- Biomedical Research (2013) Volume 24, Issue 2
Changes of matrix metalloproteinase-9 and tissue inhibitors of metalloproteinase- 1 during left ventricular remodeling in acute myocardial infarction patients after percutaneous coronary intervention
Shifang Ding*, Huijian Liu, Qing Lu, Zhigang Gong, Juquan Jiang, Zhinan Chen, Zhigang Li, Renxue WangDepartment of Cardiology, Wuhan GenAeral Hospital of Guangzhou Military Region, Wuhan, Hubei 430070, China
- *Corresponding Author:
- Shifang Ding
Department of Cardiology
Wuhan GenAeral Hospital of Guangzhou Military Region
Wuhan, Hubei 430070, China
Tel: +8627-68878415
E-mail: ddyou1234@hotmail.com
Accepted date: December 27 2012
Abstract
The study was to investigate the changes in matrix metalloproteinase-9 (MMP-9) and tissue inhibitors of metalloproteinase-1 (TIMP-1) in acute myocardial infarction (AMI) patients after percutaneous coronary intervention (PCI) and to explore their correlation to recent left ventricular remodeling (LVRM) and cardiac function. A total of 98 AMI patients were recruited of whom 51were admitted within 12 h and treated with PCI immediately (Group A), 22 were admitted at 12 h after AMI and treated with delayed PCI when the disease condition was stable(Group B), and the remaining 25 received conservative therapy(Group C). In Group D, 20 healthy subjects were enrolled. Two-dimensional echocardiography was performed to detect the end diastolic volume (EDV), end systolic volume (ESV), left ventricular ejection fraction (LVEF), left ventricular end diastolic diameter (LVDd) and ventricular aneurysm. In Group A, MMP-9 significantly increased after PCI, but returned to nearly normal level at 7 days after AMI. The MMP-9 level in Group A was markedly different from that in Groups B and C (P<0.05). At 90 days after AMI, examination revealed the EDV, ESV, LVDd and LVEF in Groups A and B were superior to those in Group C (P<0.05). The MMP-9 on day 7 was positively related to the EDV (r=0.261, P<0.05) and ESV(r=0.340, P<0.05) but negatively to LVEF (r=-0.218, P<0.05) on day 90. So we concluded that expression increases at early stage of AMI. During the LVRM, MMP-9 is positively associated with EDV and ESV but negatively with LVEF.
Keywords
percutaneous coronary intervention; Matrix metalloproteinase-9; Tissue inhibitors of metalloproteinase-1; Acute myocardial infarction; Left ventricular remodeling
Introduction
After acute myocardial infarction (AMI), compensation process is initiated and left ventricular remodeling (LVRM) is also activated which is characterized by thinning and elongation of infarct ventricular wall resulting in protrusion of infarct ventricular wall. However, the non-infarct ventricular wall thickens and elongates as a response. Both processes lead to progressive dilation and transformation of left ventricle accompanied by compromised cardiac function. During the LVRM, apart from the abnormalities in structure, metabolism and function of myocardial cells, the production and deposition of extracellular matrix (ECM) are also aberrant. In the presence of hydrolysis by matrix metalloproteinases (MMPs), the production and degradation of ECM remain at a balanced level. Tissue inhibitors of metalloproteinases (TIMPs) are endogenous specific inhibitors of MMPs [1-3]. Coronary artery recanalization and myocardial reperfusion therapy such as thrombolysis and percutaneous coronary intervention (PCI) may savage the ischemic myocardium, reduce infarct area and protect left cardiac function if this treatment can be applied soon after AMI. In the present study, the effects of emergency PCI, delayed PCI and conservative therapy on LVRM and cardiac function was compared in the AMI patients. This study aimed to explore the biological mechanisms underlying the prevention of LVRM by PCI, which was further elucidated at the level of MMPs and their inhibitors. In our study, the changes in MMP-9 and TIMP-1 were investigated in AMI patients and their relations to LVRM and cardiac function were also evaluated. Our findings suggest that MMP-9 and TIMP-1 play important role in the prediction of post-AMI LVRM and cardiac function.
Patients and Methods
Patients
A total of 98 patients with initial AMI were recruited from the Department of Cardiology in our hospital from March 2010 to November 2010. There were 70 males(71.4%) and 28 females (28.6%). Of these patients, 51 were admitted within 12 h after AMI and emergency PCI was administered (Group A); 22 were admitted at 12 h after AMI and delayed PCI was performed (Group B); 25 patients received conservative therapy (Group C). In the same period, 20 subjects without evident stenosis of coronary artery on coronary angiography served as controls (Group D). There were no marked differences in gender, age, concomitant diseases (diabetes, hypertension, hyperlipidemia) and risk factors of AMI (smoking) among groups. Inclusion criteria included 2 of 3 items: patients had typical chest pain; electrocardiography (ECG) showed elevation of ST segment was ≥ 0.2 mv (millivolt) in chest lead and ≥ 0.1 mv in limb lead; creatine kinase isoenzyme was two folds higher than that of upper limit of normal. Exclusion criteria: AMI patients had old myocardial infarction, underwent thrombolysis, had connective tissue diseases, secondary myocardial rupture/ perforation or chordal rupture and severe valvular diseases, received invasive cardio- pulmonary resuscitation, had severe liver and kidney dysfunction, active hemorrhage, contrast agent allergy, trauma and malignancies and underwent major surgery. Patients who had infective of inflammatory state or scurvy who could not recall the time of sustained chest pain were also excluded. Criteria for success PCI: thrombolysis in myocardial infarction (TIMI) III flow was present in the coronary artery, the diameter of stenotic artery was reduced by ≤20%, patients had no operation related complications (such as death) and a second AMI was not noted.
Treatment
In Group A, patients were administered with oral aspirin (300 mg) and oral clopidogrel (600 mg) immediately after admission and PCI was subsequently performed for the recanalization of stenotic arteries (Innova 2000 cardiovascular imaging machine). In Group B, patients received delayed PCI. Patients in Group C underwent conservative pharmacotherapy. For each patient, medical history was reviewed, physical examination performed and measurement of myocardium specific enzymes as well as ECG was also done. Patients also received intensive pharmacotherapy once they had no contradictions: aspirin, clopidogrel, nitrates, angiotensin-converting enzyme inhibitors, angiotensin receptor inhibitors, β receptor blockers, Statins, etc. Following PCI, patients were treated with aspirin at 300 mg/d and thereafter 100 mg/d 3 months later and with clopidogrel at 75 mg/d for at least 1 year.
Observations and evaluation
Peripheral venous blood (6 ml) was collected on admission and at 12 h, 7 d and 90 d after AMI followed by centrifugation at 3000 r/min for 10 min. The supernatant was collected and stored at -8°C. Enzyme-linked immunosorbnent assay (ELISA) was employed to measure the MMP-9 (detection limit: 0~10 ng/ml) and TIMP-1 (detection limit: 0~10ng/ml) according to the manufacturer’s instructions (Wuhan Boster, Biotech Co., Ltd). Two-dimensional echocardiography and detection of cardiac function (Agilent HP5500 Cardiac Ultrasound Detector; probe frequency: 2-4MHz) were performed within 7~10 d after admission and 3 months after AMI. Two-plane or Simpson method was applied to calculate the end diastolic volume (EDV), end systolic volume (ESV), left ventricular ejection fraction (LVEF) and left ventricular end diastolic diameter (LVDd). In addition, myocardial ventricular aneurysm was also detected.
Statistical analysis
Statistical analysis was performed with SPSS version 13.0
statistics package. Quantitative data were expressed as
mean ± standard deviation ( ±s). Comparisons were
done with Games Howell (heterogeneity of variance) or
LSD method (homogeneity of variance) between two
groups or with one way analysis of variance (ANOVA)
among 3 groups. t test or repeated measures analysis of
variance was employed for comparisons between before
and after treatment. Qualitative data were compared with
chi square test. Correlation was evaluated with Pearson
linear correlation analysis. A value of P<0.05 was considered
statistically significant.
±s). Comparisons were
done with Games Howell (heterogeneity of variance) or
LSD method (homogeneity of variance) between two
groups or with one way analysis of variance (ANOVA)
among 3 groups. t test or repeated measures analysis of
variance was employed for comparisons between before
and after treatment. Qualitative data were compared with
chi square test. Correlation was evaluated with Pearson
linear correlation analysis. A value of P<0.05 was considered
statistically significant.
Results
Levels of MMP-9 and TIMP-1
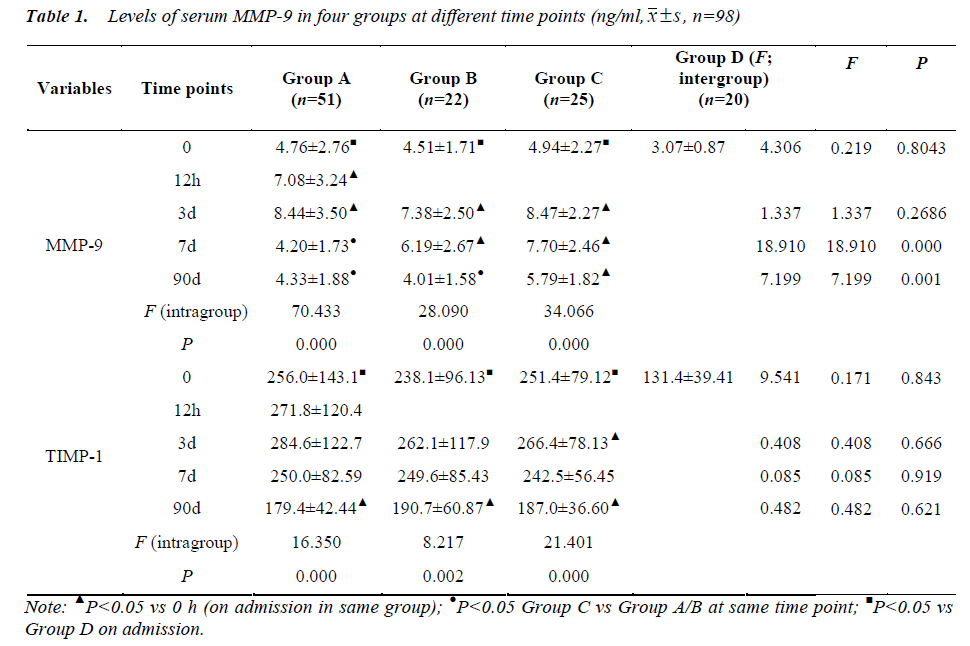
When compared with controls, the levels of MMP-9 and TIMP-2 were marked increased in Groups A, B and C after admission (F=4.306 and 9.541, respectively, P<0.05). In Group A, the MMP-9 increased again after PCI but returned to the level on admission at 7 d after AMI, which was markedly different from that in Groups B and C (P<0.05). The TIMP-1 level in Group A at 7 d after AMI was still significantly higher than that in controls (P<0.05), and but that at 90 day (d) after AMI reduced to a certain extent. In Group B, the MMP-9 level at 7 d after AMI was still higher than that on admission and that on day 90 returned to the level on admission, which was still marked higher than that in Group C (P<0.05). The TIMP-1 level was consistently higher than that in controls (P<0.05). In Group C, the levels of MMP-9 and TIMP-1 were consistently higher than that in Group D (P<0.05) (Table 1). Meanwhile, we found that MMP-9 and TIMP-1 data at each time point were not easy to analysis and also made no sense.
Findings on echocardiography
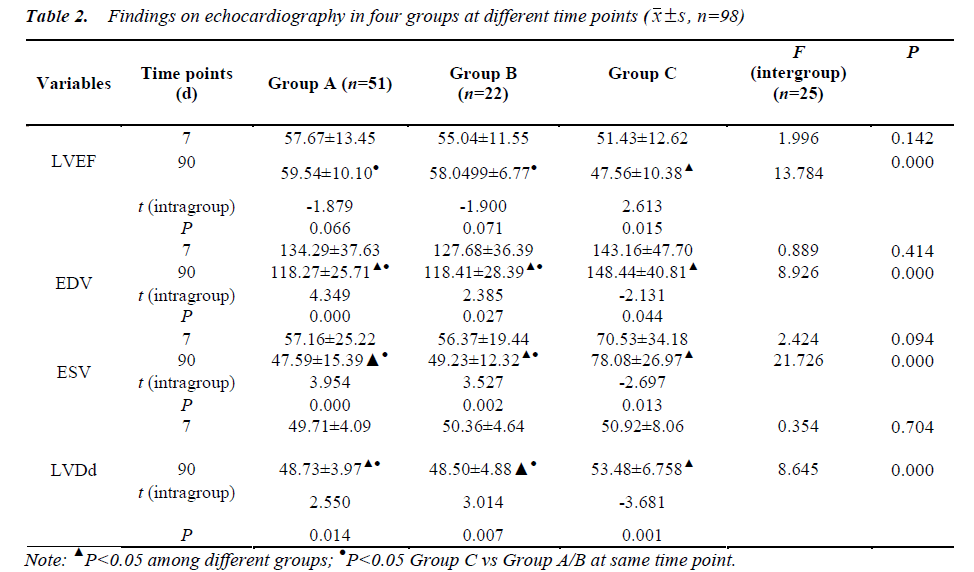
At 7 d after AMI, there were no marked differences in LVEF, EDV, ESV and LVDd among Groups A, B and C. At 90 d after AMI, the levels of LVEF, EDV, ESV and LVDd in Groups A and B were markedly higher than those in Group C (P=0.000). The LVEF level in Group A and B was significantly increased when compared with Group C at 90 d after AMI (P=0.000). No significant differences were noted in the LVEF, EDV, ESV and LVDd between Group A and Group B (P>0.05). In Groups A and B, the levels of EDV, ESV and LVDd at 90 d after AMI were dramatically reduced when compared with those at 7 d after AMI, but the increase of LVEF was not statistically significant. In Group C, the levels of EDV, ESV and LVDd at 90 d after AMI were significantly increased when compared with those at 7 d after AMI, but LVEF level dramatically reduced. There was no significant difference in the myocardial ventricular aneurysm among Groups A, B and C (Table 2).
Correlation between MMP-9 level and findings on echocardiography
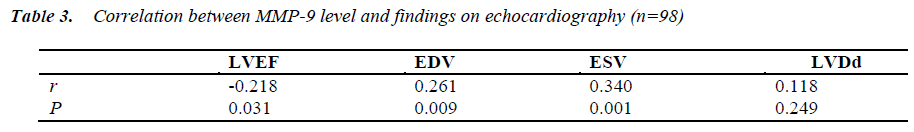
The MMP-9 at 7 days after AMI was positively related to EDV (r=0.261, P=0.009) and ESV (r=0.340, P=0.001) but negatively to LVEF (r=-0.218, P=0.031) at 90 days after AMI, and not related to LVDd (P=0.249) (Table 3).
Discussion
Following AMI, the LVRM may lead to progressive dilation and transformation of left ventricle and subsequentcompromise of cardiac function. During the post-AMI LVRM, there are abnormalities in not only myocardial cells but ECM. The ECM is crucial for the maintenance of arrangement of myocardial cells, coordination of myocardial contractibility, and the maintenance of geometrical shape of left ventricle. Under the hydrolysis of MMPs, the re-arrangement and degradation of ECM is maintained at a balanced level. TIMPs are endogenous inhibitors of MMPs. Few clinical studies have been conducted to investigate the role of ECM and MMPs in the LVRM following AMI [1-3].
Our findings indicated that the levels of MMP-9 and TIMP-1 on admission in different patients with AMI were markedly higher than those in controls (P<0.05), which suggests MMP-9 may be related to the instability of coronary plaques [4] and has promise to become an important predictor of AMI. In Group A, the MMP-9 increased again following PCI, which may be attributed to the plaque rupture and damage to blood vessels after balloon dilation and stenting. In Group A, the MMP-9 at 7 d after AMI returned to the level on admission and significantly different from that in Groups B and C (P<0.05), but the TIMP-1 level was still significantly higher than that in controls and reduced at 90 d after AMI. In Group B, the MMP-9 level at 7 d after AMI was markedly higher than that on admission and retuned to the level on admission at 90 d after AMI but was significantly different from that in Group C (P<0.05). The TIMP-1 level began to reduce at 90 d after AMI. In Group C, the levels of MMP-9 and TIMP-1 remained higher than those on admission and in the controls, and the TIMP-1 level start to reduce at 90 d after AMI. These findings suggest PCI can shorten the duration of increased MMP-9 and promote the reduction of MMP-9 when compared with pharmacotherapy alone, and this effect is more evident following emergency PCI as compared to selective PCI.
Detection of cardiac function revealed there were no marked differences in LVEF, EDV, ESV and LVDd at 7 d after AMI among Groups A, B and C. At 90 d after AMI, the levels of LVEF, EDV, ESV and LVDd in Groups A and B were markedly lower than those in Group C (P<0.05). However, the LVEF level in Groups A and B was higher than that in Group C. No marked differences were not observed in LVEF, EDV, ESV and LVDd between Groups A and B (P>0.05). In addition, the levels of EDV, ESV and LVDd at 90 d after AMI were significantly lower than those at 7 d after AMI, and the LVEF level increased without marked difference. In Group C, the levels of EDV, ESV and LVDd at 90 d after AMI were significantly higher than those at 7 d after AMI and LVEF dramatically reduced. There was no significant difference in the ventricular aneurysm among Groups A, B and C. The ventricular aneurysm at 90 d after AMI was higher than that at 7 d after AMI but without significant difference. The principles for the treatment of AMI is to recanalize ischemia-reperfusion artery (IRA) to assure myocardial perfusion, prevent myocardial necrosis, protect cardiac function, reduce ventricular remodeling and improve the short-term and long-term prognosis [5]. At the early stage of acute IRA, recanalization is an important predictor of survival [6,7]. Our findings indicated, when compared with pharmacotherapy, PCI could significantly inhibit LVRM and improve cardiac function, but no marked difference was noted between emergency PCI and selective PCI in the therapeutic efficacy. This may be attributed to short follow up period (3 months). No marked differences in the LVEF and ventricular an eurysm may also be related to the short follow up period. These findings suggest, at early stage of AMI, EDV, ESV and LVDd were more sensitive to treatment as compared to LVEF and ventricular aneurysm. When compared with pharmacotherapy, delayed PCI can significantly improve the cardiac function but the therapeutic efficacy of delayed PCI was comparable to that of emergency PCI. Thus, for patients unsuitable for emergency PCI, delayed PCI is still required and beneficial for the prognosis. There is evidence showing that delayed recanalization is beneficial for the improvement of prognosis although it may not benefit the reduction of AMI [8,9].
In addition, the correlation between serum MMP-9 and findings on ultrasonography was also evaluated. Results revealed the MMP-9 level at 7 d after AMI was positively to EDV and ESV but negatively to LVEF at 90 d after AMI. However, these were not associated with LVDd. These findings indicate serum MMP-9 at 7 d after AMI can be used to reflect the myocardial remodeling and predict the recovery of cardiac function following AMI. Moreover, this also demonstrates that MMP-9 plays an important role in the maintenance of myocardial structure and function. Whether MMP inhibitors can be applied in the prevention of ventricular remodeling following AMI is required to be further demonstrated [10-15].
Our findings indicate: 1) MMP-9 level increases at early stage of AMI and increased MMP-9 level may continue for 1 week to several months and reperfusion therapy may reduce the MMP-9 level and shorten the duration of increased MMP-9; 2) During LVRM after AMI, MMP-9 level is positively related to EDV and ESV and negatively to LVEF. MMP-9 may become an important predictor of AMI onset and ventricular remodeling after AMI; 3) Emergency PCI aiming to recanalize stenotic blood vessels is helpful for improvement of cardiac function and delayed PCI is still beneficial for suppression of ventricular remodeling; 4) At early stage of ventricular remodeling following AMI, the EDV, ESV and LVDd are more sensitive to treatment than LVEF and ventricular aneurysm.
References
- Kelly D, Khan SQ, Thompson M, Cockerill G, Ng LL, Samani N. Plasma tissue inhibitor of metalloproteinase-1 and matrix metalloproteinase-9: novel indicators of left ventricular remodelling and prognosis after acute myocardial infarction. Eur Heart J 2008; 29(17): 2116- 2124.
- Zhang P, Yang YJ, Chen X. Comparison of doxycycline, losartan, and their combination on the expression of matrix metalloproteinase, tissue inhibitor of matrix metalloproteinase, and collagen remodeling in the noninfarcted myocardium after acute myocardial infarction in rat. J Chin Med Acad 2005; 27(1): 53-61.
- Yasuda S, Miyazaki S, Kinoshita H, Nagaya N, Kanda M, Goto Y, et al. Enhanced cardiac production of matrix metalloproteinase-2 and -9 and its attenuation associated with pravastatin treatment in patients with acute myocardial infarction. Clin Sci (Lond) 2007; 112 (1): 43-49.
- Furenes EB, Arnesen H, Solheim S, Grogaard HK, Hoffmann P, Seljeflot I. The profile of circulating metalloproteinases after PCI in patients with acutemyocardial infarction or stable angina. Thromb Res 2009; 124(5): 560-564.
- Polonski L, Gasior M, Wasilewski J, Wilczek K, Wnek A, Adamowicz-Czoch E. Outcomes of primary coronary angioplasty and angioplasty after initial thrombolysis in the treatment of 374 consecutive patients with acute myocardial infarction. Am Heart J 2003; 145(5): 855- 861.
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003; 361(9351): 13-20.
- Saia F, Lemos PA, Lee CH, Arampatzis CA, Hoye A, Degertekin M. Sirolimus-eluting stent implantation in ST-elevation acute myocardial infarction: a clinical and angiographic study. Circulation; 108(16): 1927-1929.
- Hirayama A, Kusuoka H, Adachi T, Sakai A, Ueda Y, Okuyama Y. Comparison of time of reperfusion during anterior wall acute myocardial infarction to left ventricular volume one month and 20 months later. Am J Cardiol; 89(12): 1335-1340.
- Sadanandan S, Buller C, Menon V, Dzavik V, Terrin M, Thompson B, et al. The late open artery hypothesis--a decade later. Am Heart J; 142(3): 411-421.
- Jiang B, Chen J, Xu L, Gao Z, Deng Y, Wang Y. Salvianolic acid B functioned as a competitive inhibitor of matrix metalloproteinase-9 and efficiently prevented cardiac remodeling. BMC Pharmacol 2010; 10: 10.
- Krishnamurthy P, Peterson JT, Subramanian V, Singh M, Singh K. Inhibition of matrix metalloproteinases improves left ventricular function in mice lacking osteopontin after myocardial infarction. Mol Cell Biochem 2009; 322(1-2): 53-62.
- Kandalam V, Basu R, Abraham T, Wang X, Awad A, Wang W. Early activation of matrix metalloproteinases underlies the exacerbated systolic and diastolic dysfunction in mice lacking TIMP3 following myocardial infarction. Am J Physiol Heart Circ Physiol 2010; 299(4): H1012-1023.
- Miyazaki S, Kasai T, Miyauchi K, Miyazaki T, Akimoto Y, Takagi A. Changes of matrix metalloproteinase-9 level is associated with left ventricular remodeling following acute myocardial infarction among patients treated with trandolapril, valsartan or both. Circ J 2010; 74(6): 1158-1164.
- Shu T, Zeng B, Ren X, Li Y. HO-1 modified mesenchymal stem cells modulate MMPs/TIMPs system and adverse remodeling in infracted myocardium. Tissue Cell 2010; 42(4): 217-222.
- Reddy VS, Prabhu SD, Mummidi S, Valente AJ, Venkatesan B, Shanmugam P. Interleukin-18 induces EMMPRIN expression in primary cardiomyocytes via JNK/Sp1 signaling and MMP-9 in part via EMMPRIN and through AP-1 and NF-kappaB activation. Am J Physiol Heart Circ Physiol 2010; 299(4): H1242-1254.