- Biomedical Research (2014) Volume 25, Issue 3
Comparison of adhesion-preventing meshes in a rat model of incisional hernia in terms of intra-abdominal adhesions and other complications
Leblebici IM1*, Bozkurt S2 and Sever B31General Surgery Department of Sivas Susehri State Hospital, Sivas, Turkey
2General Surgery Department of Medicine Faculty, Bezmialem Vakıf University of Istanbul, Istanbul, Turkey
3Gynecology and Obstetrics Department of Sivas Susehri State Hospital, Sivas, Turkey
- *Corresponding Author:
- Leblebici, Ihsan Metin. M.D.
General Surgery Department of Sivas Susehri State
Hospital, Sivas, Turkey.
Address: Sivas Susehri State Hospital
Susehri, 58600, Sivas, Turkey
Accepted date: April 07 2014
Abstract
The aim of the present study is to evaluate the severity of adhesions occurring after the use of different meshes for incisional hernia repair in rats. We assigned 37 female Wistar– Albino rats to four groups. A 2 × 2 cm abdominal wall defect was created in all rats. In Group 1 (Control), the peritoneum was closed with 4/0 polypropylene sutures. The abdominal wall defect was repaired with a condensed polytetrafluoroethylene mesh in Group 2, a polypropylene mesh coated with absorbable polydioxanone on the parietal side and oxidized regenerated cellulose on the visceral side in Group 3 and a PP mesh coated with carboxymethylcellulose and sodium hyaluronate on one side in Group 4. The abdominal wall with the adherent tissue was resected en bloc for macroscopic, histological and biochemical examinations. Fibrosis was significantly less severe in the control group than in the mesh groups, but did not significantly differ between the mesh groups. The average pressure required to break the resected mesh specimen was significantly lower in the control group than in the mesh groups, but did not significantly differ between the mesh groups. The mean hydroxyproline level was significantly lower in of Group 1 (Control) than in Groups 3 and 4 and in Group 2 than in Group 3. None of the meshes tested in this study was superior to the others in terms of severity of adhesions and incidence of complications. All three meshes, when placed in the peritoneum, resulted in more fibrosis than that in the control group.
Keywords
adhesion, hernia, incisional hernia, mesh
Introduction
In 1900, Witzel and Goepel first repaired hernias using a material. In 1958, Usher used a polyamide mesh for hernia repair, bringing in a new era in hernia surgery [1]. In recent years, the incidence of incisional hernia has increased with abdominal surgical interventions, and is 2–11% after median incisions, 30–50% after primary repair and <15% after repair with prosthetic materials [2]. The meshes are used at the prepearing of the incisional hernias. All meshes have both advantages and disadvantages, and no ideal mesh has yet been found [3-6]. The most important disadvantage of the meshes used in incisional hernia repair is the development of massive adhesions between the mesh and the intraabdominal organs, resulting in intestinal obstruction and enterocutaneous fistula [5-7].
The characteristics of an ideal mesh have been identified through experimental and clinical studies. Permeable prostheses are preferred to non-permeable prostheses, because the former pose no risk of serum or lymphatic collection; moreover, tissue growth into the mesh is easier, and thus, prosthesis fixation is easy and does not require much suturing. Monofilament materials are preferred owing to their low infection risk. Contact of the prosthesis with internal organs must be avoided. The prosthesis must cover the hernia defect in such a way that it can be fixed to intact tissue, so that the advantage of support of the normal abdominal wall can be taken [8].
In 1942, a five-item approach was suggested for the reduction of intra-abdominal adhesions: (i) minimizing peritoneal trauma and preserving the peritoneum, (ii) preventing coagulation of serous exudate, (iii) degrading collected fibrin, (iv) keeping the involved surfaces separate until mesothelial regeneration and (v) preventing inflammatory reaction [9]. Intra-abdominal adhesions can be prevented by interrupting their pathogenesis via surgical techniques, pharmacological agents and physical barriers.
Various meshes have been developed as physical barriers to prevent adhesions [10]. Polypropylene (PP) meshes are made of non-absorbable, braided monofilaments. PP meshes result in massive adhesions when placed directly over the intra-abdominal organs, and may lead to severe complications such as fistula [11,12]. Polytetrafluoroethylene (PTFE) meshes are made of an expandable, nonbraided, non-absorbable biocompatible material. Compared to PP meshes, PTFE meshes rarely cause intraabdominal adhesions, as their micropores help inhibit tissue inflammatory response [4,5,13-15]. Therefore, these meshes can even be used in the presence of an infection [2]. Composite meshes consisting of a PP mesh with hyaluronic acid–carboxymethylcellulose components on one side of the mesh have been developed to prevent the formation of adhesions. This composite mesh creates a temporary barrier on the internal surface, while retaining the strong penetration ability of PP meshes. Moreover, this mesh is hydrophilic and soluble, and is resorbed within a week [14,15]. A double-layer mesh consisting of a PP mesh covered with absorbable polydioxanone (PDS) on the parietal side and oxidized regenerated cellulose (ORC) on the visceral side has also been developed [14].
Pharmacological agents that are used to prevent intraabdominal adhesions either interfere in the steps of wound healing, or prevent or treat the causes of adhesions such as infection and exudate. Although these agents prevent adhesion development to varying extents, the success rate of all these approaches is limited [16,17].
In the current study, we study our purposes in a rat model because of the similarty of rat's and human's anatomy. And also, it is easier to grow and feed the rats than the other animals for using in the experiments.
In the present study, intra-abdominal adhesions formed after the use of different prosthetic materials for hernia repair were investigated in a rat model of incisional hernia. The severity of intra-abdominal adhesions and the incidence of other complications were compared among the different prosthetic materials via macroscopic, histopathological and biochemical examinations.
Materials and Methods
This experimental study was conducted in 2009; the study was approved by the ethics committee of our laboratory and was in accordance with the standards of the European Convention for the Protection of Vertebrate Animals used for Experimental and Other Scientific Purposes (ETS 123).
Thirty-seven female Wistar–Albino rats were assigned to four groups: three groups in which three different meshes were used, with each group containing 10 rats, and a control group of seven rats. The rats were subjected to intraperitoneal anesthesia, and under sterile conditions, their abdominal skin was separated from the underlying muscle and fascia through a median incision to create a 2 × 2 cm defect.
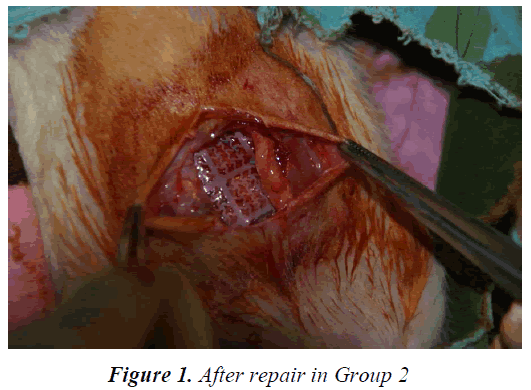
In the control group (Group 1), only an inlay suture was put on the four edges of the peritoneum using 4/0 polypropylene (Prolene®, Ethicon Inc., Somerville, New Jersey). The skin was closed by continuous sutures with 3/0 polypropylene. In the mesh groups, the abdominal wall defects were repaired using 2 × 2 cm, pre-prepared meshes as follows: Group 2, condensed PTFE (MotifMesh™, Proxy, Biomedical Limited, Galway, Ireland; Figure 1); Group 3, double-layer PP mesh covered with absorbable PDS on the parietal side and ORC on the visceral side (Proceed®, Ethicon) and Group 4, PP mesh with hyaluronic acid and carboxymethylcellulose components on one side (Sepramesh ®, Genzyme Surgical Prd., Cambridge, MA). The abdominal skin was closed using continuous sutures with 3/0 polypropylene after the meshes were placed into the peritoneum (inlay) in a primary fashion and fixed with 4/0 polypropylene sutures.
The rats were monitored for 28 days to check for weight loss, decreased food and/or water intake and infection. They were sacrificed on postoperative day 28. The abdominal skin over the fascia was decollated in order to not damage the surgical line. The anterior abdominal wall was opened via a wide, concave, full-thickness incision such that the fascial defect and the mesh could be explored from 2 cm below.
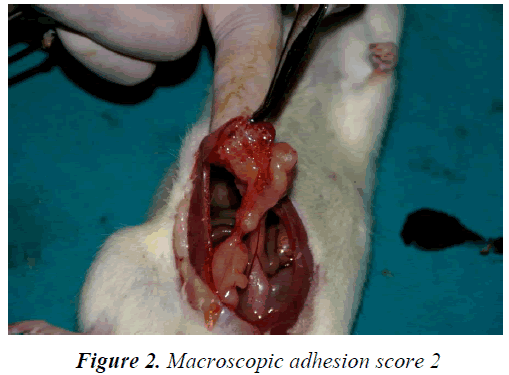
The incision and any adhesions between the mesh and intra-abdominal organs were evaluated using the macroscopic intra-abdominal adhesion scoring system proposed by Mazuji et al. [18]. The macroscopic adhesions were classified with the system identified by Majuzi [18]. Classification system is like that: a) No adhesion; score 0. b) Thin or narrow, easily separable adhesions; score 1. c) Adhesions limited to a small area; score 2. d) Thick adhesions dispersed over a large area; score 3. e) Thick and wide adhesions, adhesions of the organs to the anterior and/or posterior abdominal wall; score 4. Migration of the prosthetic material and presence of enterocutaneous fistula were also evaluated.
Histopathological examination was performed to assess the fibroblast density (0: no fibrosis, 1: minimal, loose fibrosis, 2: moderate fibrosis, 3: florid, massive fibrosis) and inflammation score (0: no inflammation, 1: large cells, rare, dispersed lymphocytes and plasma cells, 2: large cells together with increased number of lymphocytes, neutrophils, eosinophils and plasma cells, 3: multiple mixed inflammatory cells and presence of micro-abscess) [10].
The remaining 2 × 1 cm of the mesh along with the adherent tissue was harvested, and the pressure required to break the specimen was recorded in kilograms using a tensiometer. Thereafter, the specimens were placed in normal saline and sent to a biochemistry laboratory for hydroxyproline assessment. Tissue hydroxyproline levels in the materials sent were measured using high-performance liquid chromatography in milligrams per liter per gram tissue.
Statistical analyses were performed using the NCSS 2007 package program. Data were evaluated with the Kruskal– Wallis test (KW) for intergroup comparisons and with Dunn’s multiple comparison test for subgroup comparisons. Quantitative data were compared using the chisquare test. Statistical significance was set at p < 0.05.
Results
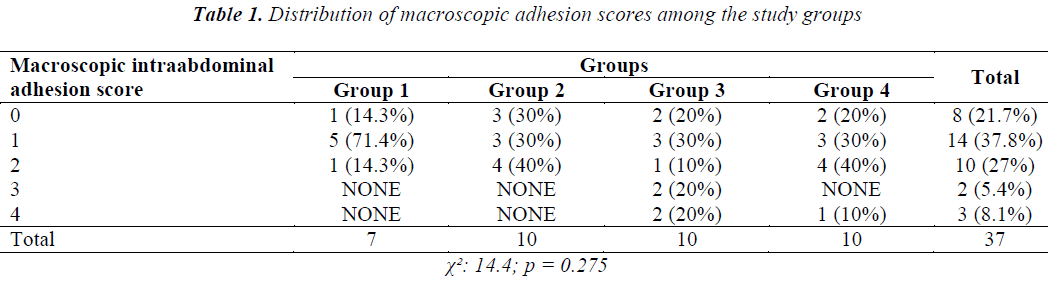
No deaths, surgical wound infections or weight loss occurred in the subjects during the study. The results of macroscopic evaluation of the adhesions are summarized in Table 1 (Figure 2). Statistical comparison of the macroscopic adhesion score among the study groups revealed a χ2; value of 14.4 and a p value of 0.275. No statistical differences were observed between the four groups in terms of distribution of macroscopic intra-abdominal adhesion scores (p = 0.275).
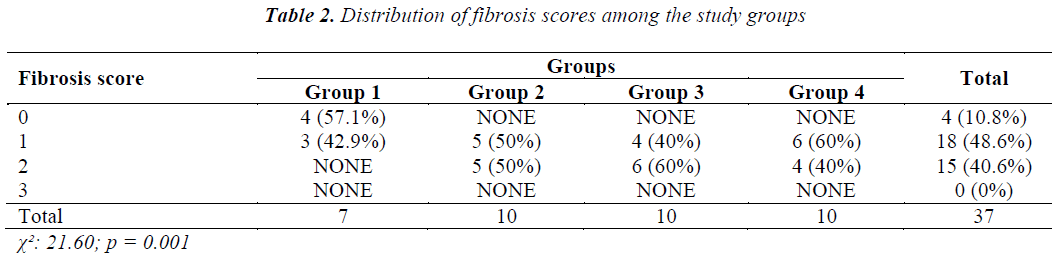
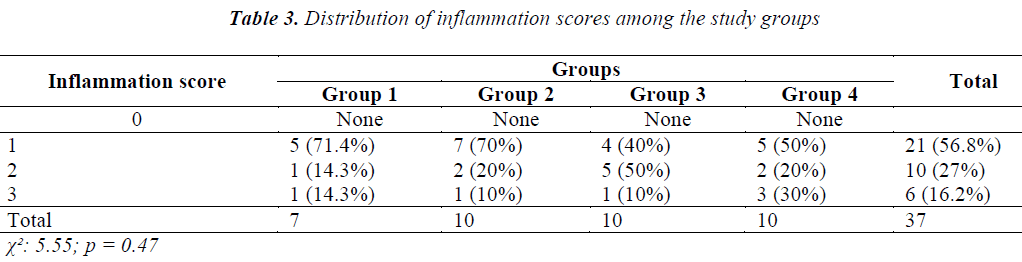
Using light microscopy, we assessed the tissue samples using the fibrosis (Table 2) and inflammation scoring systems (Table 3) used by Hooker et al. [10]. Statistical comparison of the groups and p values in terms of fibroblast density were as follows: Group 1 (Control) vs. Group 2, 0.009; Group 1 (Control) vs. Group 3, 0.007; Group 1 (Control) vs. Group 4, 0.012; Group 2 vs. Group 3, 0.653; Group 2 vs. Group 4, 0.653; and Group 3 vs. Group 4, 0.371. Significant differences were found among the fibrosis scores of Groups 1–4 (p = 0.0001). A score of 0 was significantly more common in Group 1 (Control) than in Groups 2–4 (p = 0.009, p = 0.007 and p = 0.012, respectively). No differences in fibrosis scores were found between the other groups (p > 0.05). Statistical comparison of the inflammation scores in the various study groups revealed a χ2; value of 5.55 and a p value of 0.475. No significant difference was observed in the distribution of inflammation scores among Groups 1–4 (p = 0.275).
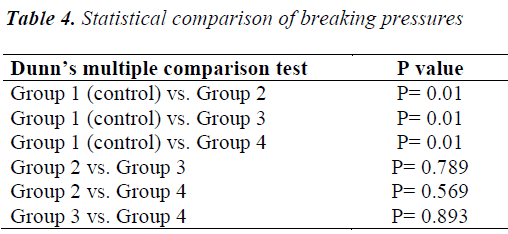
The statistical comparison of the breaking pressures, as assessed using a tensiometer, in the various groups is presented in Table 4. Significant differences in mean breaking pressure were observed among Groups 1–4 (p = 0.007). The mean breaking pressure was significantly lower in Group 1 (Control) than in Groups 2–4 (p = 0.001). No statistical differences in mean breaking pressure were found among the other groups (p > 0.05).
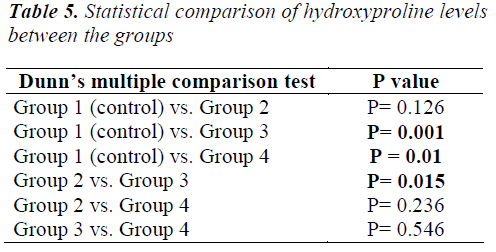
The statistical comparison of hydroxyproline levels among the groups is presented in Table 5. Significant differences in mean hydroxyproline levels were observed among Groups 1–4 (p = 0.0001). The mean hydroxyproline level was significantly lower in Group 1 than in Groups 3 and 4 (p = 0.001 and p = 0.01, respectively) and in Group 2 than in Group 3 (p = 0.015). No other statistical differences were observed among the groups (p > 0.05).
Mesh migration, which was one of the complications assessed macroscopically, was not observed in Groups 1 (Control) and 2, but was present in four subjects in Group 3 and three subjects in Group 4. No significant difference was found between the groups in terms of presence of migration (p = 0.055). Similarly, there were no statistical differences among the four groups in terms of presence of fistula (χ2: 2.77; p = 0.427). Fistula was detected in only a single subject in Group 3.
Discussion
Incisional hernias are encountered as a complication of abdominal surgical interventions and are a type of iatrogenic hernia. Prosthetic materials (meshes) that are used for the repair of incisional hernia frequently lead to intraabdominal adhesions due to the intense inflammatory response that these materials elicit. The resulting adhesions cause intestinal obstruction, chronic abdominal pain and enterocutaneous fistula, as well as difficult resurgeries and infertility in women [19].
Peritoneal trauma such as surgery is the main cause of intra-abdominal adhesion. Ischemia and the presence of a foreign body enhance the development of adhesions [20,21]. Minimally invasive surgical techniques, including laparoscopic techniques, are being developed to reduce the likelihood of intra-abdominal adhesions after incisional hernia repair. In addition, prostheses made of different materials in different designs are also being investigated for use in modern hernia surgery. In order to reduce adhesions via current approaches, peritoneal trauma should be reduced, inflammatory response and coagulation should be inhibited and surfaces that are likely to form adhesions should be cleaned to inhibit fibrosis [9].
Currently, a double-layer PP mesh covered with absorbable PDS on the parietal side and ORC on the visceral side (Proceed®), a PP mesh that includes hyaluronic acid and carboxymethylcellulose components on one side (Sepramesh®) and a condensed PTFE mesh (Motif-Mesh™) are frequently used in incisional hernia repair when primary closure of the peritoneum and fascia is not feasible. The present study macroscopically, histopathologically and biochemically compared these three frequently used meshes in terms of their capacity to elicit intra-abdominal adhesions.
The three mesh groups (Groups 2–4) were compared with a control group and with each other in terms of macroscopic adhesions, and macroscopic intra-abdominal adhesions of varying severity were detected in 79.3% of the cases. However, none of the groups was statistically superior to the others. Voskerician et al. compared condensed PTFE with the double-layer PP mesh used in this study, in terms of adhesions and found the former to be superior [22]. Burger et al. found that a PP mesh with hyaluronic acid and carboxymethylcellulose components on one side was superior to the double-layer PP mesh [23].
In our study, histopathological examination revealed that a fibrosis score of 0 was significantly more common in Group 1 (Control) than in the mesh groups, and that the incidence of this score was similar among the mesh groups, indicating that fibrosis during wound healing was enhanced in the presence of a foreign body in contact with the peritoneum. Inflammation was found in all the study groups, with an inflammation score of 1 in 56.8% of cases. However, none of the groups was found to be superior to the other in terms of inflammation.
In our study, mean hydroxyproline levels significantly differed between the four groups (p = 0.0001). This level was significantly lower in Group 1 (Control) than in Groups 3 and 4 (p = 0.001 and p = 0.01, respectively) and in Group 2 than in Group 3 (p = 0.015). No other significant differences were observed between the groups (p > 0.05).
Mesh migration occurred in Groups 3 and 4, and its incidence in these two groups was statistically similar. Fistula occurred in only a single subject in Group 3, with no significant differences between the groups. Numerous complications have been reported with the use of mesh materials and include infection, chronic sinuses, intraabdominal adhesions, enterocutaneous fistula, intestinal obstruction, malnutrition and hernia recurrence [24].
Conclusion
We compared a double-layer PP mesh covered with absorbable PDS on the parietal side and with ORC on the visceral side (Proceed®), a PP mesh with hyaluronic acid and carboxymethylcellulose components on one side (Sepramesh®) and a condensed PTFE mesh (Motif- Mesh™) in terms of the severity of adhesions and other complications, by using macroscopic, biochemical and histopathological examinations. None of the meshes was superior to the others. On biochemical examination, intraabdominal adhesions were less severe with the condensed PTFE mesh than with the double-layer PP mesh. However, all three meshes, when placed in the peritoneum, resulted in more severe fibrosis than that in the control group. Further clinical and experimental studies are required to develop an ideal mesh that would minimize intra-abdominal adhesions.
Conflict of Interest Statement
There are not any conflicts of interest about our manuscript.
References
- Abrahamson J. Hernias. Zinner MJ, Schwartz SI, Ellis H (eds), Maingot’s Abdominal Operations, 10th edition, Appleton&Lange, Stanford 1997; 479-580.
- Young RM, Gustafson R, Dinsmore RC. Sepramesh vs. Dualmesh for abdominal wall hernia repairs in a rabbit model. Curr Surg. 2004; 61: 77-79.
- Read RC. Development of inguinal herniorraphy. Surg Clin North Am 1984; 64: 185-196.
- Nyhus Lm, Pollak R. Epigastric, Umbilical and Ventral incisional hernias. Cameron JL (Editor), Current Surgical Therapy, 4th edition, BC Decker, St. Louis 1992; 536.
- Dinsmore RC, Calton WC, Harvey SB, Blaney MW. Prevention of Adhesions to Polypropylene Mesh in a Traumatized Bowel Model. J Am Coll Surg 2000; 191: 131-136.
- Oncel M, Remzi FH, Seganore JA, Connor JT, Fazio VW. Application of Adcon-P or Seprafilm in consecutive laparotomies using a murine model. Am Journal Surg 2004; 187: 304-308.
- Johns DA, Ferland R, Dunn R. Initial feasibility study of a sprayable hydrogel adhesion barrier system in patients undergoing laparoscopic ovarian surgery. J Am Assoc Gynecol Laparosc. 2003; 10: 334-338.
- Read RC, Grose WE. Ventral and Incisional Hernias. Nyhus LM. (Editor), Schackelford's Surgery of the Alimentary Tract, 3th edition, WB Saunders Co, Philadelphia 1991; 150-172.
- Boys F. The prophylaxis of peritoneal adhesions. A review of the literature. Surgery. 1942; 11: 118-168.
- Hooker GD, Taylor BM, Driman DK. Prevention of adhesion formation with use of sodium hyaluronate–based bioresorbable membrane in a rat model of ventral hernia repair with polypropylene mesh A randomized, controlled study. Surgery 1999; 125: 211-216.
- Lee J.H, Go A.K, Oh S.H, Lee KE, Yuk SH. Tissue anti-adhesion potential of ibuprofen-loaded PLLA–PEG diblock copolymer films. Biomaterials 2005; 26: 671-678.
- Baptista ML, Bonsack ME, Delaney JP. Seprafilm reduces adhesions to polypropilene mesh. Surgery. 2000; 128: 86-91.
- Matthews BD, Mostafa G, Carbonell AM, Joels CS, Kercher KW,Austin C, et al. Evaluation of adhesion formation and host tissue response to intra abdominalpolytetrafluoroethylene mesh and composite prosthetic mesh. J Surg Res 2005; 123: 227-234.
- Saravelos HG, Li TC. Physical barriers in adhesion prevention. J Reprod Med 1996; 41: 42-51.
- Diamond MP, Linsky CB, Cunningham T, Constantine B, diZerega GS, DeCherney AH. A model for sidewall adhesions in the rabbit: reduction by an absorbable barrier. Microsurgery 1987; 8: 197.
- Arikan S, Adas G, Barut G, Toklu AS, Kocakusak A, Uzun H, et al. An evaluation of low molecular weight heparin and hyperbaric oxygen treatment in the prevention of intra-abdominal adhesions and wound healing. Am j Surg 2005; 189: 155-160.
- Zhou J, Elson C, Lee TD. Reduction in postoperative adhesion formation and re-formation after an abdominal operation with the use of N, O - carboxymethyl chitosan. Surgery. 2004; 135: 307-312.
- Mazuji MK, Kalambaheti K, Pawar B. Prevention of adhesions with polyvinylpyrrolidone. Arch Surg 1964: 89; 10-11.
- Alimoglu O, Akcakaya A, Sahin M, Unlu Y, Ozkan OV, Sanli E, et al. Prevention of Adhesion formations following Repair of Abdominal wall defects with Prosthetic Materials. Hepatogastroenterology 2003; 50: 725-728.
- Boland GM, Weigel RJ. Formation and prevention of postoperative abdominal adhesions. J Surg Res 2006; 132: 3-12.
- Holmdahl L, Ericsson E, Ericsson BI, Risberg B. Depression of peritoneal fibrinolysis during operation is a local response to trauma. Surgery 1998; 13: 539-544.
- Voskerician G, Rodriguez A, Gingras PH. Macroporous condensed poly (tetra fluoro-ethylene) II. In vivo effect on adhesion formation and tissue integration. J Biomed Mater Res A. 2007; 82: 426-435.
- Burger JW, Halm JA, Wijsmuller AR, ten Raa S, Jeekel J. Evaluation of new prosthetic meshes for ventral hernia repair. Surg Endosc 2006; 20: 1320-1325.
- Leber GE, Garb JL, Alexander Al, Reed WP. Long-Term complications associated with prosthetic repair of incisional hernias. Arc Surg 1998; 133: 378-382.