Letter to Editor - Journal of Gastroenterology and Digestive Diseases (2016) Volume 1, Issue 2
Antithrombin: A possible new prognostic marker and therapeutic tool for acute pancreatitis?
- *Corresponding Author:
- Etrusca Brogi
Department of Anaesthesia and Intensive Care University of Pisa Italy
Tel: 0039050997608
Fax: 0039050997607
E-mail: etruscabrogi@gmail.com
Accepted date: November 30, 2016
Abstract
The clinical manifestations of acute pancreatitis (AP) range from a local inflammatory process to the more severe form, associated with a systemic inflammatory response. Only patients with severe AP require intensive care admission. AP is characterized by the systemic activation of protease cascades. This inappropriate intracellular activation of digestive enzymes leads to the release of cytokines, activation of coagulation, tissue ischemia and tissue necrosis. All these factors play a vital role in the worsening of AP as well as in the development of associated extra-pancreatic complications. Haemostasis is strongly influenced by this inflammatory cascade; indeed, the pathways of inflammation and coagulation are intimately linked. Consequently, the multiorgan failure of severe acute pancreatitis is often associated with sepsis and disseminated intravascular coagulation
The clinical manifestations of acute pancreatitis (AP) range from a local inflammatory process to the more severe form, associated with a systemic inflammatory response. Only patients with severe AP require intensive care admission. AP is characterized by the systemic activation of protease cascades. This inappropriate intracellular activation of digestive enzymes leads to the release of cytokines, activation of coagulation, tissue ischemia and tissue necrosis. All these factors play a vital role in the worsening of AP as well as in the development of associated extra-pancreatic complications. Haemostasis is strongly influenced by this inflammatory cascade; indeed, the pathways of inflammation and coagulation are intimately linked. Consequently, the multiorgan failure of severe acute pancreatitis is often associated with sepsis and disseminated intravascular coagulation [1].
Antithrombin III (AT) is a potent endogenous anticoagulant, but it has also remarkable anti-inflammatory properties. Antiinflammatory properties of AT involve direct interactions with cells (binding the syndecan-4) thus interfering with the intracellular signal induced by mediators and down-modulating the inflammatory response [2]. We believe that AT is a good prognostic factor to differentiate between serious and moderate AP [3], especially during the first 3 days of admission. The role of protease inhibitors in the treatment of mild or severe AP is still unclear, however, we reckon that AT might have a therapeutic effect in severe AP as well.
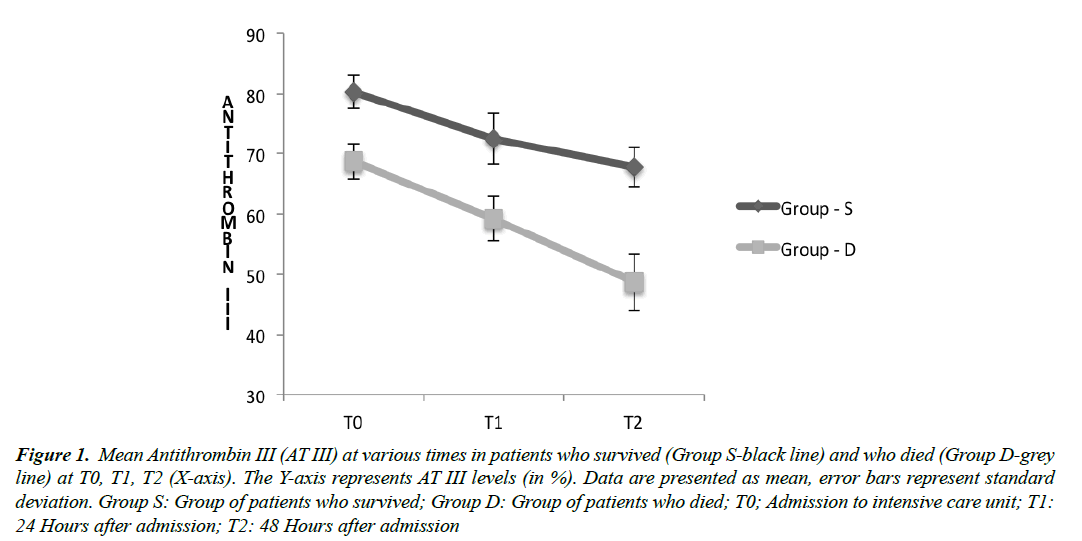
We conducted a pilot study to investigate whether AT could represent a useful prognostic marker for AP. We recruited 15 patients with the diagnosis of AP admitted to our intensive care unit. We excluded patients with a history of haematological disease, bleeding and/or thrombosis disease. AT was measured at admission (T0) and for up to 2 days (T1 and T2). We also calculated SAPS II at admission and SOFA score from T0 to T2. Out of 15 patients, 4 patients died and 8 required continuous renal replacement therapy. The group of patients who died (Group D) presented the higher value of SAPS II and SOFA at T0 and T1. In this group, we also observed a statistical significant difference between mean AT at TO (68.7 ± 2.9, %) and at T2 (48.7 ± 4.8, %; p=0.002). In the group of patients that survived (Group S), mean AT III at T0 was 80.3 ± 2.8 (%) whereas at T2 was 67.8 ± 3.18 (%; p=0.0001). Thus, there was a statistical significant difference between AT between T0 and T2 in both groups (Figure 1). Moreover, we compared mean AT between Group D and Group S; we observed a statically significant difference at T0 (P=0.0002) and also at T2 (P=0.0001) between these groups.
Figure 1: Mean Antithrombin III (AT III) at various times in patients who survived (Group S-black line) and who died (Group D-grey line) at T0, T1, T2 (X-axis). The Y-axis represents AT III levels (in %). Data are presented as mean, error bars represent standard deviation. Group S: Group of patients who survived; Group D: Group of patients who died; T0; Admission to intensive care unit; T1:24 Hours after admission; T2: 48 Hours after admission
We acknowledge the limitations of this initial report and intend to examine the prognostic value of AT further in a randomized blinded fashion. We did not investigate the possible therapeutic value of AT, however, we intend to analyse it in future trials. The impact of concomitant heparin treatment has to be analysed deeply as well. Definitely in the presence of heparin, the interaction between AT and its cellular receptor is impaired [4]. Thus, the anti-inflammatory characteristics of AT are weakened. However, we have to emphasise the usefulness of the AT and we recommend measuring it during the recovery of patients with AP.
References
- Badhal SS, Sharma S, Saraya A, et al. Prognostic significance of D-dimer, natural anticoagulants and routine coagulation parameters in acute pancreatitis. Trop Gastroenterol.2012; 33(3): 193-9.
- Roemisch J, Gray E, Hoffmann JN,Antithrombin: A new look at the actions of a serine protease inhibitor. Blood Coagul Fibrinolysis.2002; 13(8): 657-70.
- Las Heras G1, Roncalés FJ, Juncà J, et al. Antithrombin III: Its prognostic value in acute pancreatitis. Sangre (Barc).1992; 37(3): 165-8.
- Kienast J, Juers M, Wiedermann CJ, et al. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J Thromb Haemost. 2006; 4(1): 90-7.