Research Article - Biomedical Research (2017) Volume 28, Issue 11
Anatomy of the ligaments between the first cuneiform and the base of the second metatarsal and its clinical significance
Hui Zhu#, Chun-Guang Li#, Guang-Rong Yu*, Yun-Feng Yang and Bing Li
Department of Orthopaedics, Tongji Hospital, Tongji University School of Medicine, Shanghai, PR China
#These authors contributed equally to this work
- *Corresponding Author:
- Guang-Rong Yu
Department of Orthopaedics
Tongji Hospital
Tongji University School of Medicine, PR China
Accepted on March 21, 2017
Abstract
Background: This study aimed to investigate the anatomic characteristics of the ligaments between the first cuneiform and the base of the second metatarsal, which might improve the treatment of Lisfranc injury.
Methods: Twenty fresh foot specimens of normal adults were dissected. The length and width of the dorsal, plantar and Lisfranc ligaments were measured. Morphology of Lisfranc ligament and its origin on the first cuneiform were observed and investigated.
Results: The length and width of dorsal ligaments were 5.44 ± 0.83 mm and 4.20 ± 0.64 mm; those of plantar ligament were 7.07 ± 1.05 mm and 5.23 ± 1.10 mm; and those of Lisfranc ligament were 9.33 ± 1.34 mm and 8.00 ± 1.23 mm, respectively. The included angle between Lisfranc ligament and the proximal end of the shaft of the second metatarsal bone was 61.45 ± 5.03°. Lisfranc ligament was located on the lateral surface of the first cuneiform. The origin of Lisfranc ligament was 10.89 ± 0.84 mm away from the dorsal side of the first cuneiform, 8.31 ± 0.92 mm away from the plantar region, 5.35 ± 0.60 mm away from the distal end, and 12.04 ± 0.85 mm away from the proximal end.
Conclusions: The Lisfranc ligament is the largest one in the Lisfranc complex, plantar ligament is the second largest, and the dorsal ligament is the smallest. The internal fixation for the treatment of Lisfranc injury can be performed based on the location of the origin of Lisfranc ligament and the included angle between the ligament and the shaft of the second metatarsal bone.
Keywords
Second metatarsal bone, Tarsometatarsal joints, Lisfranc ligament, Applied anatomy
Introduction
The incidence rate of injury to tarsometatarsal joint (Lisfranc damage), which usually occurs in traffic accidents, has been gradually rising in recent years [1]. The Lisfranc joint with extremely delicate anatomic structure connects the forefoot and midfoot, and constitutes the transverse and longitudinal arches of the foot. In a broad sense, in addition to tarsometatarsal joint, Lisfranc joint includes intermetatarsal and tarsal joints. Together, they constitute Lisfranc joint complex. In a narrow sense, Lisfranc joint only includes the first and second tarsometatarsals and intercuneiform joints (no joint exists between the first and second metatarsals) [2]. The first and second tarsometatarsal joints are essential parts of the medial and middle columns in the tarsometatarsal joint, which are very important in maintaining stability of the midfoot. The most important joint is formed by the medial of second metatarsal and the lateral of the medial cuneiform bone. This joint, which is connected by the dorsal, Lisfranc and plantar ligaments, is the key to maintain the stability of the entire Lisfranc joint. The ligament structure of Lisfranc joint is very complex, of which the morphology, number, starting and ending points do not always remain the same, and commonly the actual anatomical structure is complex and variable in course, number, and insertions [3]. Panchbhavi et al. reported the location, dimensions, and variability in the position and surface area of the ligament attachment sites of Lisfranc ligament [4]. Ultrasound was used to diagnose injury of dorsal ligaments of the first/second metatarsal joint [5-7]. Thus, it is of clinical significance to investigate the anatomical characteristic of this structure. This research observed and investigated anatomical characteristics of the three ligaments between medial cuneiform and the base of the second metatarsal to provide anatomic evidence for the clinical treatment of trauma in the relevant parts.
Materials and Methods
Ethics statement
This research has been approved by the Ethics Committee of Tongji Hospital of Tongji University (2013-15-J), and that all subjects gave their consent to participate in this study.
Materials
Fresh foot specimens of twenty adults were included, of which 15 cases were from Department of Anatomy of Tongji University School of Medicine and five from the patients with traumatic amputation. The ratio of male to female was 13/7; ten were left foot and ten were right foot; and the average age was 59.3, ranging from 25.0-73.0 years. The specimens were cryopreserved at the -20ºC. X-ray imaging was used to exclude the cases with bone and joint degeneration, metabolic diseases, tumor, deformity, bone abnormalities and other conditions.
Measurement of structures
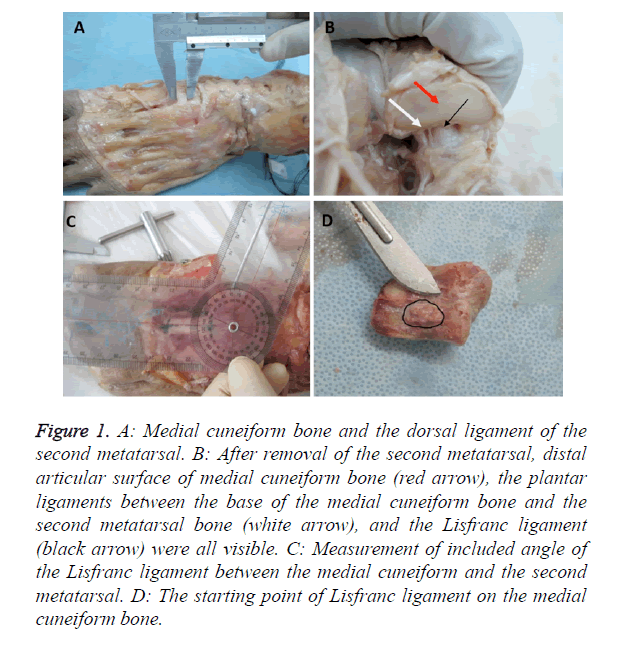
The first and second tarsometatarsal joints were dissected. The skin was incised and subcutaneous soft tissue was carefully dissected. During this process, we ensured the integrity of the anatomical structures that we intended to study. The transverse line connecting two midpoints of the end point of the ligament was used to measure the length. The widest part of the ligament was measured as the width of the ligament. For the direction of the ligament, the angle protractor was used to measure the included angle between the ligament and the proximal end of the selected baseline, which was the second metatarsal medial shaft. This measurement is accurate, accurate, and repeatable. During measurement, the midcourt line of second metatarsal backbone was used as the baseline. A Kirschner wire was implanted into the bone along ligament under direct vision. Then, the angle was between the Kirschner wire and the baseline. First, the data about the dorsal and metatarsal lateral ligaments were measured. Then the first metatarsal and intermediate cuneiform bone were removed to fully expose Lisfranc ligament for the measurement of its related data. Finally, the Lisfranc ligament was amputated to measure the distance from the original point to the upper/lower and front/rear edge of the outer side of the medial cuneiform bone (Figure 1).
Figure 1. A: Medial cuneiform bone and the dorsal ligament of the second metatarsal. B: After removal of the second metatarsal, distal articular surface of medial cuneiform bone (red arrow), the plantar ligaments between the base of the medial cuneiform bone and the second metatarsal bone (white arrow), and the Lisfranc ligament (black arrow) were all visible. C: Measurement of included angle of the Lisfranc ligament between the medial cuneiform and the second metatarsal. D: The starting point of Lisfranc ligament on the medial cuneiform bone.
The Vernier caliper made in China was used to measure the length and width of the ligament, and the distance from its origin at articular surface to the edge, with the accuracy of 0.02 mm. Vernier caliper has also been reported in another research, which is with a high accuracy [8]. The protractor made in China was used to measure the included angle, with the accuracy of 1.0º. All specimens were measured by the same person with the same set of instruments, and were repeated three times to take the average value.
Statistical methods
SPSS version 14.0 statistical software (International Business Machines Corporation, NY, USA) was applied. The data were presented as mean ±standard deviation.
Results
The length and width of dorsal ligament between the medial cuneiform bone and the base of the second metatarsal bone was 5.44 ± 0.83 mm and 4.20 ± 0.64 mm, respectively. The plantar ligament of 16/20 specimens was divided into two bundles, which ended at the base of the second and third metatarsals, respectively. The fourth foot plantar ligament ended at the base of the second metatarsal. All structures measured in this research were about the ligaments from the medial cuneiform to the second metatarsal. The length and width of Lisfranc ligament was 9.33 ± 1.34 mm and 8.00 ± 1.23 mm, respectively. The included angle between Lisfranc ligament and the proximal end of medial shaft of the second metatarsal bone was 61.45 ± 5.03°. The origin of Lisfranc ligament was 10.89 ± 0.84 mm away from the dorsal part of the first cuneiform, 8.31 ± 0.92 mm away from its plantar side, 5.35 ± 0.60 mm away from its distal end, and 12.04 ± 0.85 mm away from its proximal end. We conclude that among the three ligaments between the medial cuneiform bone and the base of the second metatarsal, the Lisfranc ligament is the largest, followed by plantar ligament and then the dorsal ligament. The origin of the Lisfranc ligament at the lateral of the medial cuneiform bone is near the distal metatarsal side, namely the anterior-inferior part of entire joint surface (Table 1).
| Items | ͞x ± s (min-max) mm/° |
|---|---|
| The length of dorsal ligament | 5.44 ± 0.83 (4.22-6.88) |
| The width of dorsal ligament | 4.20 ± 0.64 (3.18-5.36) |
| The length of plantar ligament | 7.07 ± 1.05 (4.96-8.82) |
| The width of plantar ligament | 5.23 ± 1.10 (3.28-7.66) |
| The length of Lisfranc ligament | 9.33 ± 1.34 (6.96-11.26) |
| The width of Lisfranc ligament | 8.00 ± 1.23 (5.90-11.14) |
| The included angle between Lisfranc ligament and the shaft of the second metatarsal bone | 61.45 ± 5.03 (54-70) |
| The distance between the origin of Lisfranc ligament and the dorsal of the first cuneiform | 10.89 ± 0.84 (9.00-11.86) |
| The distance between the origin of Lisfranc ligament and the plantar of the first cuneiform | 8.31 ± 0.92 (6.36-10.22) |
| The distance between the origin of Lisfranc ligament and the distal of the first cuneiform | 5.35 ± 0.60 (4.32-6.22) |
| The distance between the origin of Lisfranc ligament and the proximal of the first cuneiform | 12.04 ± 0.85 (10.52-13.20) |
Table 1. Measurements of anatomic index of the ligaments between the first cuneiform and the basement of the second metatarsal bone.
Discussion
According to different anatomical characteristics and functions, the tarsometatarsal joint can be divided into three parts: the middle, medial and lateral columns. The medial column consists of the first tarsometatarsal joint, the middle column of the second and third arsometatarsal joints, and lateral column of the fourth and fifth tarsometatarsal joints. The medial and the middle columns play a major role in maintaining the stability of the foot.
Clinical significance of the ligaments between cuneiform and the base of the second metatarsal
There are three ligaments between cuneiform and the base of the second metatarsal, including dorsal, interosseous (Lisfranc) and plantar ligaments. A series of biomechanical characteristics of Lisfran and dorsal ligaments were tested by Kura et al. [9]. The stiffness coefficient of Lisfranc ligament is about three times that of the dorsal ligament, and the load is two times that of the latter. After Kaar et al. cut off the Lisfranc ligament [10], and the ligament between the medial and the intermediate cuneiform bones, causing the instability of the Lisfranc joint in a transverse direction. It is indicated that the Lisfranc ligament plays an important role in maintaining the stability of the second metatarsal base and the entire Lisfranc joint. Because of the special position of Lisfranc ligament, it cannot be repaired by suture after injury, and can only heal itself by scar repair, which requires the perfect realignment of the joint surface [11]. Besides the Lisfranc ligament, the plantar ligament which connects the medial cuneiform bone and the second/third metatarsal base is the strongest and the most important one among other numerous plantar ligaments. This ligament originates from the lateral border of the medial cuneiform bone, which is then divided into two bundles traveling obliquely to the lateral side. The thin and deep one ends at the base of second metatarsal, and the thick and superficial one ends at the base of the third metatarsal. These two bundles cross the articular surface in a bowstring shape at the plantar side to maintain the stability of the medial and intermediate columns. Damage of the ligament is likely to cause the avulsion fracture of the bases of the second and third metatarsals [10]. Therefore, it is of clinical significance to investigate the anatomy of the ligaments between the medial cuneiform and the base of the second metatarsal.
Anatomical characteristics of the ligaments between medial cuneiform bone and the second metatarsal and the comparison between them
We found that the dorsal ligaments originated from the dorsal lateral side of the medial cuneiform bone and ended at the dorsal medial side of the second metatarsal. It was rectangular and flat. The plantar ligaments originated from the lateral metatarsal side of the medial cuneiform bone. The sixteen feet ligaments split into two bundles, ending at the bases of the second and third metatarsals, as previously reported [12]; four had variation, and only one bundle ended at the base of the second metatarsal. The Lisfranc ligament originated from the lateral of medial cuneiform and ended near the articular surface of the base of the second metatarsal ligament. It was thick and approximately ellipsoidal. Studies rarely report anatomic measurement of these three ligaments. Johnson et al. measured the width, thickness, cross-sectional etc., of the metatarsal, dorsal and Lisfranc ligaments. They found that Lisfranc ligament was the largest, and followed by plantar and dorsal ligaments [8]. These results are consistent with those of the biomechanical tests, showing that the dorsal ligament is weaker than the plantar ligament. Therefore, the dorsal ligament is broken earlier than the plantar ligament under the external force. Thus, in clinical settings, when Lisfranc is injured, dislocation of the dorsal side is more common than that of the plantar side. The data of these ligaments obtained by us are consistent with the conclusion by Johnson et al.; thus they could improve the understanding of the anatomic characteristics of ligaments at the joint and provide reference for clinical treatment. Because the direction of dorsal and plantar ligament was almost transversal, and the direction of Lisfranc ligament was diagonal, Lisfranc ligament was found to be the longest in this study. Jognson et al. has measured the width, thickness, and transversal area of these three ligaments, and found that Lisfranc ligament was the longest [8]. So far, there was no report about the length of Lisfranc ligament.
Meanwhile, we have also mentioned that the shorter branch of plantar ligament was used for measurement in this study. All structures measured in this research were about the ligaments from the medial cuneiform to the second metatarsal. Thus, Lisfranc ligament was the longest.
Clinical significance of measuring the starting position and direction of the Lisfranc ligament
No domestic and foreign studies have reported the origin of the Lisfranc ligament at the medial cuneiform bone and its orientation. However, with the development of treatment for Lisfranc injury, the anatomical data of this part have become more and more important.
Most surgical treatments of injury to Lisfranc joint adopt open reduction and internal fixation, for which available tools include Kirschner's pins, screws, plate, staple, suture buttons and others, each with their advantage and disadvantage. The internal fixation should be chosen appropriately based on the location and extent of Lisfranc damage. If the Lisfranc ligament has been damaged and the gap between medial cuneiform bone and the second metatarsal base has been widened, a “Lisfranc screw” should be placed along the conventional direction of the Lisfranc ligament, generally from the medial of the medial cuneiform bone obliquely to the second metatarsal base. Lisfranc screw, a kind of position screw, cannot exert pressure, but is important for maintaining position between the medial cuneiform bone and the second metatarsal base and for repairing Lisfranc ligament. As no anatomical data are available to help selecting the site for the placement of the screw, if it is blindly implanted, the starting point of the Lisfranc ligament will be damaged, affecting the repair effect. Based on our experimental data, the origin of the Lisfranc ligament at the medial side of the cuneiform bone was near the distal plantar side, which was the anterior-inferior part of the entire joint surface. When the Lisfranc screws are inserted in operation, this location should be avoided so as to avoid damage to the starting point of the ligament.
In recent years, the endo-button, which can provide a kind of non-rigid anatomical reduction and is more consistent with the physiological characteristics of the Lisfranc ligament, has been applied in treating Lisfranc injury. Panchbhavi et al. [13] compared the biomechanical strength between the suture button and the hollow nail, finding that they have equivalent fixation strength, the fracture of the screws will not occur, and the 2nd operation is not required to remove the screws. Suture button is often used for the fixation between the medial cuneiform bone and the second metatarsal base after Lisfranc ligament damage, and can be used to replace the Lisfranc screw. Brin et al. [14] reported the significant short-term therapeutic effect of treating Lisfranc ligament damage with suture button in five patients, and the AOFAS scores of four patients were significantly improved. A satisfactory effect was obtained by using the suture button in the cases that need revision surgery after the failure of the screw fixation [15]. In this experiment, we measured the direction of Lisfranc ligament. Its included angle with the proximal of the axis of the second metatarsal base was 61.45 ± 5.03°. The suture button can be placed based on this angle in surgery, to make its direction consistent with the physiological angle of the Lisfranc ligament, so as to obtain satisfactory effect.
In conclusion, the Lisfranc ligament is the largest one in the Lisfranc complex, plantar ligament is the second largest and the dorsal ligament is the smallest. The internal fixation for the treatment of Lisfranc injury can be performed based on the location of the origin of Lisfranc ligament and the included angle between the ligament and the shaft of the second metatarsal bone. Further studies should be focused on biomechanical analyses about endo-button used in fixation for Lisfranc ligament injures.
Limitations
Due to the lack of cadaver specimens, this study had only a few specimens of both women and men. Thus, it is inevitable to have differences in body/foot size in terms of the size of the ligaments. However, results may not be generalized as this it is only a one-center study.
References
- Seybold JD, Coetzee JC. Lisfranc Injuries: When to observe, fix, or fuse. Clin Sports Med 2015; 34: 705-723.
- Perron AD, Brady WJ, Keats TE. Orthopedic pitfalls in the ED: Lisfranc fracture-dislocation. Am J Emerg Med 2001; 19: 71-75.
- Hatem SF. Imaging of lisfranc injury and midfoot sprain. Radiol Clin North Am 2008; 46: 1045-1060, vi.
- Panchbhavi VK, Molina D, Villarreal J, Curry MC, Andersen CR. Three-dimensional, digital, and gross anatomy of the Lisfranc ligament. Foot Ankle Int 2013; 34: 876-880.
- Ryba D, Ibrahim N, Choi J, Vardaxis V. Evaluation of dorsal Lisfranc ligament deformation with load using ultrasound imaging. Foot (Edinb) 2016; 26: 30-35.
- Rettedal DD, Graves NC, Marshall JJ, Frush K, Vardaxis V. Reliability of ultrasound imaging in the assessment of the dorsal Lisfranc ligament. J Foot Ankle Res 2013; 6: 7.
- Marshall JJ, Graves NC, Rettedal DD, Frush K, Vardaxis V. Ultrasound assessment of bilateral symmetry in dorsal Lisfranc ligament. J Foot Ankle Surg 2013; 52: 319-323.
- Johnson A, Hill K, Ward J, Ficke J. Anatomy of the lisfranc ligament. Foot Ankle Spec 2008; 1: 19-23.
- Kura H, Luo ZP, Kitaoka HB, Smutz WP, An KN. Mechanical behavior of the Lisfranc and dorsal cuneometatarsal ligaments: in vitro biomechanical study. J Orthop Trauma 2001; 15: 107-110.
- Kaar S, Femino J, Morag Y. Lisfranc joint displacement following sequential ligament sectioning. J Bone Joint Surg Am 2007; 89: 2225-2232.
- Yuen JS, Yung SW, Wong MK. Open reduction and temporary rigid internal fixation of Lisfranc fracture-dislocations. Singapore Med J 2001; 42: 255-258.
- Crim J. MR imaging evaluation of subtle Lisfranc injuries: the midfoot sprain. Magn Reson Imaging Clin N Am 2008; 16: 19-27.
- Panchbhavi VK, Vallurupalli S, Yang J, Andersen CR. Screw fixation compared with suture-button fixation of isolated Lisfranc ligament injuries. J Bone Joint Surg Am 2009; 91: 1143-1148.
- Brin YS, Nyska M, Kish B. Lisfranc injury repair with the TightRope device: a short-term case series. Foot Ankle Int 2010; 31: 624-627.
- Lundeen G, Sara S. Technique tip: the use of a washer and suture endobutton in revision lisfranc fixation. Foot Ankle Int 2009; 30: 713-715.