Research Article - Biomedical Research (2017) Volume 28, Issue 12
A novel suture-traction method for right internal jugular vein catheterization in left-lateral position in anesthetized patients
Tianliang Wu1* and Huajie Zhao2
1Department of Anesthesia, First People's Hospital of Fuyang District, Hangzhou, PR China
2Department of Ultrasonic, First People's Hospital of Fuyang District, Hangzhou, PR China
- *Corresponding Author:
- Tianliang Wu
Department of Anesthesia
First People's Hospital of Fuyang District
Hangzhou, PR China
Accepted on May 8, 2017
Abstract
Right Internal Jugular Vein (RIJV) catheterization may be collapsed by the advancement of the needle and the pressure from ultrasonic probe, and the sutures are needed to fix the catheters after RIJV catheterization. This study aimed to develop a Suture-Traction Method (STM) to facilitate RIJV catheterization. 70 anesthetized patients underwent RIJV catheterization in Left-Lateral Position (LLP). In group T, the sutures were fixed by a skin-suturing needle and adopted to fix RIJV catheters after the puncture. In group N, only after puncture a position would be selected to fix RIJV catheters by the suture. The Cross-Sectional Area (CSA) and Anteroposterior Diameter (AD) of RIJV in Supine Position (SP) and in LLP were measured. Compared to CSA and AD in SP, CSA and AD at cricoid cartilage level were smaller in LLP during cannulation in Group N. Compared to CSA and AD before cannulation, CSA and AD at cricoid cartilage level were smaller in LLP during cannulation in Group N. Compared to CSA and AD in SP, CSA and AD at cricoid cartilage level was smaller in LLP during cannulation in Group T. We found no difference in LLP before and during cannulation in Group T. Compared to patients in group N, loss of resistance, easy aspiration of blood into syringe during needle insertion, first pass punctures and cannulations completed within 60 s increased significantly while catheterization time was shortened significantly in group T. In conclusion, STM facilitates the success of RIJV catheterization in LLP in anesthetized patients.
Keywords
Left-lateral position, Ultrasound, Internal jugular vein, Catheterization.
Introduction
Central venous catheterization is an important means of clinical infusion and monitoring, in which the Right Internal Jugular Vein (RIJV) catheterization is mainly employed [1,2]. Ultrasound-guided RIJV catheterization has the advantages of safety and high success rate [3]. However, RIJV may be collapsed by the advancement of the needle, the pressure from the ultrasonic probe and the muscle due to head rotation [4]. After RIJV catheterization, the sutures are generally used to fix the catheters to prevent them from being pulled out unintentionally [5].
In the clinical, RIJV catheterization in the Left-Lateral Position (LLP) is required for some patients under the following circumstances: First, for patients with severe right lateral chest emergency, surgeons perform chest operation from the right side in LLP to save time. Second, for patients with kyphosis RIJV catheterization is performed after general anesthesia. Therefore, it is important to establish a method for conductive RIJV catheterization in LLP.
Therefore, in this study we report the development of a novel Suture-Traction Method (STM), in which the puncture point of the skin right above the RIJV is fixed in original position by suture “traction” with the aim to facilitate catheterization of RIJV. STM not only maintains the vein size but also prevents the vein from collapsing during catheterization.
Patients and Methods
Patients
This study was approved by Institution Ethics Committee and all patients or their families signed consent. Seventy anesthetized patients were selected, who were required to perform RIJV catheterization, including 8 general chest surgery patients, 34 right hip fracture operation patients, 12 kyphosis patients and 16 urological operation patients. The patients’ ASA grade was I-III, age was 19-73 y old, weight was 48-82 Kg, and height was 160-183 cm. Exclusion criteria were external neck injury, previous RIJV catheterization, severe cardiovascular disease, injection-site infection, hematological disease, thrombosis history and obesity.
All patients were randomly divided into control group (group N) and suture-traction method group (group T). There were 35 patients in each group. An ultrasound surface probe (L25x/ 13-6 MHZ, SonoSite, Bothell, WA, USA) were used during catheterization and the same equipment was used on all subjects. All operations were performed by the same physicians.
Measurements
Before anesthesia induction, Heart Rate (HR), invasive Mean Arterial Pressure (MAP) and oxygen saturation were measured continuously. All patients were placed in the Supine Position (SP) with the head turned 30º to the left after anesthesia induction. The Cross-Sectional Area (CSA) and Anteroposterior Diameter (AD) of the RIJV at the cricoid cartilage level were measured in triplicate using electronic callipers. Afterward, the patients were changed to LLP with a small pillow under the head and a bolster under the upper left chest. CSA and AD of the RIJV in LLP were measured in triplicate. The anatomical position of RIJV, Internal Carotid Artery (ICA) and trachea could be seen from the top to the bottom. In group T, the ultrasonic probe should be perpendicular to the skin without any pressure after disinfecting the right neck skin. The skin right above the RIJV at the level of cricoid cartilage was selected, where a suture was fixed by using a needle to sew the skin with 20 cm long suture left outside. Cannulation was under real-time ultrasound visualization in the transverse plane, and the ends of suture were both wound around the left hand thumb of operator and were adhered closely to the middle of ultrasonic probe which pointed at the patient’s head side during catheterization. The force to drag the sutures was zero. A puncture needle (16 G, 20 cm, Lepu Medical Technology, Beijing, China) was inserted into the root of the sutures slowly under continuous negative pressure. The direction of the needle was 35-45º angle to the skin. During the needle insertion, the suture was straightened due to the down force of the needle. The CSA and AD of the RIJV was measured in triplicate. When the blood entered the needle, the needle was fixed and a guidewire was inserted. Only after that the guidewire was placed, the sutures and the ultrasonic probe were relaxed. After the success of RIJV catheterization, the suture should be adopted to fix the catheters. In group N, after the success of RIJV catheterization, the position of the suture should be selected to fix the catheter. The remaining procedures of the operations were the same as those in group T. In case that the right ICA was punctured in two groups, RIJV catheterization should be abandoned.
The age, gender, height and weight of patients were recorded. The following variables were recorded: hypotension and bradycardia during catheterization, CSA and AD of the RIJV at cricoid cartilage level both in the SP and in the LLP after anesthesia induction and during catheterization in the two groups patients, the number with obvious loss of resistance during catheterization, the number with easy aspiration of the blood into the syringe during needle insertion, the depth of needle insertion, catheterization time, the number of first pass punctures, the number of cannulations completed within 60 s, total success rate, complications such as pneumothorax, hemothorax, local hematoma and the number of cases with inadvertent arterial puncture.
Statistical analysis
Data values were presented as mean ± SD. One-way analysis of variance was used to compare variables between groups. If a significant difference was noted, Bonferroni multiple comparison test was used to evaluate the differences. P<0.05 indicated significance.
Results
General patient characteristics were similar between two groups (Table 1, P>0.05). In group N, two cases were excluded because of ICA puncture. Thus 68 patients were included in our study.
| Variables | Group N (n=33) | Group T (n=35) |
|---|---|---|
| Age (years) | 65.6 ± 12.4 | 64.8 ± 10.8 |
| Height (cm) | 168.5 ± 8.3 | 168.2 ± 7.8 |
| Weight (kg) | 61.6 ± 7.2 | 62.4 ± 7.4 |
| Gender (male/female) | 19/14 | 23/12 |
| ASA classification I/II/III | 16/12/15 | 17/15/3 |
| Data were expressed as mean ± SD or number of patients. ASA: American Society of Anesthesiologists. | ||
Table 1. General characteristics for all patients.
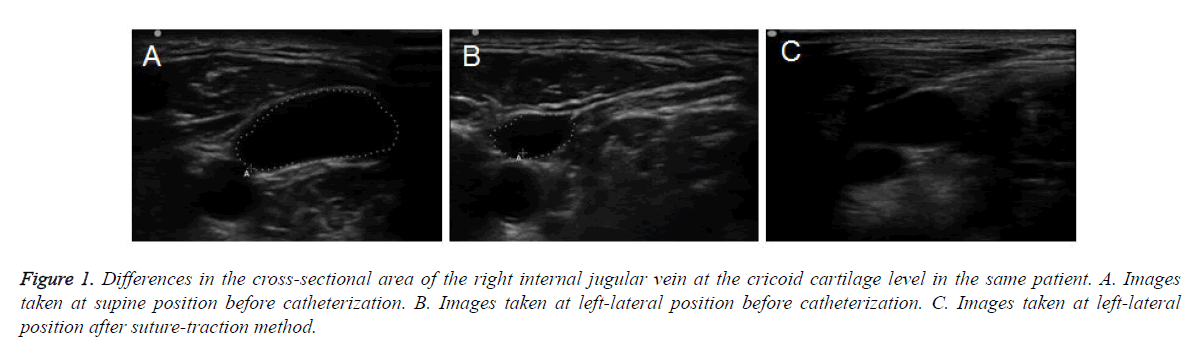
Compared to CSA and AD of RIJV in SP, CSA and AD of RIJV at cricoid cartilage level were smaller in LLP in two groups before catheterization (Table 2 and Figures 1A and 1B). Compared to CSA and AD of RIJV in SP, CSA and AD of RIJV at cricoid cartilage level were smaller in LLP during cannulations in Group N (P<0.01). Compared to CSA and AD of RIJV before cannulations, CSA and AD of RIJV at cricoid cartilage level were smaller in LLP during cannulations in Group N (P<0.05). Compared to CSA and AD of RIJV at cricoid cartilage level in SP, CSA and AD of RIJV at cricoid cartilage level was smaller in LLP during cannulations in Group T (P<0.05). However, they showed no differences in LLP before and during cannulation in Group T (P>0.05) (Figure 1C).
Figure 1. Differences in the cross-sectional area of the right internal jugular vein at the cricoid cartilage level in the same patient. A. Images taken at supine position before catheterization. B. Images taken at left-lateral position before catheterization. C. Images taken at left-lateral position after suture-traction method.
| Variables | Group N (n=33) | Group T (n=35) |
|---|---|---|
| CSA in SP before catheterization (cm2) | 1.03 ± 0.28 | 1.01 ± 0.31 |
| CSA in LLP before catheterization (cm2) | 0.53 ± 0.21★ | 0.52 ± 0.23★ |
| CSA in LLP during catheterization (cm2) | 0.24 ± 0.11##▲ | 0.55 ± 0.21★ |
| AD in SP before catheterization (cm2) | 0.88 ± 0.23 | 0.85 ± 0.25 |
| AD in LLP before catheterization (cm2) | 0.42 ± 0.13★ | 0.45 ± 0.14★ |
| AD in LLP during catheterization (cm2) | 0.22 ± 0.09##▲ | 0.52 ± 0.15★ |
| CSA: cross-sectional area. AD: anteroposterior diameter. Data were expressed as mean ± SD (n=3). ★P<0.05 compared to the value in SP before catheterization. ##P<0.01 compared the value in SP before catheterization. ▲P<0.05 compared to the value in LLP before catheterization. | ||
Table 2. CSA and AD of RIJV before and during catheterization.
Compared with patients in group N, the number with obvious loss of resistance, the number with easy aspiration of blood into syringe during needle insertion, the number of first pass punctures and the number of cannulations completed within 60 s increased significantly in group T (P<0.01). Compared with patients in group N, catheterization time was shortened significantly in group T (P<0.05). However, depth of needle insertion and total success rate were not significantly different (P>0.05, Table 3). There were two cases which were excluded the study because of ICA puncture in group N. There were no other complications in two groups.
| Outcomes | Group N (n=33) | Group T (n=35) |
|---|---|---|
| Obvious loss of resistance on venipuncture n (%) | 2 (6.1) | 28 (80.0)★ |
| Aspiration of blood into syringe during needle insertion n (%) | 5 (15.2) | 25 (71.4)★ |
| Depth of needle insertion, cm | 1.87 ± 0.25 | 1.93 ± 0.31 |
| Catheterization time, s | 243 ± 76 | 180 ± 68★★ |
| First pass punctures n (%) | 7 (21.2) | 23 (65.7)★ |
| Cannulations completed within 60s | ||
| n (%) | 5 (15.1) | 22 (62.9)★ |
| Data were expressed as mean ± SD, number (n) or percentage (%). ★P<0.01,★★P<0.05 compared to group N. | ||
Table 3. Puncture related information.
Discussion
When performing RIJV catheterization in LLP, the body position of the patients is different from that in routine position. Therefore, it is important to develop a method for conductive RIJV catheterization in LLP. In our study, lateral to the cricoid cartilage (often called the central) was selected for catheterization. Previous studies indicated that ultrasonicguided internal jugular vein catheterization increased success rate and reduced catheterization time and the complications [6-8]. Troianos et al. reported that the success rate of ultrasonic-guided central vein catheterization was 100% [9]. In this study, the success rate was 100% by STM in LLP, consistent with previously reported.
In our study, the sutures were tracted to the skin right above the RIJV under ultrasound. During catheterization, the sutures were placed close to the middle of the ultrasonic probe which pointed at the patient’s head. During catheterization, the needle tip was inserted down direction and the height of sutures and ultrasonic probe was kept unchanged. We found that the neck sutures tried to maintain the tissue position right above the RIJV. STM had the advantage of maintaining CSA and AD of RIJV. In this way, there was obvious loss of resistance when the anterior wall of RIJV was perforated, which indicated that AD of RIJV was still long enough. Having several advantages due to extravascular negative force to maintain RIJV, STM facilitated catheterization and shortened catheterization time.
In our study, the sectional areas of RIJV at the cricoid cartilage level in LLP were smaller than that in SP in two groups. The main reason may be that RIJV was oppressed by the neck muscle and flatted due to the straightening of RIJV itself when the head was turned to the left. The perforation of the posterior vessel wall still occurred even when venipuncture was guided by ultrasound [10]. Koich et al. found that the blood was aspirated into the syringe during a 16 G needle insertion only in 42.6% patients [11]. However, in our study the sutures were used to skin traction beforehand and the blood was aspirated in 71.4% patients, which implied that only the anterior vascular wall was perforated. In addition, we found sudden loss of resistance in 80.0% patients during venipuncture, which also suggested that only the anterior vascular wall was perforated. STM made RIJV less prone to indentation when the puncture needle was inserted, and as a result the puncture needle was more likely to perforate the vessel wall without overshoot.
It was suggested that the bigger the overlap area of the ICA covered by RIJV, the higher the probability of ICA puncture [12,13]. In our study, ICA was totally overlapped by RIJV. However, there was no significant difference in the probability of ICA puncture. We found that the posterior vascular wall was not easy to be perforated using STM, which prevented the puncture needle from touching ICA. This may be also associated with real-time ultrasonic-assisted guidance catheterization techniques which help observe the tip of the needle.
Verghese et al. found that carotid artery palpation and the cannulation needle insertion could make the internal jugular vein collapse [14,15]. In our study, we found that the internal jugular vein under the needle stem was collapsed in group N, but it was unchanged due to the suture traction during the needle advance in group T. The anterior walls in the needle tip direction in two groups were extruded to be collapsed by the needle. We found no difference in the depth of cannulation needle insertion in two groups. However, AD of RIJV in group T was wider than that in group N. Therefore, we speculated that the probability of ICA puncture in group N was higher than that in group T.
Sasano et al. developed a novel Skin-Traction Method (STM) in which the puncture point of the skin over the IJV was stretched upwards with several pieces of surgical tape in the cephalad and caudal directions to facilitate IJV catheterization [4]. Their method increased the compressive force required to collapse the IJV, and maintained the CSA of the vein during real-time ultrasound-assisted guidance, but their method was only tested in 10 samples and there was no implementation of ultrasound-guided venipuncture. Thus the clinical value of the method remains to be tested. Previously we developed a Puncture Point-Traction Method (PPTM) to facilitate RIJV cannulation, we retained the puncture point of the skin directly above the RIJV in its original position by the traction of surgical suture [16]. PPTM method facilitated the catheterization of RIJV and improved the success rate of RIJV catheterization in anesthetized patients in the supine position [16]. However, it is known that it is easy to puncture when patients are at supine position. In the clinical, some patients need RIJV catheterization in LLP and PPTM is not practical. Therefore, in this study we developed STM, in which the puncture point of the skin right above the RIJV is fixed in original position by suture “traction”. STM not only maintains the vein size but also prevents the vein from collapse during catheterization. STM facilitates RIJV and increases the success rate of RIJV catheterization even in LLP in anesthetized patients.
In our experience, one surgeon helped pass the ultrasonic probe with ultrasonic coupling agent and inserted a guidewire while the other performed the operations. We found that the guidewire could not be inserted into RIJV sometimes if the sutures were relaxed before guidewire insertion. We speculated that the distance of needle insertion into RIJV was short. When the sutures were relaxed, the traction of cervical tissue disappeared and the tip of the needle was out of the vein. To prevent this, we would not relax the sutures until the guidewire had been inserted into RIJV.
This study has some limitations. First, RIJV catheterization using our method needs good preparation before the surgery. Second, our method could only be performed by experienced anesthesiologist. Third, our sample size is small. The clinical value of our method needs need to be confirmed in multicenter studies with large sample size. Despite these limitations, our study suggests that STM is a novel method that facilitates RIJV and increases the success rate of RIJV catheterization in LLP in anesthetized patients.
Conflict of Interest
No
References
- Fathi M, Izanloo A, Jahanbakhsh S. Central venous cannulation of the internal jugular vein using ultrasound-guided and anatomical landmark techniques. Anesth Pain Med 2016; 6: 35803.
- Aoyama K, Takenaka I, Iwagaki T, Sano H. A simple maneuver for confirmation of the guidewire during ultrasound-guided internal jugular vein cannulation. Can J Anaesth 2015; 62: 839-840.
- Treglia A, Musone D, Amoroso F. Retrospective comparison of two different approaches for ultrasound-guided internal jugular vein cannulation in hemodialysis patients. J Vasc Access 2017; 18: 43-46.
- Sasano H, Morita M, Azami T. Skin-traction method prevents the collapse of the internal jugular vein caused by an ultrasound probe in real-time ultrasound-assisted guidance. J Anesth 2009; 23: 41-45.
- Redo SF. Modified catheter for prolonged central venous use. J Pediatr Surg 1995; 30: 1544-1545.
- Lau CS, Chamberlain RS. Ultrasound-guided central venous catheter placement increases success rates in pediatric patients: a meta-analysis. Pediatr Res 2016; 80: 178-184.
- Wu SY, Ling Q, Cao LH, Wang J, Xu MX. Real-time two-dimensional ultrasound guidance for central venous cannulation: a meta-analysis. Anesthesiology 2013; 118: 361-375.
- Alagoz A, Tunc M, Sazak H. Absence of the right internal jugular vein during ultrasound-guided cannulation. J Biomech 2015; 48: 1852-1859.
- Troianos CA, Jobes DR, Ellison N. Ultrasound-guided cannulation of the internal jugular vein. A prospective, randomized study. Anesth Analg 1991; 72: 823-826.
- Blaivas M, Adhikari S. An unseen danger: frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. Crit Care Med 2009; 37: 2345-2349.
- Maruyama K, Nakajima Y, Hayashi Y, Ohnishi Y, Kuro M. A guide to preventing deep insertion of the cannulation needle during catheterization of the internal jugular vein. J Cardiothorac Vasc Anesth 1997; 11: 192-194.
- Kim W, Mi S, Choi S. Optimal head rotation and puncture site for internal jugular vein cannulation after laryngeal mask airway insertion. Singapore Med J 2015; 56: 472-478.
- Deangelis V, Denny J, Chyu D. The optimal angle of head rotation for internal jugular cannulation as determined by ultrasound evaluation. J Cardiothoracic Vasc Anesth 2015; 29: 1257-1260.
- Airapetian A, Maizel J, Langelle F. Ultrasound-guided central venous cannulation is superior to quick-look ultrasound and landmark methods among inexperienced operators: a prospective randomized study. Intensive Care Med 2013; 39: 1938-1944.
- Shrestha GS, Gurung A, Koirala S. Comparison between long- and short-axis techniques for ultrasound-guided cannulation of internal jugular vein. Ann Card Anaesth 2016; 19: 288-292.
- Wu T, Zang H. Puncture point-traction method: A novel method applied for right internal jugular vein catheterization. Exp Ther Med 2016; 12: 307-311.