Research Article - Biomedical Research (2017) Volume 28, Issue 12
A prospective, randomised trial comparing transurethral enucleation with bipolar system (TUEB) to monopolar resectoscope enucleation of the prostate for symptomatic benign prostatic hyperplasia
Zhenlong Wang#, Hecheng Li# and Tie Chong*
Department of Urology, Second Affiliated Hospital, School of Medicine, Xi'an Jiaotong University, Xi’an, PR China
#These authors contributed equally to this work
- *Corresponding Author:
- Tie Chong
Department of Urology
Second Affiliated Hospital
School of Medicine
Xi'an Jiaotong University, PR China
Accepted date: April 27, 2017
Abstract
Objective: To compare the clinical outcomes between Transurethral Enucleation with Bipolar system (TUEB) and monopolar resectoscope enucleation of the prostate (mTUEP) for treating Benign Prostatic Hyperplasia (BPH) in a prospective randomized trial with 12 months of follow-up.
Methods: The study randomized 114 consecutive patients with BPH into either a TUEB (n=59) or mTUEP (n=55) treatment group.
Results: Significant differences were seen in the resection weight per unit time (0.76 ± 0.14 vs. 0.82 ± 0.23 g/min, P=0.04) and blood glucose levels (6.20 ± 1.35 vs. 5.34 ± 1.32 mmol/L, P=0.00) perioperatively, favoring TUEB over mTUEP. Patients in the mTUEP group showed statistically significant increases in postoperative blood glucose compared with their preoperative baseline (5.63 ± 1.54 vs. 6.20 ± 1.35 mmol/L, P=0.04), but still within normal limits. There was no statistically significant difference in operative time, intraoperative blood loss, resection rate, or serum sodium and haemoglobin levels.
Conclusion: TUEB was shown to be a safe and highly effective technique for relief of Bladder Outlet Obstruction (BOO). The clinical efficacy of TUEB is sustainable for up to 1 year of follow-up. Our single-center results show that TUEB has the same efficacy as monopolar TUEP for the surgical treatment of symptomatic BPH, which is potentially associated with a low rate of complications and a high efficiency of enucleation.
Keywords
Transurethral enucleation of the prostate (TUEP), Benign prostate hyperplasia (BPH), Transurethral enucleation with bipolar system (TUEB).
Introduction
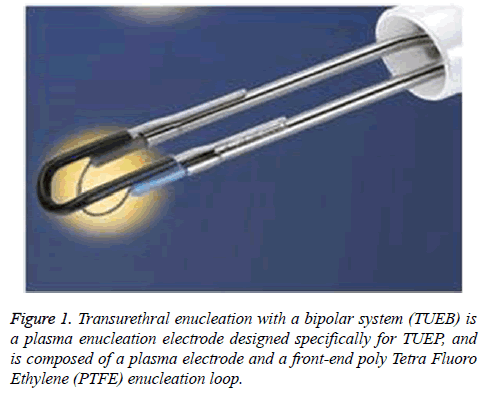
Transurethral Resection of the Prostate (TURP) is the gold standard treatment for Benign Prostate Hyperplasia (BPH) [1], but there are complications, such as residual hyperplastic tissue. Physicians that are developing new directions in transurethral prostatectomy have debated how best to resect the hyperplastic gland safely, efficiently, and completely. Transurethral Enucleation of the Prostatecan (TUEP) targets the same anatomical tissue as open surgery but results in less residual hyperplastic gland tissue compared with TURP. For this reason, TUEP has become an increasingly popular technology in transurethral prostate surgery [2]. At present, different transurethral prostate resection devices, such as resectoscopes [2], Holmiun lasers [3], Green lasers, and Thulium lasers [4] have been reported in the literature as effective in TUEP. In China, the monopolar resectoscope is still the most widely utilized technology in transurethral resection of the prostate, especially in less sophisticated hospitals and TUEP with monopolar resectoscope has been widely used. Transurethral enucleation with a bipolar system (TUEB) is a plasma enucleation electrode designed specifically for TUEP, which is composed of a plasma electrode and a front-end Poly Tetra Fluoro Ethylene (PTFE) enucleation loop (Figure 1). The efficacy and advantages of TUEB compared with the other enucleation devices are rarely reported in the literature. In order to examine the safety and efficacy of TUEB, we performed a prospective, randomized study of TUEB compared to mTUEP in patients with BPH in our department from January to October 2011.
Patients and Methods
Patients
From January to October 2011, men with moderate or severe lower urinary tract symptoms who were clinically diagnosed with BPH in our Department of Urology were invited to participate in the study. These men also agreed to endosurgical treatment.
Inclusion criteria were based on the patients’ 1) medical history, International Prostatic Symptom Score (IPSS), a Direct Rectal Examination (DRE), urinary flow rate detection and via abdominal ultrasound diagnosis. 2) The indications of surgery for BPH were compiled using the European Association of Urology (2009) guidelines [5]. 3) A pathological diagnosis of BPH was performed after surgery and 4) the performance of TUEP with TUEB electrodes and monopolar technology was evaluated.
Patients were excluded if they had 1) a combined neurogenic bladder dysfunction (including the BPH patients with a previous history of stroke) indicated by medical history and urodynamic examination, 2) urethral stenosis, 3) a diagnosis of prostate carcinoma in preoperative biopsy, 4) bladder tumors, 5) could not endure surgery because of some severe medical diseases, 6) the failure to attend follow-up visits or for whom information was lost.
Patients were randomized in a 1:1 ratio to undergo either TUEB (TUEB group) or monopolar TUEP (mTUEP group) from January to October 2011. There were 59 patients in the TUEB group and 55 patients in the mTUEP group (3 patients were excluded because of urethral stenosis detected during the operation). The age of all of the patients ranged from 56 to 89 y, and the average age was 73.09 ± 7.04 y. There were 7 patients with coronary disease or arrhythmia, 1 patient with coronary stent, 2 patients with cerebral infarction and one patient with renal insufficiency. All of the 114 patients participated in the one and 12 month follow-up.
Surgical methods
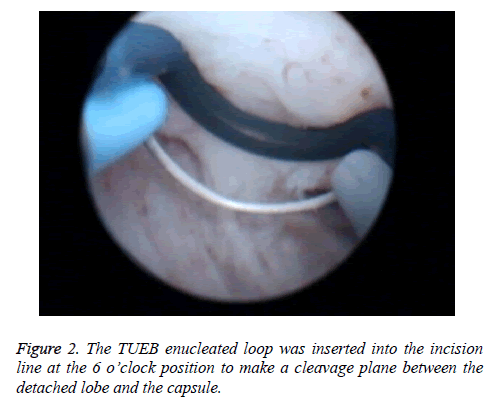
Each procedure was performed by two experienced surgeons (Chong Tie and HC Li) in our Department, who are skilled in TUEP and TURP. The patients were under epidural anaesthesia and placed in a lithotomy position. The TUEB procedure was performed using the Olympus Plasmasect enucleation electrode of the TUEB (Japan) and operated with a cutting power of 160 W and a coagulating power of 80 W. A 0.9% saline solution was used as the irrigation fluid in all of the cases. As the enucleation began, a "λ" shaped cut was made along the verumontanum with the TUEB cutting loop at the distal edge of the prostate lobes and the proximal edge of the external sphincter muscle. A circular incision on the urethral mucosa was made along the marks and extended into the surgical capsule until clear transverse fibres were observed. The TUEB enucleated loop was then inserted into the incision line at the 6 o’clock position to make a cleavage plane between the detached lobe and the capsule (Figure 2). The resectoscope sheath was moved into the cleavage plane just as the surgeon’s index finger did when performing open prostatectomy, and the detachment area was extended to the lateral, reserved 12 o' clock position so that the bladder neck was fixed for use. Meanwhile, the median and the lateral prostatic lobes were dissected away from the surgical capsule in a retrograde fashion from the prostate apex, towards the bladder. When bleeding on the established plane occurred, haemostasis was achieved with coagulation. Thus, the prostatic lobes were subtotally enucleated and devascularised but still connected to the bladder neck by a narrow pedicle. Finally, these devascularised lobes were fast-fragmented with the plasmakinetic cutting loop into pieces small enough to be evacuated through the resectoscope sheath.
Patients in the mTUEP group underwent TUEP using the olympus monopolar resectoscope (Japan) which was operated with a cutting power of 120 W and a coagulating power of 60 W. A 5% glucose solution was used as the irrigation fluid in all the cases and enucleated with the tip of a resectoscope sheath.
At the end of both procedures, a 22 F three-way Foley catheter was inserted into the bladder with a closed drainage system. All of the retrieved tissue was collected and examined histopathologically. Postoperative bladder irrigation with physiologic saline solution was applied as necessary until the efflux was sufficiently clear. The catheters were removed one to five days after the operation, and the patients were then discharged from the hospital one day later.
Collection of information
Before the operation, the International Prostate Symptom Score (IPSS), Quality of Life (QOL), maximum urinary flow rate (Qmax), Post-void Residual urine Volume (PRV), and the weight of the prostate and serum Prostate Specific Antigen (PSA) were recorded. The weight of the prostate was calculated based on Equation 1.
During the operation, the volume of the hemorrhage and the resection rate of the prostate were calculated based on Equations 2 and 3.
Weight of prostate=anteroposterior diameter (cm) × transverse diameters (cm) × axial diameters (cm) × 0.52 × 1.05 g/ml → (1)
Resection rate of prostate=(weight of resectional prostate × 1.2/weight of prostate) × 100% → (2)
Volume of haemorrhage=volume of irrigation fluid (L) × hemoglobin concentration of irrigation fluid (g/L) × 1000 (ml/L)/hemoglobin concentration (g/L) → (3)
Hemoglobin concentration, sodium concentration and blood glucose were measured before and immediately after surgery. The incidence of complications, such as transient urinary incontinence, and recovery time from these complications were recorded. IPSS, QOL, urinary flowing rate, residual urine (measured by ultrasound) and incidence of urethral stricture were measured or calculated for one month and one year after the operation.
Statistical analysis
SPSS16.0 software was used to analyse the data. Assuming a two-sided significance test with a significance level α=0.05 for the current study, with our sample size of 114 cases, the estimated power was 90%. Baseline characteristics and perioperative data between the two groups were compared by means of the independent-samples T test and Mann-Whitney test. Postoperative adverse events were compared by means of the two-tailed χ2 test. The Friedman test was used to compare preoperative and postoperative parameters within each group. Statistical significance was considered at p<0.05 for all analyses.
Results
From January to October 2011, 114 patients were enrolled in the study. All of the patients finished a one month follow-up. Forty-nine (83.1%) patients who underwent TUEB and 51 (92.7%) patients who underwent mTUEP finished the one year follow-up. The histologic finding indicated BPH in all cases. There was no statistically significant difference in any preoperative parameters between the two arms (Table 1).
| Parameters | All patients (n=114), mean ± SD (range) | TUEB group (n=59), mean ± SD (range) | mTUEP group (n=55), mean ± SD (range) | p value |
|---|---|---|---|---|
| Age (y) | 73.09 ± 7.04 | 72.22 ± 6.75 | 73.56 ± 7.18 | 0.24 |
| Serum PSA, mg/ml | 4.96 ± 3.88 | 5.06 ± 4.07 | 4.91 ± 3.80 | 0.81 |
| TRUS prostate volume, ml | 57.46 ± 17.79 | 55.75 ± 18.91 | 58.37 ± 17.19 | 0.36 |
| IPSS | 25.15 ± 5.26 | 25.97 ± 4.50 | 24.71 ± 5.59 | 0.14 |
| QoL | 4.73 ± 1.03 | 4.68 ± 0.99 | 4.76 ± 1.05 | 0.61 |
| Qmax, ml/s | 7.79 ± 2.64 | 7.93 ± 2.57 | 7.71 ± 2.69 | 0.61 |
| PVRU volume, ml | 88.63 ± 55.41 | 91.25 ± 57.55 | 87.21 ± 54.45 | 0.65 |
Table 1. Baseline characteristics of eligible patients.
Table 2 shows that significant differences favouring TUEB were seen perioperatively in the resection weight per unit time and blood glucose. Also, patients in the mTUEP group showed statistically significant increases in postoperative blood glucose compared with their preoperative baseline, but still within normal parameters. There was no statistically significant difference in operative time, intraoperative blood loss, resection rate, serum sodium and haemoglobin between the two patient groups.
| Parameters | TUEB group (n=59), mean ± SD (range) | mTUEP group (n=55), mean ± SD (range) | p value |
|---|---|---|---|
| Operative time, min | 46.76 ± 16.16 | 52.09 ± 19.27 | 0.72 |
| Resected tissue weight (g) | 37.42 ± 14.49 | 38.54 ± 12.76 | 0.61 |
| Intraoperative blood loss (ml) | 158.20 ± 57.71 | 171.02 ± 64.42 | 0.2 |
| Resection rat (%) | 66.68 ± 6.15 | 65.60 ± 6.80 | 0.31 |
| Resection weight per unit time (g/min) | 0.82 ± 0.23 | 0.76 ± 0.14 | 0.04 |
| Serum sodium (mmol/L) | |||
| Preoperative | 143.23 ± 4.90 | 142.85 ± 4.92 | 0.63 |
| Postoperative | 141.89 ± 4.87 | 141.11 ± 4.93 | 0.32 |
| p value | 0.14 | 0.07 | |
| Haemoglobin (g/dl) | |||
| Preoperative | 124.93 ± 15.43 | 127.35 ± 14.27 | 0.31 |
| Postoperative | 121.31 ± 15.91 | 123.15 ± 14.12 | 0.44 |
| p value | 0.21 | 0.13 | |
| Blood glucose (mmol/L) | |||
| Preoperative | 5.36 ± 1.48 | 5.63 ± 1.54 | 0.29 |
| Postoperative | 5.34 ± 1.32 | 6.20 ± 1.35 | 0 |
| p value | 0.93 | 0.04 |
Table 2. Perioperative characteristics of the patients in the two groups.
An analysis of treatment efficacy is detailed in Table 3. There were significant improvements in IPSS, QoL, Qmax, and PVRU by both modalities at each postoperative assessment compared with their preoperative baseline. However, no statistically significant disparities were identified in postoperative IPSS, QoL, Qmax, and PVRU between the two groups after one year (Table 3).
| Parameters | TUEB | mTUEP | p value | ||
|---|---|---|---|---|---|
| Patients, no. | Mean ± SD (range) | Patients, no. | Mean ± SD (range) | ||
| IPSS | |||||
| Preoperative | 59 | 25.97 ± 4.50 | 55 | 24.71 ± 5.59 | 0.14 |
| 1 mon | 59 | 7.80 ± 3.85* | 55 | 7.60 ± 2.65* | 0.72 |
| 1 y | 49 | 6.26 ± 2.62* | 51 | 5.96 ± 2.42* | 0.49 |
| QoL score | |||||
| Preoperative | 59 | 4.68 ± 0.99 | 55 | 4.76 ± 1.05 | 0.14 |
| 1 mon | 59 | 1.76 ± 0.82* | 55 | 2.00 ± 0.84* | 0.72 |
| 1 y | 49 | 1.60 ± 0.78* | 51 | 1.51 ± 0.64* | 0.49 |
| Qmax, ml/s | |||||
| Preoperative | 59 | 7.93 ± 2.57 | 55 | 7.71 ± 2.69 | 0.6 |
| 1 mon | 59 | 19.59 ± 3.41* | 55 | 20.33 ± 3.55* | 0.2 |
| 1 y | 49 | 21.54 ± 4.19* | 51 | 20.55 ± 3.52* | 0.13 |
| PVR, ml | |||||
| Preoperative | 59 | 91.25 ± 57.55 | 55 | 87.21 ± 54.45 | 0.65 |
| 1 mon | 59 | 20.58 ± 15.79* | 55 | 16.71 ± 17.43* | 0.16 |
| 1 y | 49 | 15.06 ± 11.88* | 51 | 13.27 ± 14.44* | 0.42 |
Table 3. Follow-up data stratified by treatment.
Patients in the TUEB group showed statistically significant improvements in postoperative transient incontinence compared to the patients in the TUEP group. Four patients (6.8%) in the TUEB group and seven patients (12.7%) in the mTUEP group who were diagnosed with transient incontinence without intrinsic sphincter deficiency by urodynamic evaluation, improved in 3.50 ± 1.29 and 7.71 ± 4.36 days, respectively (p<0.05). There was no transurethral resection of prostate syndrome (TURS) occurrence in the two treatment groups. In the study, one patient (1.7%) in the TUEB group and two patients (3.6%) in the mTUEP group developed urethral stricture. In these patients, dysuria eased after urethral dilation without internal urethrotomies and all of the patients improved after 2 months.
Discussion
TURP is the gold standard treatment for prostatectomy, but there are associated complications such as the presence of residual hyperplastic tissue and capsular perforation [6]. Within eight years after surgery, the incidence of further operation for the removal of residual gland is as high as 15.5~16.8% [7]. The question in the field of transurethral prostatectomy has been to determine how to resect a hyperplasic prostate gland safely, efficiently, and completely. TUEP has the same anatomical target as open surgery and residue little tissue after surgery compared with TURP, Shimizu performed TUEP on 64 BPH patients after giving them TURP, and found that the average removal rate of TURP was 54.5% [8]. At present, different transurethral prostate resection devices, such as the monopolar, bipolar plasmakinetic [2], Holmiun laser [9,10], green laser [11,12], and thulium laser [13] have been reported to effective and safe in enucleation. The enucleation electrode of the TUEB was composed of the plasma electrode and the front-end PTFE enucleation loop, which is designed particularly for prostate enucleation. The effect and advantages of TUEB, compared with other enucleation devices, are rarely reported in the literature. In this study, the gland resection rate showed a similar resection rate with monopolar TUEP.
One of the main advantages of TUEP is an improvement in symptoms of BPH. Postoperative IPSS, QoL, PVR and Qmax were significantly improved compared with the same values before surgery [2,3,14]. Over the course of 1month, 12 month follow-up, there were statistically significant differences in favour of TUEB with regard to improvements in postoperative IPSS, QoL score, Qmax, and PVR during. There were no statistical differences in these same values compared 1month with 12 month after surgery. TUEB is the proven durability of improved Lower Urinary-Tract Syndrome (LUTS), which is similar to TUEP. These indicate that TUEB and mTUEP can effectively improve the low urinary tract symptoms caused by BPH.
Several prospective randomized trials have demonstrated that TUEP could provide sufficient safety during operation. The factors affecting intraoperative safety are mainly hemorrhage and TURS. During the process of prostate enucleation, the tearing of subcapsular blood vessels is the chief reason for intraoperative hemorrhage. TUEB combines PTFE loop blunt dissection with plasma electrode coagulation, which was convenient the cessation of subcapsular hemorrhage. In our trail, there was no statistically significant difference in haemoglobin postoperation compared to pre-operation, similar to TUEP. The TURS occurs mainly because a great amount of flushing fluid is absorbed quickly because of capsular perforation, which causes the overload of the systemic circulation, and the imbalance of water and electrolyte. The TUEB electrode depends on the PTFE loop at the front of the electrode to get a blunt separation, and it was able to precisely control the location and depth of the separated gap, reducing the risk of capsular perforation. Our results showed that there is no capsular perforation in the two groups of patients. The serum sodium level showed no significant difference in TUEB postoperation compared with pre-operation. However, there were significant decreases in the TUEP group compared postoperative to pre-operative. But still within the normal range. None of the patients developed TURS. In the mTUEP group, blood glucose were significantly increased postoperatively but still within the normal range. These results demonstrated that TUEB and mTUEP were safe choices for patients. TUEB was more suitable for patients with heart disease or diabetes.
In the process of sheath enucleation, the main reasons affecting the efficiency of enucleation was bleeding caused by tearing of the subcapsular blood vessels and the presence of the fiber bands between capsules and the gland. TUEB enucleation electrodes combine a PTFE loop with a plasma electrode, so as to blunt dissect, cut fiber bands and coagulate almost at the same time. Meanwhile, there were statistically significant differences in favour of TUEB with regard to improvements in the efficiency of enucleation compared to the mTUEP treated group. Resection weight per min was signicantly more than that in the mTUEP group that demonstrated the superiority of operation efficiency in TUEB.
In our trail, we detected a lower rate of complications in the TUEB group, including urethral stricture and postoperative transient incontinence. In the study, one patient (1.7%) in the TUEB group and two patients (3.6%) in the mTUEP group developed prostatic urethra stricture, and dysuria eased after urethral dilation without internal urethrotomies. All of the patients improved over a 2 month period. The absence of a return current in the plasmakinetic system may reduce the risk of burns and urethral or bladder neck stricture. Monopolar current could be related to greater thermal damage [15].
Transient incontinence defined as any type of urine leakage, occurred after TUEP, in some patients, most of whom recovered within three months. In this study, there were statistically significant differences in favour of TUEB with regard to improvements in postoperative transient incontinence. The incidence rate and recovery time of provisional incontinence in patients treated with TUEB showed a significant decrease to the mTUEP group. One of the main advantages of the process of enucleation in TUEB was decreased urethral rhabdosphincter mechanical injury. The process of enucleation under monopolar sheath requires a great deal of force to push urethral rhabdosphincter, pry and separate the prostate gland from the surgical capsule. In the TUEB group, the angle of the PTFE loop and the plasma electrode is confined to local tension directed between the gland and the surgical capsule, not the sphincter. The force of the pressure on the external sphincter was lighter than monopolar sheath enucleation, reduced the possibility of sphincter mechanical damage and the incidence rate of postoperative provisionality incontinence. None of the patients developed permanent urinary incontinence.
TUEB was shown to be a safe and highly effective technique for relief of BOO. In our single-centre trail, TUEB has the same efficacy as TUEP, which is potentially associated with a low rate and recovery time of postoperative transient urinary incontinence.
References
- Yu XH, Elliott SP, Wilt TJ, McBean AM. Practice patterns in benign prostatic hyperplasia surgical therapy: The dramatic increase in minimally invasive technologies. J Urology 2008; 180: 241-245.
- Zhao ZG, Zeng GH, Zhong W, Mai ZL, Zeng SH, Tao XT. A prospective, randomised trial comparing plasmakinetic enucleation to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: three-year follow-up results. Eur Urol 2010; 58: 752-758.
- Ahyai SA, Lehrich K, Kuntz RM. Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol 2007; 52: 1456-1464.
- Herrmann TRW, Bach T, Imkamp F, Georgiou A, Burchardt M, Oelke M, Gross AJ. Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol 2010; 28: 45-51.
- Stohrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol 2009; 56: 81-88.
- Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol 2006; 50: 969-979.
- Shimizu Y, Hiraoka Y, Iwamoto K, Takahashi H, Abe H, Ogawa H. Is complete resection of hypertrophic adenoma of the prostate possible with TURP? J Nippon Med School 2005; 72: 146-148.
- Shimizu Y, Hiraoka Y, Iwamoto K, Takahashi H, Abe H. Measurement of residual adenoma after transurethral resection of the prostate by transurethral enucleation technique. Urol Int 2005; 74: 102-107.
- Yin L, Teng JF, Huang CJ, Zhang XM, Xu DF. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. J Endourol 2013; 27: 604-611.
- Krambeck AE, Handa SE, Lingeman JE. Experience with more than 1,000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urology 2013; 189: 141-145.
- Hermanns T, Batzill W, Hefermehl LJ, Gross O, Strebel DD, Talimi S, Krings T, Schwarz H, Seifert HH, Sulser T. 893 Photoselective lbo-green light laser vaporsation versus thulium laser vaporsesction of the prostate: a prospective bi-center comparson of peri-operative and early functional outcome. Eur Urol 2010; 9: 282.
- Kalchev I, Sancha F, Botsevski A, Kotsev J, Georgiev G. Green light laser vaporization and enucleation (GLEP) of the prostate-a 2 year series of 388 cases. Eur Urol 2011; 10: 581-582.
- Yang ZH, Wang XH, Liu TZ. Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up reply. Urology 2013; 81: 401.
- Gross AJ, Netsch C, Knipper S, Holzel J, Bach T. Complications and early postoperative outcome in 1080 patients after thulium vapoenucleation of the prostate: results at a single institution. Eur Urol 2013; 63: 859-867.
- Ko R, Tan AHH, Chew BH, Rowe PE, Razvi H. Comparison of the thermal and histopathological effects of bipolar and monopolar electrosurgical resection of the prostate in a canine model. Bju Int 2010; 105: 1314-1317.