time consumption, image quality and efficacies of dual-source Computed Tomography (CT) Dual-Energy Angiography (DE-CTA) in diagnosing vascular stenosis. The medical records of 35 patients with clinically suspected caudomedial vascular diseases were performed DE-CTA. The residual bone images obtained in DE-CTA and conventional 3D software were compared, as well as the sensitivity and specificity of these two imaging methods in diagnosing the segment with vascular stenosis ≥ 50%. The results showed that the overall effects of Automatic Bone Remove (ABR) were better than Automatic Bone Subtraction (ABS) (P<0.05); the post-processing time consumption of ABS and plaque subtracted after Additional Manual Bone Remove (ABPS) (7.62 ± 2.13 min) was less than that in automatic bone remove after Additional Manual Bone Remove (ABR-M) (11.4 ± 2.5 min), and the difference was statistically significant (P<0.05). The sensitivity and specificity in ABPS and ABR-B towards the segment with stenosis ≥ 50% were: 95.67%, 96.26% and 93.78%, 98.23%, respectively. In conclusion, DE-CTA had better image quality after bone subtraction, could much more accurately diagnose the vascular stenosis, the post-processing time consumption was less than the conventional 3D method, and not affected by human factors.
Keywords
Dual source CT, Energy subtraction, Caudomedial vessel
Introduction
In recent years, with the rapid development of Multi-Slice Spiral Computed Tomography (MSCT) technology, the noninvasive vascular imaging technology had been accelerated and improved, and showed great advantages in practical clinical work [1-3]. But the clinical application towards caudomedial CT Angiography (CTA) was not wide enough, which was mainly because the traditional postprocessing technology showed not ideal results in removing the plaques in pelvis, spine and vascular walls, the time consumption was long, and the effects would be easily affected by operator’s proficiency, so the diagnostic accuracy towards vascular stenosis would be affected to a certain extent [3,4]. The successful development of Dual-Source CT (DSCT) added new technology towards angiography, which could achieve subtracted images among different energy data by its dual-energy mode, thus effectively removed the iodine and calcium-containing materials [5-7]. This information can be used to identify bone and plaque and pull them from the improved dataset, making it possible to display a real luminogram. It was reported that the dual energy subtraction imaging showed no significant difference in image quality than conventional 64 slice CT when applied towards caudomedial vessels, and the radiation dose was not increased, but it was rarely reported about the image qualities of residual bone and plaque [8,9]. This study analysed the image quality, postprocessing time and exhibiting capability towards vascular stenosis, aiming to explore the clinical application value of DSCT energy subtraction imaging.
Materials and Methods
General information
35 patients with suspected caudomedial vascular disease were selected in our hospital from November 2014 to January 2016 for the DE-CTA examination, including 21 males and 14 females, aged 32 to 65 years, with the mean age as (48.32 ± 1.14 y). Exclusion criteria: with poor kidney functions, with adverse reactions or allergic to the contrast agent, BMI>30 kg/m2, with abdominal diameter>35 cm [8]. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of the People's Hospital of Liaoning Province. Written informed consent was obtained from all participants.
DSCT scanning
CTA was performed using a dual-source CT system (Somatom Definition Flash, Siemens, Munich, Germany). The peak voltages of dual-tube balls were 140 kV and 80 kV, respectively, the corresponding peak tube currents were 75 As and 300 As, respectively; pitch 0.5, bed-speed 37 mm/cycle, tube rotation speed 0.33 s/cycle, collimator 2 × 32 × 0.6 mm, CTDIVol 4.1 mGy (3.8~5.6 mGy), thickness of reconstructed layer 1.0 mm. Before scanning, the patient was fasted and restricted water for 6 h, then indwelled one trocar into the median cubital vein; the caudomedial dynamic enhanced scanning was then performed in the supine position, from head to toe, and with the dual-energy mode, the scanning range was from the diaphragmatic dome to the level of inguinal ligament. The non-ionic contrast agent (Ultravist, 300 mg/ml) was injected through cubital vein, with the dosage as 1.5 ml/kg, and the injection rate was 3.5 ml/s, followed by 20 ml of saline injected at the same speed. The bolus tracking intelligent trigger mode was used, and the Region of Interest (ROI) was set in the abdominal aorta, with the threshold value as 100 HU to trigger the scanning. The caudomedial DE-CTA scanning sequence (DE BodyAngioBone Remove) was selected to obtain three mutually matched cross-sectional images, i.e. the images of 140 kV, 80 kV and 140-80-merged (DE Composition 0.3), respectively.
Image processing
All collected data were input into the Siemens workstation (Siemens multi-modality workplace, MMWP), the data obtained at different energies (140 kV, 80 kV) were performed the Automatic Bone Subtraction (ABS) and ABS and plaque subtracted after Additional Manual Bone Remove (ABPS) by the software; the merged data were performed the Automatic Bone Remove (ABR) and automatic bone remove after Additional Manual Bone Remove (ABR-M) [10] in the conventional 3D software (SOMAT OMCA RDIAC). The Maximum Intensity Projection (MIP) and Multiplanar Reformation (MPR) reconstruction were then performed to show the whole vascular image, the adjustments of reconstruction parameters included window width, window position and transparency, and the time consumed in ABPS and ABR-M was also recorded.
Image quality assessment
The images were double-blind evaluated by two physicians in the department of imaging with random sequence, during the diagnostic process, the original images were combined for a comprehensive analysis, and the disagreement was discussed to reach a consensus. The abdominal artery system was divided into 16 segments [11]: superior and inferior abdominal aorta (with the level of renal artery as the border), renal artery (divided into proximal, middle and distal segment), common iliac artery, internal and external iliac arteries (divided into proximal and distal segment), when the accessory renal artery and other variant blood vessels appeared, the division was performed in the corresponding positions.
Evaluation indicators
1. Residual bone scoring [10]: 1 point: with more than 50% residual bone; 2 points: with 25% to 49% residual bone; 3 points: with 10% to 25% residual bone; 4 points: with less than 5% residual bone. 2. Arterial visibility scoring [11]: 0 point: poor or non-visibility, could not perform the clinical diagnosis; 1 point: acceptable visibility for the main vessel, while nonvisibility for partial peripheral and collateral vascular structures or exhibited significant deformation, pseudo movies, and the clinical diagnosis could be acceptable; 2 points: clear visibility to blood vessels, with mild deformation or artifacts, could meet the clinical diagnosis; 3 points: very clear visibility to vascular structures, could fully meet the clinical diagnosis. 3. As for the vascular segment with arterial visibility score ≥ 1, it was divided into four grades depending on the degrees of vascular stenosis [11]: grade 0: without stenosis or stenosis<10%; grade 1: stenosis within 10% to 49%; grade 2: stenosis within 50% to 99%; grade 3: vessel was completely occluded. When more than one stenotic luminal change was detected in the same vessel segment, the most severe stenosis was used for grading and analysis.
Statistical analysis
The results are expressed as means ± SD. For all statistical determinations a value of p ≤ 0.05 (two-sided) was considered significant. All statistical analyses were performed using SPSS 13.0 software.
The paired t-test was performed to compare the residual bone situations in ABR and ABS, average postprocessing time and arterial visibility score in ABPS and ABR-M. The comprehensive diagnostic results of MPR and the original images were used as the standard, and the fourfold table was used to calculate the specificity and sensitivity of ABPS and ABR-B in diagnosing the segment with vascular stenosis ≥ 50%; with P<0.05 considered as the statistical significance.
Results
The examination processes of the 35 patients went smoothly, a total of 560 vascular segments were examined, among which 57 segments exhibited the arterial visibility score as 0, and 3 patients were found 5 accessory renal arteries.
Conditions of residual bones
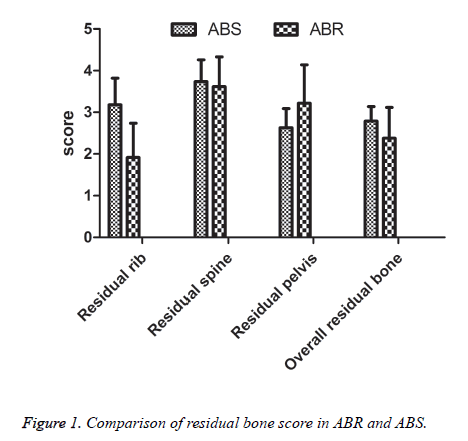
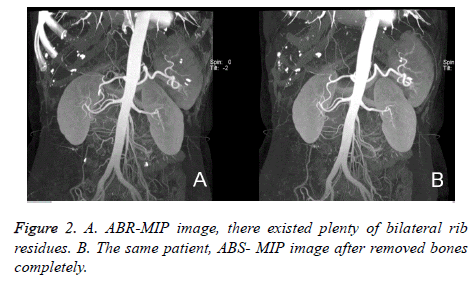
Effect comparison of two different automatic bone removal methods: the overall residual bone in MIP of ABR was less than ABS (Figures 1 and 2), while the residual bone in pelvis was slightly more than ABS (Figure 1), there existed no significant difference in the effects of removing spinal bone (P>0.05).
Conditions of postoperative time-consumption
Comparison of average postprocessing time between the 2 methods: the average postprocessing time of ABPS (7.62 min ± 2.13 min) was less than ABR-M (9.64 min ± 1.32 min), and the difference was statistically significant (P<0.05, Table 1).
| Parameter | MPR | ABPS | ABR-M |
|---|---|---|---|
| Postprocessing time (min) | - | 7.62 ± 2.13 | 11.4 ± 2.5 |
| Arterial visibility score | - | 3.63 ± 0.54 | 3.61 ± 0.72 |
| Grading of luminal arrowing | |||
| Total number of vascular segments | 508 | 508 | 508 |
| Grade 0: 0%-10% stenosis | 288 | 286 | 272 |
| Grade 1: 10%-49% stenosis | 95 | 108 | 109 |
| Grade 2: 50%-99% stenosis | 66 | 65 | 67 |
| Grade 3: occlusion | 59 | 49 | 60 |
| Sensitivity of stenosis ≥ 50% (%) | - | 95.67 | 93.78 |
| Specificity of stenosis ≥ 50% (%) | - | 96.26 | 98.23 |
Table 1. Comparison of postprocessing time, arterial visibility and stenotic segment evaluation between ABPS and ABR-M.
Conditions of arterial displaying
Comparison of diagnostic accuracy towards vascular stenosis between the two methods: The difference in arterial visibility scores between ABPS and ABR-M showed no statistical significance (P>0.05, Table 1), 508 segments were actually used to evaluate the stenotic degrees of main-iliac artery and renal artery; The sensitivity and specificity of ABPS and ABRB towards the segment with stenosis ≥ 50% were 95.74%, 96.19% and 92.93%, 97.87%, respectively (Table 1).
Discussion
Presently, the common imaging methods used for the caudomedial vascular examination were MRA, color Doppler ultrasound, routine CTA and DSA, among which MRA had no ionizing radiation, and needed no injection of contrast agent [1,3], but it was difficult for the MRA images to accurately display the situations of peripheral vascular diseases, and it was not sensitive to the calcification, meanwhile, the examination time was too long [2,4]. Color Doppler ultrasound was simple, non-invasive, with relatively low cost, while it could be easily interfered by the breathing exercises and abdominal intestinal gas, and the effects towards the wide range of vessel wall calcification were poor, furthermore, the results were also largely affected by operator’s proficiency [11,12]. Conventional CTA was more general, but it’s still shows a lower sensitivity for quantifying stenosis in the presence of dense calcification or indwelling stents since these may obscure contrast material in the lumen [10]. Drawbacks of CTA are the exposure to radiation and iodinated contrast agents, as well as the need for postprocessing methods. It would be difficult to accurately assess the stenotic situations, the time consumption of manual deboning was long and would be easily affected by operator’s proficiency [3-5]. The DSA examination had been considered as the gold standard towards the diagnosis of vascular diseases [11,13], but it was an invasive examination, with the risks of focal hematoma and distal embolization occurred at the puncture sites, and the operator and patient would be largely affected by the radiation dose.
DSCT dual energy subtraction imaging was a new technology, one scanning could gather the data of two different energies, and the flying focal spots between two points of Z-axis [2,5-7] made it possible to obtain the reconstructed images with excellent isotropism and all-phase homogeneity; its subtraction used the difference of X-ray, with different energies, towards the decay rates of serum iodine ingredients and calcified or bony components, thus the blood vessels with complex structures could be directly separated, as well as removed the bony structures and hard plaques on vascular walls [2,10].
Advantages of DE-CAT are the shorter acquisition time, has the potential to distinguish iodine from bone or calcifications using the attenuation difference between the two energies, and the lower cost. The results of this study showed that the overall residual bone in DE-CAT was significantly less than the conventional 3D angiography (P<0.05), consistent with Meyer et al. [14]. Because DSCT distinguished the tissue components according to their differences in X-ray attenuation, the distinction towards bone and blood vessels was more complete and accurate than the conventional angiography 3D software, which used the density difference to remove bones [6,15]. The ABS operation could be realized through simply pressing one key, meanwhile the plaques could also be removed, which greatly reduced the data processing time and physician’s workload, and would not be affected by operator’s proficiency. The results of this study still remained a small amount of residual bone, which needed to be further removed manually (Figure 1), especially the ABS effects towards pelvis were slightly less (Figure 1), therefore, the software still needed further perfection [9,16]. It was reported [2,5,6] that when scanning the body parts with more bones, such as skull and thoracoabdomen, because the dual energy scanning had large data, the postprocessing might be prolonged. However, in this study, the postprocessing time towards the caudomedial vessels was (7.62 ± 2.13 min), shorter than the traditional 3D vascular imaging method (P<0.05).
Willmann et al. [16] reported that the diagnostic sensitivity and specificity of traditional 64 slice CT towards the stenosis of aortic-iliac artery and renal artery were 92.0% and 99.0%, and the results of this study (ABR-M) were 93.78% and 98.23%, close to the above results; because DSCT dual energy workstation could better define the relationships between the iodine- and calcium-containing materials, it could effectively remove the perivascular bones and the calcified plaques on vascular walls, thus avoiding the impacts of calcified plaques and bones on the vessels [5,17], and much more clearly exhibiting the vascular structures, so the image qualities were satisfactory, with the sensitivity and specificity as 95.67% and 96.26%, respectively, the sensitivity was better than the traditional 3D CTA. Our study showed that calcified plaques were almost completely removed from the carotids after applying DE bone removal and hard plaque removal postprocessing to DE-CAT images. Compared with MPR and the original images, ABPS had 11 segments overvalued, while 9 segments undervalued, the possible reasons were: when the local vessels were seriously eroded by the lesions or the vascular distortion was larger, the opening of collateral circulation might develop the occluded distal vessels, which might easily be misunderstood as that the vessels were not occluded; as for the blood vessels adjacent to bones, they might be excessively separated during the ABS process, especially when the wall had hard plaques, due to the partial volume effects, they might be easily excessively separated, so the original images needed to be combined for the analysis to improve the diagnostic accuracy [17,18].
Limitations of this study: the number of patients included was small, thus needed to be further enlarged in future researches; due to the restrictions of small bulb FOV (26 cm), tall or more obese patients could not be included; because the manual removal of residual bone was performed, the diagnostic accuracies towards stenosis of these two method might be overestimated; and the results were not compared with the gold standards of vascular examination (DSA) [11-16].
This study preliminarily considered: DSCT automatic bone subtraction could effectively separate vessels and bony structures, and could better remove the vascular calcification, thus better exhibiting the situations of inner vascular walls, while saving more time and much more feasible than the conventional 3D CTA [13,19].
Conclusions
The energy subtraction had high accuracy in diagnosing and evaluating the caudomedial stenotic blood vessels, while would not be affected by the calcified plaques to some extent, the sensitivity could then be increased, so it could become the main method for the preoperative evaluation and screening of caudomedial arterial diseases, and worthy of clinical applications.
Acknowledgements
All data and experiments were done by my team. Here we thank professor He Dan for energetic support and help in the process of experience. I really very much appreciate your months of guidance and help.
Conflicts of Interest
All of the authors declare that they have no conflicts of interest regarding this paper.
References
- Lell MM, Anders K, Uder M, Klotz E, Ditt H. New techniques in CT angiography. Radiographics 2006; 26: 45-62.
- Delesalle MA, Pontana F, Duhamel A, Faivre JB, Flohr T. Spectral optimization of chest CT angiography with reduced iodine load: experience in 80 patients evaluated with dual-source, dual-energy CT. Radiology 2013; 267: 256-266.
- Gnannt R, Fischer M, Goetti R, Karlo C, Leschka S. Dual-energy CT for characterization of the incidental adrenal mass: preliminary observations. AJR Am J Roentgenol 2012; 198: 138-144.
- Qu M, Jaramillo-Alvarez G, Ramirez-Giraldo JC. Urinary stone differentiation in patients with large body size using dual-energy dual-source computed tomography. Eur Radiol 2013; 23: 1408-1414.
- Johnson TR, Krauss B, Sedlmair M, Grasruck M, Bruder H. Material differentiation by dual energy CT: initial experience. Eur Radiol 2007; 17: 1510-1517.
- Schulz B, Kuehling K, Kromen W. Automatic bone removal technique in whole-body dual-energy CT angiography: performance and image quality. AJR Am J Roentgenol 2012; 199: 646-650.
- Kaluri R, Pratap CH. Sign gesture recognition using modified region growing algorithm and adaptive genetic fuzzy classifier. Int J Intel Eng Sys 2016; 9: 225-234.
- Breeze J, West A, Clasper J. Anthropometric assessment of cervical neurovascular structures using CTA to determine zone-specific vulnerability to penetrating fragmentation injuries. Clin Radiol 2013; 68: 34-38.
- Graser A, Johnson TR, Chandarana H, Macari M. Dual energy CT: preliminary observations and potential clinical applications in the abdomen. Eur Radiol 2009; 19: 13-23.
- Meyer BC, Werncke T, Hopfenmüller W, Raatschen HJ, Wolf KJ. Dual energy CT of peripheral arteries: effect of automatic bone and plaque removal on image quality and grading of stenoses. Eur J Radiol 2008; 68: 414-422.
- Schertler T, Wildermuth S, Alkadhi H. Sixteen-detector row CT angiography for lower-leg arterial occlusive disease: analysis of section width. Radiology 2005; 237: 649-656.
- Rajesh K, Pradeep CH. An enhanced framework for sign gesture recognition using hidden markov model and adaptive histogram technique. Int J Intel Eng Sys 2017; 10: 11-19.
- Waugh JR, Sacharias N. Arteriographic complications in the DSA era. Radiology 1992; 182: 243-246.
- Meyer BC, Werncke T, Hopfenmüller W, Raatschen HJ, Wolf KJ. Dual energy CT of peripheral arteries: effect of automatic bone and plaque removal on image quality and grading of stenoses. Eur J Radiol 2008; 68: 414-422.
- Mongan J, Rathnayake S, Fu Y. Extravasated contrast material in penetrating abdominopelvic trauma: dual-contrast dual-energy CT for improved diagnosis-preliminary results in an animal model. Radiology 2013; 268: 738-742.
- Winklehner A, Gordic S, Lauk E. Automated attenuation-based tube voltage selection for body CTA: Performance evaluation of 192-slice dual-source CT. Eur Radiol 2015; 25: 2346-2353.
- Ramon F, Diego S, Ivonne G. Asymptomatic bilateral calcified stylohyoid ligaments detection by panoramic radiography and cone beam computerized tomography. Biomed Res 2016; 27: 1413-1415.
- Rajesh K, Pradeep CH. A comparative study on image segmentation techniques. Int J Pharm Technol 2016; 8: 12712-12717.
- Willmann JK, Wildermuth S, Pfammatter T. Aortoiliac and renal arteries: prospective intraindividual comparison of contrast-enhanced three-dimensional MR angiography and multi-detector row CT angiography. Radiology 2003; 226: 798-811.