Review Article - Journal of Advanced Surgical Research (2017) Volume 1, Issue 1
A review of periosteal pedicle graft technique for the management of Gingival recession defects.
Ajay Mahajan*
Department of Periodontology, HPGDC Shimla, Himachal Pradesh, India
- *Corresponding Author:
- Ajay Mahajan
Department of Periodontology
HPGDC Shimla Himachal Pradesh, India
Tel: +919418017029
E-mail: drajdent@yahoo.in
Accepted date: February 21, 2018
Citation: Mahajan A. A review of periosteal pedicle graft technique for the management of gingival recession defects. Adv Surg Res. 2018;2(1):10-14
Abstract
Now a day’s gingival recession has become a very common finding along with inadequate vestibular depth. Gingival recession may be a concern for patients for a number of reasons such as root hypersensitivity, erosion, root caries and esthetics many techniques have been utilized in order to treat such defects and obtain predictable root coverage. Several graft procedures are used to obtain the coverage however, a graft having its own vascularity that can be extricated from the adjoining defect site in ample amounts with a capacity to regenerate is ideal. Since, the periosteal pedical graft satisfies the all requirements of an ideal graft material like own blood supply, its regenerative potential, ample amount of availability, single surgical site, also when compared to other graft materials its properties have proved to be superior, recently its use as a graft has shown better results when used for the management of gingival recession defects. The present review article is undertaken to evaluate the use of Periosteal Pedicle Graft (PPG) and its success over the past one decade for treating gingival recession defects.
Keywords
Gingival recession, periosteal pedicle graft, management, periosteum, review
Introduction
Management of Gingival Recession Defects (GRD) has always been an area of concern for dental surgeons. If left untreated, it will result in loss of supporting structure and aloveolar bone which ultimately leads to tooth loss [1]. The fact that gingival recession results in functional as well as aesthetic problems for the patient, various treatment modalities have been suggested to treat the same since long sub-epithelial connective tissue graft, GTR, auto-genus grafts etc. [2-4]. Despite availability of various surgical options to treat GRD there are inherent limitations of the traditional techniques which limit their utility. PPG is a relatively recent technique which has shown remarkable results [3]. The aim of the current article is to review in depth the origin and current status of periosteal pedicle graft.
Search strategy
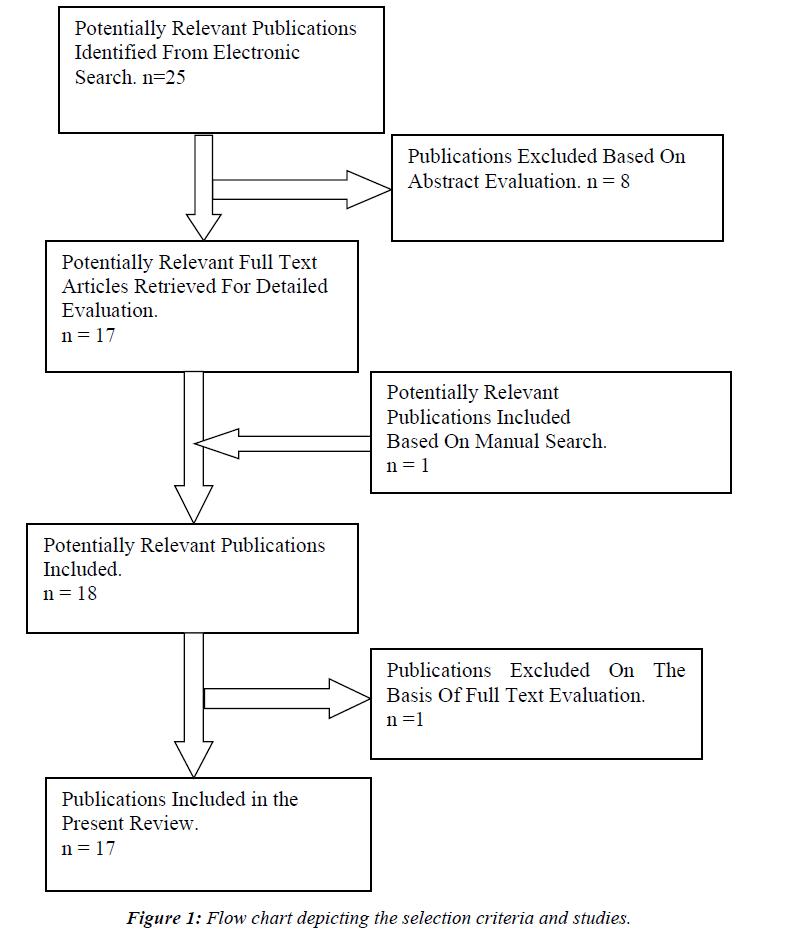
A search of the electronic database of PUBMED, up to and including 2017 was made. Studies included were randomized control trials, case series, case reports, review articles and systematic reviews the flow chart depicting the selection criteria and studies (Figure 1).
Inclusion criteria
Studies which compared the effectiveness of periosteal grafts (free or pedicle, tissue engineered periosteal membrane or cultured periosteal cells) in the management of gingival recession. Randomized controlled trials, clinical trials, case reports, case series and systematic reviews and Human studies.
Exclusion criteria
Studies not in English language and Studies where outcome parameters are not clearly mentioned and Studies on gingival recession included 5 case reports, 1 case series and 6 RCT, 3 review articles and 2 systematic reviews.
Gingival recession definition and consequences
Gingival recession is apical migration of the gingival margin to the Cemento Enamel Junction (CEJ) resulting in exposure of the root surface. It can be localized or generalized and can be related to one or more tooth surfaces [5]. According to Naber 1954, “adequate” zone of gingiva was considered critical for the maintenance of marginal tissue health as it prevents subgingival plaque formation and clinical attachment loss [6] gingival recession causes many problems such as impaired esthetics, plaque accumulation and subsequent gingivitis and root caries or dentin hypersensitivity [7]. The gingival recession has a multifactorial etiology ranging from clinical attachment loss due to plaque accumulation to factors like tooth malpositions, aberrant frenum and iatrogenic factors [8,9].
What are the treatment modalities?
The treatment of GRD is based on detailed evaluation of the defects and elimination of causative factors [8]. The treatment modalities for root coverage mainly include but are not limited to surgical techniques utilizing pedicle flaps, sub-epithelial connective tissue graft and GTR membrane [9,10] the two different types of surgical procedures are.
Pedicle soft tissue graft procedures
Type of graft attached to their base with active blood supply such procedure include either rotational flap procedures (laterally positioned flap, double papilla flap) or advancement procedures (carnally advanced flap).
Free soft tissue graft procedures
Require a donor site and a recipient site free gingival graft and sub-epithelial connective tissue graft [8].
Several factors are responsible for selection of the surgical techniques, which include the defect site anatomy, recession defect size, availability of keratinized tissue adjacent to defect, interdental soft tissue height and width and depth of the vestibule [11,12]. Although there are numerous available procedures to achieve root coverage, a vascular graft available adjacent to the recession site in sufficient amount is the need of the hour [13]. Recently periosteum has been used for the treatment of gingival recession defects and has revealed promising results over other techniques. One of the recent technique involves the use of periosteum as a pedicle to cover the exposed root surface area [14]. Almost 10 year have passed since the PPG was first proposed for the treatment of gingival recession [15]. Reasons for using periosteum as a graft in root coverage procedures were
• Periosteum is a rich source of pluripotent stem cells, retain their ability to regenerate.
• Rich vascularity of periosteum
• Ability of periosteum to release vascular endothelial growth factors
Why use Periosteum as graft?
The periosteum is a highly vascular connective tissue sheath which covers the outer surface of all the bones except articulation and muscle attachment sites [16]. There are two layers of periosteum, an inner cambium layer, and the outer fibrous layer. The osteoblasts and osteon-progenitor cells are present on the inner layer and dense collagen fibers, fibroblasts, and their progenitor cells on the outer layer [16]. The utilization of periosteum as a graft in dentistry is not novel. To explain osteogenic potential of human periosteal grafts a variety of research papers are available [8-17]. A study has shown that periosteal cells release vascular endothelial growth factor and promote neovascularization [18]. Periosteum, the “Sleeping Giant” leaps into action by surgical trauma and offers“ a river of regenerative tissue” which favours collagen formation and osteogenesis. It also acts as a catalyst for nerve regeneration for gingiva, mucosa and graft that lies above it [18]. Periosteum as a GTR has been recommended by many studies, although conclusive evidences regarding the ability of periosteum as a barrier membrane are lacking [17]. Based upon the properties of periosteum its use as a graft for GRD treatment was justified [19].
The journey of periosteal pedicel graft in treatment of GRD
Healing of wound after a gingival surgery depends upon ability to form clot, revascularization, and preservation of blood supply. Probably a vascular graft survive more on an vascular root face .Such qualities make periosteum an appropriate graft over an avascular root area. In addition, necrosis is prevented by having a rich blood supply even if it is left exposed by the flap which lies over it, particularly if gingival recession is present over a large area [18]. Lekovic et al. treated 28 furcation defects 14 treated with a periosteal barrier and 14 treated with a coronally positioned flap. They carried out follow up surgery at 6 months .They found that group utilizing periosteum had more significant bone formation [19,20]. In a similar study done by Gaggl et al. it was found that after doing periodontal flap surgery on 15 patients with recession defects of periodontium the periostium covered the periodontal recession defects and resulted in gain in clinical attachment level and regeneration of the defects with improved esthetics [21]. Mahajan in 2009 did a study where he used periosteal pedicle graft to treat recession defects of gingiva. He treated four patients with Miller Class I and II recessions with PPG. After one year, all defects were successfully recovered [13] in another study Mahajan A in 2010 treated multiple gingival recession defects with PPG. He examined twenty teeth in 6 patients of recession defects (Miller Class I and II) with PPG. He measured the depth of probe inside gingiva, attached gingival width and depth of recession defect. With the use of the paired test he found that after a year, there was successful root coverage with a considerable increase in width of attached gingiva however there was no variation in probing depths. He concluded successful results in gingival recession defects treated with PPG technique [22]. Mahajan et al. in 2012 done a randomized control trial and compared PPG with SCTG to treat defects of gingival recession and found comparable clinical efficacy of PPG and SCTG , but PPG had superior outcomes to SCTG in terms of patient’s compliance, reflecting improved patient comfort and overall patient satisfaction [14]. Hofmänner et al. performed a systemic review to predict various techniques used to cover gingival recession involving multiple teeth and he found that when CTG used with CAF, MCAF it offered more successful results compared to CTG when used alone [23]. Harshvardhana et al. did the same study on multiple gingival recession and found successful results when treated using periosteal pedicle graft [24]. Gupta et al. did a case series which included three males and two females to assess the usefulness of the PPG as a root coverage procedure and concluded that edema and related morbidity as a constant and expected complication of PPG when used in the maxillary canine/premolar area [25]. Chatterjee et al. studied multiple gingival recessions with vista technique and reported excellent results as periosteal pedical graft [26]. Kumar et al. used a modification of PPG for extension of vestibule. He used reflected periosteal layer after fenestration as graft to cover root and the results were enhanced depth of vestibule with successful coverage of root defect [18]. Mahajan and Assin reviewed current literature to assess the efficacy of Periosteal pedicle graft technique and came to a conclusion that Periosteal Pedicle Graft has good clinical outcomes in treating GRD patients [15]. In a study published in IJPRD by Godavarthi et al. in which clinical efficacy of PPG and a cellular dermal matrix allograft with carnally advanced flap to treat recession defects was compared. After a year they found that compared to the use of ADMA, the PPG technique uses similar incision design and flap management at the graft site, equal in technique sensitivity, and improved esthetic outcomes [27]. Singh and Gautam evaluated the PPG (PRF induced) with VISTA technique to cover denuded root surface area. A patient with Miller Class II gingival recession of 6.5 mm was treated by PRF reinforced with VISTA technique. PRF was prepared from whole blood and applied to the root surface. After 6 months, 5.5 mm, that is, 84.6% root coverage attained .They concluded PRF reinforced PPG with VISTA technique had successful results in the treatment of gingival defects [28]. Dandu and Murthy done a study to compare the vestibular incision subperiosteal tunnel access (VISTA) technique by means of Geistlich membrane improved with Osteohealth to PPG with coronally advanced flap and concluded that both VISTA and PPG techniques provided better root coverage also VISTA technique being less invasive require negligible time and had superior esthetic outcomes [29]. Yasaswini, et al. performed a study to compare clinically and radio graphically the regenerative potential of marginal periosteal pedicle graft (MPPG) or platelet rich fibrin (PRF) with a bioactive glass in the treatment of two and three wall intrabony defects. Results showed that in both experimental groups there was clinically and considerable reduction in mean PI, SBI, PD, radiographic defect depth, and improvement in CAL. At six months the defect fill was (70.55 ± 15.99 vs. 55.30 ± 11.87) and 9 months (84.55 ± 11.74 vs. 72.2 ± 9.91) was significantly greater in Site A compared to Site B [30]. Mahajan and Assi have recently done a study to compare periosteal Pedicle Graft with coronally advanced flap for the treatment of Multiple gingival Recession and concluded that periosteal pedical graft has better results than to coronally advanced flap [31].
Limitations and future prospective
Over a decade multiple studies have been done and several techniques have emerged to attain predictable root coverage [14]. Studies till date have shown that PPG produces good results in terms of root coverage and patient centered criteria [22-27]. The reason for success of periosteal pedical graft can be attributed [14].
• Its own blood supply
• Potential for promoting regeneration
• Ample amount of availability
• Single surgical site
• Better patient comfort
• Cost effective
The results of our review show that there are minimal side effects associated with periosteum pedical graft. Among all the studies included in this review there is just one case report that mention ecchymosis as possible side effect of PPG, none of the other studies have shown any complications. The possible mechanism for success of PPG needs further investigation in terms of histopathological analysis. Histopathological studies will not only reveal the type of healing taking place at the PPG grafted site but will also be useful to analyze the regenerative potential of the periosteum. Thus, quality interventional studies with a larger sample size and longer observation periods are needed to examine the patient to compare the effectiveness of PPG technique in relation to other techniques for the treatment of gingival recessions. In Future, studies with extended followups and histological data regarding the healing of PPG are suggested to assess the healing pattern of periosteal pedical graft.
Conflict of Interest
The authors declares no conflict of interest
References
- Pradeep K, Rajababu P, Satyanarayana D, et al. Gingival recession: review and strategies in treatment of recession. Case Rep Dent.2012.
- Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol.2015;86:8-51.
- Francetti L, Weinstein R, Taschieri S, et al. Coronal Advanced Flap With or Without Sub epithelial Connective Tissue Graft for the Treatment of Single Recession: 5-Year Outcomes from a Comparative Study. Int J Periodontics Restorative Dent.2018;1:16.
- Langer B, Langer L. Sub epithelial Connective Tissue Graft Technique for Root Coverage J Periodontol.1985;56:715-20.
- Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc.2003;134:220-5.
- Jan L, Wennstrom G, Giovan P. “Mucogingival therapy-Periodontal plastic surgery”Jan Lindhe 5th edition.2003;9:95-6.
- Mahajan A, Assin KS. Periosteal pedicle graft for the treatment of gingival recession defects current status and future prospects: What the evidence suggests. J Indian Soc Periodontol.2016;10:20-2.
- Alghamdi H, Babay N. Surgical management of gingival recession a clinical update. Saudi Dent J.2009;21:83-94.
- Tugnait A, ClerehughV. Gingival recession-its significance and management, J Dent.2001;29:381-94.
- Wennstrom JL. Mucogingival therapy Ann. Periodontol.1996;1:671-701.
- Zucchelli G, Testori T, DeSanctis M. Clinical and anatomical factors limiting treatment outcomes of gingival recession a new method to predetermine the line of root coverage. J Periodontol.2006;77:714-21.
- Haghighati F, Mousavi M, Moslemi N, et al. comparative study of two root-coverage techniques with regard to interdental papilla dimension as a prognostic factor. Int. J. Periodont. Rest. Dent.2009;29:179-89.
- Mahajan A. Periosteal pedicle graft for the treatment of gingival recession defects a novel technique. Aust Dent J.2009;54:250-4.
- Mahajan A, Bharadwaj A, Mahajan P. Comparison of periosteal pedicle graft and sub-epithelial connective tissue graft for the treatment of gingival recession defects. Aust Dent J.2012;57:51-7.
- Mahajan A, Assin KS. Periosteal pedicle graft for the treatment of gingival recession defects current status and future prospects: What the evidence suggests J Indian Soc Periodontol.2016;21:220-1.
- Lin Z, Fateh A, Salem DM. eriosteum Biology and Applications in Craniofacial Bone Regeneration. J Dent Res.2014;93:109-116.
- Mahajan A. Periosteum, A Highly Underrated Tool in Dentistry:Int J Dent.2012.
- Kumar S, Gupta KK, Agarwal R, et al. Periosteal Pedicle Flap Harvested during Vestibular Extension for Root Coverage. Case Rep Dent.2015.
- Shah MP, Patel AP, Shah KM. Periosteal pedicle graft a novel root coverage.2015; 19:99-102.
- Lekovic V, Kenney EB, Carranza FA, et al. The use of auto-genus periosteal grafts as barriers for the treatment of Class II furcation involvements in lower molars. J Periodontol.1991;62:775-80.
- Gaggl A, Jamnig D, Triaca A, et al. A new technique of periosteoplasty for covering recessions Preliminary report and first clinical results PERIO.2005;2:55-62.
- Mahajan A. Treatment of Multiple Gingival Recession Defects Using Periosteal Pedicle Graft A Case Series. J Periodontol.2010;81:1426-31.
- Hofmanner P, Alessandri R, Laugisch O, et al. Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions-a systematic review. Qintessence int.2012;43:545-54.
- Harshavardhana B, Rath SK, Mukherjee M. Periosteal pedicle graft - A new modality for coverage of multiple gingival recession defects. Indian J Dent Adv.2013;5:1139-42.
- Gupta GK, Kulkarni MR, Thomas BS. Post-operative morbidity following the use of the inverted periosteal graft: A case series. J Indian Soc Periodontol.2014;18:82-4.
- Chatterjee A, Shar/ma E, Gundanavar G, et al. Treatment of multiple gingival recessions with vista technique A case series. J Indian Soc Periodontol.2015;19:232-5.
- Godavarthi L, Murthy KR, Pavankumar S. A Comparison of A cellular Dermal Matrix Allograft and Periosteal Pedicle Graft Covered by coronal Advanced Flap in the Treatment of Gingival Recession 1-Year Follow-Up Study. Int J Periodontics Restorative Dent.2016;36:67-75.
- Singh AK, Gautam A. Platelet-rich fibrin-reinforced periosteal pedicle graft with vestibular incision sub-periosteal tunnel access technique for the coverage of exposed root surface. J Interdiscip Dentistry 2016;6:33-8.
- Dandu SR, Murthy KRV. Multiple Gingival Recession Defects Treated with coronal Advanced flap and either the VISTA technique enhanced with GEM21S or Periosteal Pedicle Graft a 9 month Clinical Study. Int J Perioodntics Restorative Dent.2016; 36:231-7.
- Yasaswini MS, Rao KV, Tanuja P, et al. Comparison of Marginal Periosteal Pedicle Graft and Bioactive Glass with Platelet-rich Fibrin and Bioactive Glass in the Treatment of Intrabony Defects A Clinic-radiographic Study. J Pharm Bioallied Sci. 2017;9:96-102.
- Rajpal J, Gupta KK, Srivastava R, et al. Vestibular deepening by periosteal fenestration and its use as a periosteal pedicle flap for root coverage. Journal of Indian Society of Periodontology.2013;17:265-70.