Research Article - Biomedical Research (2017) Volume 28, Issue 11
Application of retcam III wide-field fundus imaging in screening of retinoblastoma
Shaofen Lin1#, Wei Sun2#, Lin Lv1, Xiujuan Zhao1, Yuxiang Mao1* and Shibo Tang3*
1Zhongshan Ophthalmic Center, Sun Yat-Sen University, Guangzhou, PR China
2Guangdong Women and Children Hospital, Guangdong Sheng, PR China
3Aier School of Ophthalmology, Central South University, PR China
#These authors contributed equally to this manuscript
- *Corresponding Author:
- Yuxiang Mao
Zhongshan Ophthalmic Center
Sun Yat-Sen University, PR China
Shibo Tang
Aier School of Ophthalmology
Central South University, PR China
Accepted on April 11, 2017
Abstract
Background: To investigate value of Retcam III in screening and follow-up of Retinoblastoma (RB) in infants.
Method: A total of 395 infants with orbital tumors who were treated as outpatients and received 130º wide-field Retcam III fundus imaging in our unit between July 2013 and September 2014 were reviewed. They underwent Retcam III fundus imaging for both eyes under topical anesthesia after mydriasis was adequately induced by compound Tropicamide eye drops. Data were documented and analysed.
Result: A total of 395 infants cooperated and completed RB screening, of which 147 were found to have RB.
Conclusion: Retcam III is not only useful in the screening and follow-up of RB in infants, but also facilitates early discovery of RB and regular follow-up after treatment. Thus it is a safe and effective approach. The cooperation between physician and patient is the key to a successful imaging.
Keywords
Wide field retcam III, Retinoblastoma, Cooperation between physician and patient
Introduction
Retinoblastoma (RB) is the most common intraocular malignant tumor in infants, posing significant threat to visual acuity and well-being of infants. Its early screening, diagnosis and treatment have caught more and more attention among ophthalmologists in recent years. With progression in modern diagnostic and therapeutic technology, treatment goal and pattern for RB have been changed [1]. Retcam III has important role in grading/treatment [2] and follow-up of RB. Retcam III wide-field fundus imaging is a safe and reliable screening method for early discovery of fundus diseases. It provides wide-field visualization of retina as well as highdefinition and real-time image, and allows for observation and recording of fundus image in infants. The accuracy of examination allows doctors to establish further treatment regimen for infants with RB according to changes in condition of the fundus. In addition, it helps doctors visualize the RB tumor at different phases. Retcam III wide-field imaging system and fundus imaging technology provide strong support for the diagnosis and treatment of RB.
Study Subjects
A total of 395 infants with orbital tumors who were treated as outpatients and came to our unit for screening examination with Retcam III in the Zhongshan Ophthalmic Center between July 2013 and September 2014 were collected, of which 147 were diagnosed with RB. These included 246 males and 149 females. Age ranged between one (1) month to seven (7) years, averagely 2.44 years.
Main Instruments
Ophthalmic wide-field imaging system Retcam III (Clarity Medical System. Inc. USA) and pediatric blepharostat.
Methods
Education before examination
Precautions before, during and after examination were explained to parents, ensuring they fully understood (please refer to Precautions set forth by our unit). Good communication between doctor and patient could build up parent’s trust and lay foundation for the cooperation. Older infants and children should be given more encouragement and praise, telling them it was just going to take a picture of their eyes, and explaining to them steps of the examination in simple words, so as to alleviate their fear and ensure good cooperation. During examination, let parents distract the infants by talking to them. Before examination, medical history was taken carefully, including birth weight and family history.
Preparation before examination
Before examination, infants aged below six (6) months should fast over 1-2 h before examination, so as to avoid vomiting and subsequent asphyxia during examination. For those aged above 6 months who would not cooperate, a dose of 10% choral hydrate (0.5=0.8 mg/kg, 50-80 mg/kg) was administered orally after confirmation of mydriasis.
Before examination with Retcam III, compound tropicamide eye drops were applied to induce adequate mydriasis. Before inducing mydriasis, medical chart and medical order were checked, and pupils examined again. Eye drops were applied a total of 3-4 times at 15 min intervals. After each application, lacrimal sac was pressed for 1-2 min, so as to prevent the eye drops from flowing into nasopharynx and being absorbed via mucosa, causing toxication. When pupils were dilated to 6-8 mm, tetracaine hydrochloride eye drops were applied to induce topical anesthesia.
The probe of the imaging system was cleaned using 75% alcohol, and was air dried (or cleaned using sterile water). The probe was then visually examined for any defects. Light intensity and focal length were modified.
Preparation for the infants: Young infants were wrapped with a bed sheet, with their extremities immobilized. The infants were placed in supine position, with their heads immobilized by the hands of a guardian who was present during examination.
Examination
Eye lids were kept open using a sterilized pediatric blepharostat: Ofloxacin eye cream was applied to prevent dryness of corneal epithelium and ocular surface abrasion. During the examination, let parents talk to the patient so as to distract them.
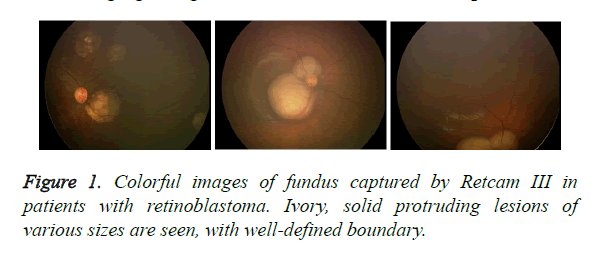
Images were captured in the following order: optic disc, macula lutea, temporal region, upper region, nasal region, and lower region. Distribution of tumor was observed using the monitor. Examiner could capture image and modify focal length using the paddle. Fundus (Figure 1) was examined using Retcam III. Before examination, patient information, including name, gender, date of birth, and weight, was input into the Retcam III program. During examination, retina was examined, starting from the right eye and then left eye, and starting from posterior optic disc, and then macula lutea, nasal, upper, temporal and lower regions, with images captured accordingly. Tumor was observed for its location, size and distribution over the monitor. For patients receiving repeated examination, change of tumor size after treatment should be carefully observed, as well as the presence of calcification, atrophy and new tumor formation. Examiner could capture images and modify focal length using the paddle. After imaging, images were selected, archived and printed. Examination with Retcam III proved successful even in neonates.
Cooperation between physician and patient before, during and after examination: it was crucial that the parents cooperated. During examination, the infants were carefully monitored for their conditions, including appearance, breathe, lip color, and change in sound of crying. Airway was maintained. In case of vomiting, examination was terminated; the patient was held in upright position, with their back patted gently. Resuscitation was started in case of emergency.
Neomycin eye drops were applied after examination.
The used probe was cleaned with 75% alcohol.
After imaging, images were selected, archived and printed.
Results
A total of 395 patients cooperated and completed their screening for RB, and 147 were confirmed to have RB. Retcam III is not only useful in screening and follow-up of RB in infants, but also facilitates early discovery of RB and regular follow-up after treatment. It is thus a safe and effective approach. Cooperation between doctor and patient is crucial. The accuracy of the examination allows doctors to establish further treatment regimen for infants with RB according to changes of the condition. Moreover, it allows doctor to visualize the changes in the tumor at different phases. Retcam III wide-field imaging system and fundus imaging technology provide strong support for the diagnosis and treatment of RB.
Discussion
Retinoblastoma (RB) is the most common intraocular malignant tumor in children, with an incidence of 1/17,000, accounting for 4% of all malignant tumors in children. Worldwide, there are 5,000 newly diagnosed cases of RB every year [3,4]. Children have higher chance of survival if RB is caught early and treated timely [5,6]. However, fundoscopy in infancy is complicated and difficult; therefore early diagnosis and timely treatment have become a critical but difficult step in the management of RB.
In developed countries, such as America, survival of RB patients has exceeded 95%, while worldwide, mean survival for RB patients is roughly 50%. The disparity of survival is mainly explained by the fact that RB is accurately caught at early phase in developed countries, while in less developed regions RB is often found only when tumor has invaded a major portion of the eyeball or orbit or intracranial structure [7]. Due to young age, neonates and infants can’t describe their eye discomfort with words, and early lesion could only be found by examination.
Early diagnosis and timely treatment not only save a patient’s life, even preserve partial vision in some cases. When early tumor is very small or is located in peripheral region, conventional fundoscopy might fail to identify them due to its narrow visualization field. Also, it can’t provide archival of images. As the tumor grows, leukocoria and strabismus appear (20%) [8]. Tumors that involve macula lutea can cause irreversible visual loss. As the disease progresses, patients might suffer exophthalmos, and life-threatening extra-orbital metastasis in severe cases.
Previously, the diagnosis of RB was generally based on fundoscopy and ultrasonography. Calcification inside the tumor is a gold standard in ultrasonography-based diagnosis. However, patients who have not yet developed calcification are often considered to have Coat’s disease [9,10] or angioma; RB is thus unnoticed, and best treatment timing slips away. Ultrasonography is very useful in confirming the size of the tumor. Yet, it will be difficult to catch the disease by ultrasonography when there is no significant calcification or there is only small calcification in the tumor. At this point, CT scan is recommended. The shortcoming of CT scan is radiation, which would cause a second tumor in sensitive individuals. MRI scan [11,12] is associated with less radiation, but it requires much cooperation of the patients, who must remain extremely calm during the scanning. For younger children, it may necessitate sedation, and even anesthesia. On the other hand, it is expensive. Therefore, it is not a proper approach for screening.
In early RB, a typical fundus sign is whitish creamy tumor surrounded by angioma-like vascular dilation. Other fundus findings include number, size, and thickness of tumor, its distance to optic disc and macula lutea, the presence of subretinal fluid, and subretinal and vitreous seeding. These are very important for the diagnosis, treatment and prognosis prediction of the disease. Therefore, early discovery and timely prevention and treatment are crucial in improving survival and preserving vision for the patients.
The RetCam III wide-field imaging system (Clarity Medical Systems. Inc. USA) is very valuable in confirming the size and location of the tumor. RetCam III provides 130º full range scanning of the fundus, and allows for real-time recording of high definition images. In addition, the system is equipped with various lens combinations. Different lens combinations may be used for different location and different visualization effect, so as to obtain more amplified image. Good visualization and recording are possible even for small tumors and peripherally located tumors (Figure 1). Moreover, the system includes an image-comparing software, which can prove useful in monitoring changes of tumor size, especially in measurement of efficacy in patients receiving chemotherapy [13,14].
In our study, no Retcam III related complication was seen. This was related to a number of factors, including education before examination to inform fasting time and precautions, observation on vital signs during examination, strictly executed sterilization before and after examination, use of antibiotic as coupling agent, and attentive and careful operation. The American Academy of Ophthalmology has conducted study on nosocomial infection that occurred among patients receiving examinations, and concluded that human tears were not considered to contain massive amount of blood-borne viruses; therefore, it was not necessary to execute precautions against blood-borne viruses as set forth by the American Occupational Safety and Health Administration (OSHA), and chance was slim for contagious infection. In addition, as recommended by Center for Disease Control and Prevention (CDCP), we used 75% medical alcohol and then sterile water to clean the probe, so as to avoid abrasion to the corneal epithelium caused by residual disinfectant on the probe. Also, the use of antibiotic as coupling agent further decreased the possibility of infection. Hence, it is a rather safe examination approach.
Retcam III fundus imaging is associated with few complications. If the patient is not cooperative and touches the blepharostat, causing subconjunctival hemorrhage, Ofloxacin eye cream might be applied for 1 or 2 d. Furthermore, chloral hydrate could not be administered in consecutive doses within 24 h. In a Retcam III fundus imaging, mydriasis must be induced adequately, so as to allow discovery of peripheral RB lesion.
The third-generation wide-field retinal imaging system (Retcam III) is characterized by image capturing, user-friendliness, and vivid and archivable images, and is thus useful in screening and the follow-up of patients receiving treatment. It allows for clear visualization of fundus in infants and can easily and precisely identify lesions in peripheral locations. Better prevention and treatment and further research are of profound significance for this condition. Retcam III is a system worthy of widespread use in clinical screening of RB, providing convenience and assistance for the treatment. Physicians who are well-experienced in diagnosis of RB may confirm diagnosis based on typical signs of the tumor. The third-generation wide-field retinal imaging system (Retcam III) also captures fundus image, and is an important tool for image storage and comparison, clinical teaching and research. It has important value for the screening of RB. However, for the purpose of final confirmation, a number of auxiliary examinations, such as CT scan, ultrasonography, fluorescent imaging, pathology and physiology, are still necessary.
Acknowledgments
This work was supported by Medical Research Foundation of Guangdong Province (A2013214). A study funded by Project 973 (A2013CB967004).
Declaration of Interest
The authors declare that they have no conflict of interest.
References
- Li B, Sun XL. Recognize the value of the individually combined therapy for children with retinoblastoma. Zhonghua Yan Ke Za Zhi 2007; 43: 481-483.
- Shields CL, Mashayekhi A, Au AK. The international classification of retinoblastoma predicts chemoreduction success. Ophthalmology 2006; 113: 2276-2280.
- Moll AC, Kuik DJ, Bouter LM, Den Otter W, Bezemer PD. Incidence and survival of retinoblastoma in The Netherlands: a register based study 1862-1995. Br J Ophthalmol 1997; 81: 559-562.
- Doz F, Brisse HJ, Stoppa-Lyonnet D. Retinoblastoma.In: Pinkerton R, Plowman P, Pieters R (eds) Paediatr Oncol 2004; 323-338.
- Shields CL, Shields JA. Retinoblastoma management: advances in enucleation, intravenous chemoreduction, and intraarterial chemotherapy. Curr Opin Ophthalmol 2010; 21: 203-212.
- Abramson DH. Retinoblastoma in the 20th century: past success and future challenges the Weisenfeld lecture. Invest Ophthalmol Vis Sci 2005; 46: 2683-2691.
- Carol S, Sun H, Zhang J. Clinical manifestations and diagnosis of retiboblastoma. Chinese J Ocular Fundus Dis 2004; 20: 118-120.
- Balasubramanya R, Pushker N, Bajaj MS, Ghose S, Kashyap S. Atypical presentations of retinoblastoma. J Pediatr Ophthalmol Strabismus 2004; 41: 18-24.
- Shields JA, Shields CL, Parsons HM. Differential diagnosis of retinoblastoma. Retina 1991; 11: 232-243.
- Shields CL, Uysal Y, Benevides R, Eagle RC Jr, Malloy B. Retinoblastoma in an eye with features of Coats disease. J Pediatr Ophthalmol Strabismus 2006; 43: 313-315.
- Mehta M, Sethi S, Pushker N, Kashyap S, Sen S. Retinoblastoma. Singapore Med J 2012; 53: 128-135.
- de Graaf P, Goricke S, Rodjan F. Guidelines for imaging retinoblastoma: imaging principles and MRI standardization. Pediatr Radiol 2012; 42: 2-14.
- Shields CL, Shields JA. Retinoblastoma management: advances in enucleation, intravenous chemoreduction, and intraarterial chemotherapy. Curr Opin Ophthalmol 2010; 21: 203-212.
- Gobin YP, Dunkel IJ, Marr BP, Brodie SE, Abramson DH. Intra-arterial chemotherapy for the management of retinoblastoma: four-year experience. Arch Ophthalmol 2011; 129: 732-737.