Case Report - Case Reports in Surgery and Invasive Procedures (2017) Case Reports in Surgery and Invasive Procedures (Special Issue 1-2017)
Chronic iron deficiency anaemia after Roux-en-Y gastric bypass leading to Plummer Vinson syndrome.
- *Corresponding Author:
- Wesley Prichard
Department of Internal Medicine,St. Vincent Hospital Indianapolis,2001 W. 86th St, Indianapolis, IN 46260
Tel: 317-512-0185
Fax: 317-338-6359
E-mail: wesley.prichard@stvincent.org
Accepted date: December 23, 2016
Citation: Prichard W, Wilson S. Chronic iron deficiency anaemia after Roux-en-Y gastric bypass leading to Plummer Vinson syndrome. Case Rep Surg Invasive Proced. 2017;1(1):1-2.
Abstract
Plummer-Vinson Syndrome (PVS) is a rare condition that classically presents as a triad of dysphagia, proximal esophageal webs, and iron deficiency anemia. The prevalence of PVS has rapidly declined since it was first described by Henry Plummer and Stanley Vinson in the early 1900’s due to improved nutritional status and subsequent resolution of iron deficiency [1]. To our knowledge, only one prior case of PVS has been reported following gastric bypass surgery.
Keywords
Plummer Vinson syndrome, anaemia, Chronic iron deficiency.
Introduction
Plummer-Vinson Syndrome (PVS) is a rare condition that classically presents as a triad of dysphagia, proximal esophageal webs, and iron deficiency anemia. The prevalence of PVS has rapidly declined since it was first described by Henry Plummer and Stanley Vinson in the early 1900’s due to improved nutritional status and subsequent resolution of iron deficiency [1]. To our knowledge, only one prior case of PVS has been reported following gastric bypass surgery. PVS is most commonly observed among middle-aged Caucasian females, and only rarely is present among those of African descent. We report a unique case of PVS diagnosed during a workup for chronic iron deficiency anemia in an African-American patient with a prior history of gastric bypass surgery.
Case presentation
A 31-year-old African-American female status post Roux-en-Y gastric bypass surgery for morbid obesity in 2010 presented to the hospital in August 2016 with dysphagia of three to four weeks duration. She noted more discomfort with solid than liquid substances as well as epigastric pain. She reported often having to massage her anterior neck to help with passage of food. On review of systems she endorsed progressive burning sensation around her mouth and tongue, discoloration of her tongue, and worsening fatigue. She denied fever, chills, nausea, vomiting, diarrhea, chest pain, shortness of breath, melena, hematochezia, easy bruising, or rash. She was not taking any medications although she reported a history of previous iron supplementation more than two years ago which was selfdiscontinued due to constipation and dyspepsia.
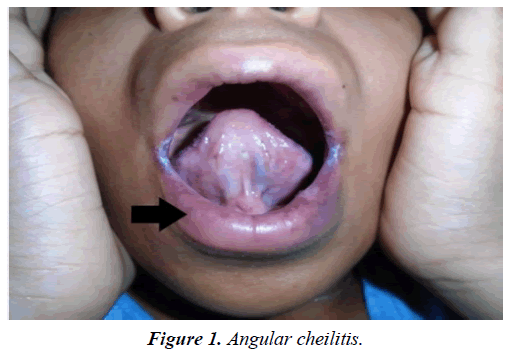
On physical examination, the patient was hemodynamically stable. She was observed to have significant conjunctival pallor as well as evidence of angular cheilitis (Figure 1).
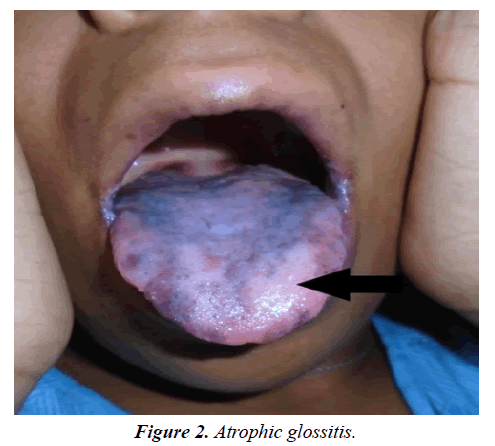
stomatitis, and atrophic glossitis with a hyperpigmented tongue and lower lip (Figure 2). Routine blood work demonstrated a severe microcytic, hypochromic anemia with hemoglobin of 7.4 g/L, mean corpuscular volume of 65, iron of 12 mcg/dL (normal 50 mcg/dL to 170 mcg/dL), total iron binding capacity of 428 mcg/dL (normal 228 mcg/dL to 428 mcg/dL), and ferritin of 6.6 ng/mL (normal 4.6 ng/mL to 204.0 ng/mL) findings consistent with severe iron deficiency anemia.
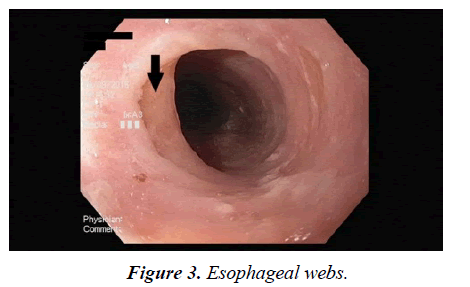
Testing for HIV and hepatitis B and C were negative. INR was within normal limits. Occult blood testing was negative. On further investigation, it was noted that the patient’s iron and ferritin levels four years prior were relatively unchanged from her current presentation. The patient underwent an upper endoscopy, which was significant for several proximal esophageal webs (Figure 3), ectopic gastric mucosa in the proximal esophagus, and inflammation at the gastrojejunal anastomosis site.
The patient underwent dilation of the esophageal webs with a Maloney dilator and was started on parenteral iron therapy indefinitely.
Discussion
PVS presents with the classic triad of iron deficiency anemia, dysphagia, and upper esophageal webs. The upper esophageal webs are depicted in Figure 3. Rarely reported among the African-American population, this is one of the first cases that we have identified in the literature-especially among the patient population that has undergone Roux-en-Y gastric bypass surgery [2,3]. Angular chelitis and atrophic glossitis are other common exam findings in PVS patients [4]. The pathogenesis is not well understood in any population presenting with PVS: perhaps the gastric bypass predisposed the patient to a decreased propensity for iron absorption. Roux-en-Y gastric bypass surgery involves separation of the antrum from the proximal gastric pouch; in doing so this may disrupt the conversion of ferric to ferrous iron as the gastric acid secretion typically coming from the parietal cells of the antrum [5]. Additionally, it has been observed that gastric bypass impairs oral heme absorption from occurring at the level of the duodenum due to a delayed interaction of pancreatic enzymes and biliary secretions [6]. Treatment for PVS includes iron supplementation initiation as well as dilation of esophageal webs as was done in our patient. These patients need additional surveillance after diagnosis due to an increase risk of squamous cell carcinoma of the pharynx and esophagus [1-6]. Although the pathophysiology and etiology of PVS development among patients with chronic iron deficiency anemia that have undergone gastric bypass are unclear, we offer this case of PVS and mechanism for awareness in future gastric bypass patients with iron deficiency and dysphagia. Practitioners should be vigilant in their adherence to the American Society for Metabolic and Bariatric Surgery (ASMBS) guidelines to eliminate preventable complications in post-Roux-en-Y patients [7].
References
- Novacek G. Plummer-Vinson syndrome. Orphanet J Rare Dis.2006;(36):1-36.
- Uysal A, Arora S, Tapolyai M (2007) Plummer-Vinson syndrome in a black female. Internet J Gastroenterol. 7(1).
- Sapthavee A, Kircher ML, Akst LM (2014) Plummer-Vinson syndrome following gastric bypass surgery. Ear Nose Throat. 93:E15.
- Singh A, Yuwanati M, Umarji H. Plummer-Vinson Syndrome. J Oral Health Res.2014;(4):13-8.
- Love AL, Billett HH. Obesity, bariatric surgery, and iron deficiency: True, true, and related. Am J Hematol.2013;(83):403-9.
- Rasool I, Begum R, Ravichandra K. Revisiting Plummer Vinson Syndrome: A report of three cases and review. Malta Med J. 2014;(26):37-41.
- Allis L, Blankenship J, Buffington C. ASMBS allied health nutritional guidelines for the surgical weight loss patient. Surg ObesRelatDis.2008;(4):73-108.