Research Article - The International Tinnitus Journal (2020) Volume 24, Issue 1
Upper Cervical Nerves Can Induce Tinnitus
Department of Pain Therapy Pain Clinic De Bilt, Groenkanseweg Bilt, The Netherlands
*Send correspondence to: Henk M Koning, Department of Pain Therapy Pain Clinic De Bilt, Netherlands, E-mail: hmkoning@pijnkliniekdebilt.nl, Phone: +0031302040753
Paper submitted on April 06, 2020; and Accepted on May 02, 2020
Citation: Upper Cervical Nerves Can Induce Tinnitus. 24(1):26-30.
Abstract
Introduction: Treating cervical spine disorders can result in a reduction of tinnitus
Objectives: The object of the study was to ascertain the benefit of therapy of the third and fourth cervical nerves in reducing tinnitus and to assess parameters indicating a long-term relief.
Design: Subjects were 37 tinnitus patients who were treated with infiltration of the third and fourth cervical nerves. Clinical data form these patients were reviewed retrospectively. An independent perceiver evaluated the long-term effect of the therapy by telephone interview.
Results: In a group of tinnitus patients, 19% of the patients reported less tinnitus after therapy of the third and fourth cervical nerves. Most of the patients had a moderate reduction of 25% to 50%. At 3.8 months, 50% of the successful treated patients still had a positive effect. No adverse events of the procedure were observed. The combination of an evident anterior spur at the third cervical vertebrae together with less hearing at 2 kHz indicate patients who responded the best to therapy of the third and fourth cervical nerves.
Conclusions: Treating cervical spine disorders can reduce tinnitus. In a group of tinnitus patients, 19% of the patients had less tinnitus after therapy of the C3 and C4. Screening of tinnitus patients is needed for the proper selection of the ones who could benefit from a somatic approach. In our study, the combination of an evident anterior spur at the third cervical vertebrae together with less hearing at 2 kHz indicate patients who responded the best following therapy of the C3 and C4
Keywords
Tinnitus, nerve root infiltration, third cervical nerve, fourth cervical nerve, cuneate nucleus, cochlear nucleus, cervical spine, hearing loss.
Introduction
Somatosensory input to the auditory nuclei may cause neuronal activity in auditory pathways, which may be perceived as tinnitus [1, 2]. Therefore, treating cervical spine disorders can result also in a reduction of tinnitus [3, 4]. Screening of tinnitus patients is needed for the proper selection of the ones who could benefit from a somatic approach. The object of the study was to ascertain the benefit of therapy of the third (C3) and fourth (C4) cervical nerves in reducing tinnitus and to assess parameters indicating a long-term relief.
Materials and Methods
Subject: The Medical research Ethics Committees United (Nieuwegein, the Netherlands) sanctioned the study. A patient chart review selected all patients who had infiltration of the C3 and C4 in an interval between October 2016 to October 2019. Exclusion criteria were tinnitus lasting less than 1 month. The corner between the posterior boundary of the cervical vertebrae, the disc height, and the proportions of the anterior spur were measured from the cervical spine radiograph, as previously described [5].
Infiltration of the cervical nerves: The procedure of infiltration of the C3 and C4 was executed with the patient lying face upward. The X-ray beam was moved from a lateral to oblique position to visualize the neural foramina at its largest dimension. The levels of the foramen of the C3 and C4 were marked and used as the access of the needles. After decontamination of the skin, two 23-gauge needles (Top Neuropole needle XE-S, Tokyo, Japan) were inserted and positioned as a point at the foramen of C2-C3 and C3-C4. With an anteroposterior radiographic projection, the needles were moved forward until they were at the foraminal canal at C2-C3 and C3-C4, and halfway across the facet joint line. Under fluoroscopic guidance, 0.5 ml Iohexol (Omnipaque 240, Eindhoven, and the Netherlands) was instilled to see the contrast at the nerves. If the needles were at the correct places and there was no blood on aspiration, a mixture of 1 ml bupivacaine 0.5% (Bupivacaine Aurobindo, Baarn, and the Netherlands) and 0.5 ml dexamethasone (Dexamethasone CF, Etten- Leur, the Netherlands) was instilled. The patients were reassessed 7 weeks postoperative.
Data Assessment: Data were recorded from the patient charts, including the self-reported benefit 7 weeks postoperative on a 4-point Likert scale (none [0%], slight [less than 25%], moderate [25% to 50%], good [50% or more]), and the interval of relief. Further treatment of tinnitus was resumed at 7 weeks postoperative when required. If the patient noticed an improvement of their tinnitus, the period of relief from the first treatment up until the consecutive treatment was recorded. All patients with less tinnitus following infiltration of C3 and C4, and without a reported relapse, were incorporated for an evaluation by questionnaire. In December 2019, an independent perceiver had a telephone interview with the patients, using a standardized question sheet to estimate the interval of relief.
Statistical Methods: Univariate and multivariate statistical analyses were executed with Minitab 18 (Minitab Inc., State College, PA, USA). The period of relief following treatment was studied using survival analysis techniques. Multiple regression analysis was used to obtain a model to tell in advance a successful effect on tinnitus at 7 weeks postoperative.
Results
During a three-year period, 37 tinnitus patients were subjected to an infiltration of C3 and C4. The features of the patients are visible in (Table 1). Seven patients (19%) noticed less tinnitus. The amount of relief was rated as good for 14% and as moderate for 86% of the patients. No adverse effects of the procedure were reported at follow-up.
| Prevalence | Median | Q1 – Q3 | |
|---|---|---|---|
| Age (year) | 60.0 | 52.0 – 66.0 | |
| Gender (male) | 70% | ||
| Unilateral tinnitus | 43% | ||
| Self-perceived hearing loss | 65% | ||
| Cervical pain | 68% | ||
| Period of tinnitus (year) | 10.0 | 1.5 – 19.0 | |
| Hearing loss (dB) at: | |||
| 250 Hz | 15.0 | 10.0 - 36.3 | |
| 500 Hz | 15.0 | 10.0 – 42.5 | |
| 1 KHz | 15.0 | 10.0 – 40.0 | |
| 2 KHz | 25.0 | 12.5 – 35.0 | |
| 4 KHz | 40.0 | 21.5 – 56.5 | |
| 8 KHz | 51.5 | 25.0 – 76.0 |
dB: decibel; Hz: Hertz; KHz: Kilohertz;Q1 – Q3: Inter-Quartile Range.
Table 1: Clinical characteristics of the patients with tinnitus.
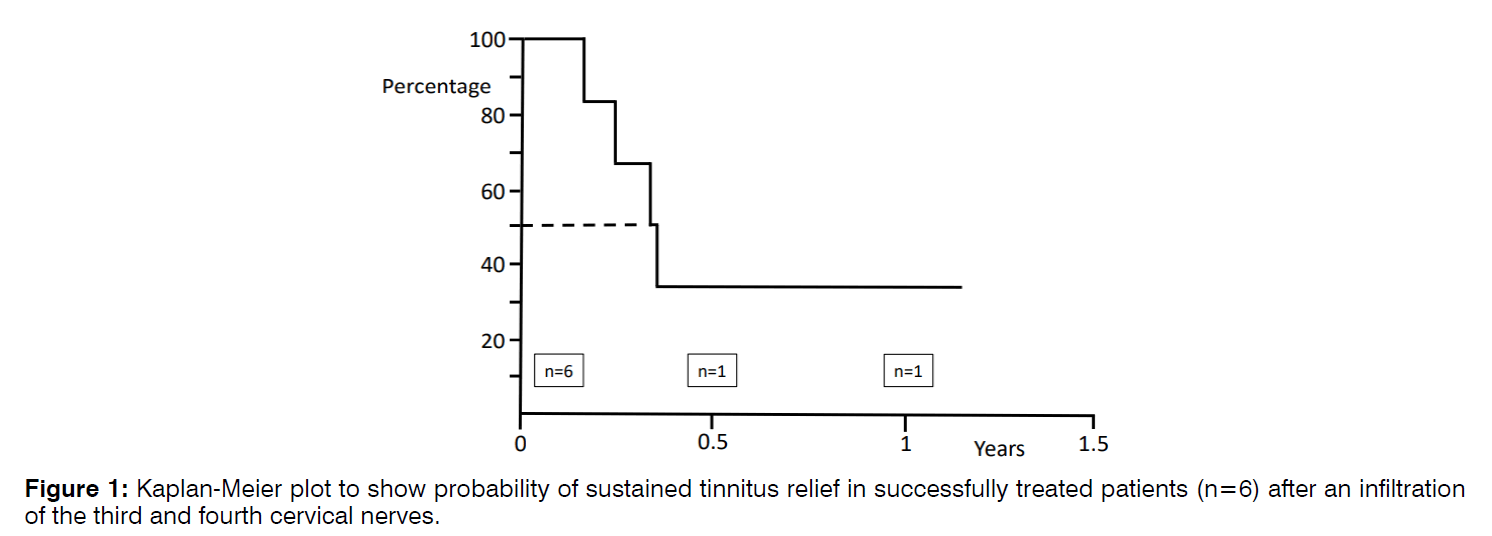
Figure 1 shows a Kaplan–Meier plot of the likelihood of permanent relief after successful therapy of C3 and C4 in patients suffering from tinnitus. At 3.8 months, 50% of the patients still had a benefit up to this time. Patients with less tinnitus following infiltration of C3 and C4 were compared with patients not reacting to therapy (Table 2). The existence of cervical pain was linked to a positive effect of infiltration of C3 and C4 on tinnitus.
| Positive effect of therapy of C3 and C4 (n=7) | No effect of therapy of C3 and C4 (n= 30) | P-value | |||||
|---|---|---|---|---|---|---|---|
| Prev. | Mean | SEM | Prev. | Mean | SEM | ||
| Gender (male) | 71% | 70% | 0.94 | ||||
| Unilateral tinnitus | 29% | 47% | 0.384 | ||||
| Self-perceived hearing loss | 71% | 63% | 0.682 | ||||
| Cervical pain | 100% | 60% | 0.042 | ||||
| Age at the start of tinnitus (year) | 49.3 | 5.1 | 45.5 | 2.7 | 0.526 | ||
| Hearing loss (dB) at: | |||||||
| 250 Hz | 31.4 | 9.9 | 24.8 | 4.3 | 0.556 | ||
| 500 Hz | 30.0 | 11 | 24.5 | 4.0 | 0.663 | ||
| 1 KHz | 31.4 | 12 | 24.7 | 4.1 | 0.605 | ||
| 2 KHz | 39.3 | 11 | 25.6 | 3.5 | 0.264 | ||
| 4 KHz | 46.4 | 11 | 42.1 | 4.6 | 0.721 | ||
| 8 KHz | 57.1 | 12 | 51.6 | 6.0 | 0.691 | ||
| Angle between vertebrae C2 and C6 (degrees) | 7.9 | 3.1 | 5.4 | 1.9 | 0.520 | ||
| Farfan’s measurement of disc space height (%) | |||||||
| C2-C3 | 44 | 2.9 | 41 | 1.5 | 0.359 | ||
| C3-C4 | 33 | 4.7 | 37 | 1.6 | 0.451 | ||
| C4-C5 | 36 | 3.6 | 35 | 1.9 | 0.757 | ||
| C5-C6 | 30 | 4.6 | 28 | 1.8 | 0.768 | ||
| C6-C7 | 31 | 3.0 | 26 | 1.6 | 0.171 | ||
| Size of anterior spur (%) at: | |||||||
| C3 | 10 | 2.4 | 5 | 1.0 | 0.108 | ||
| C4 | 9 | 1.2 | 12 | 1.9 | 0.284 | ||
| C5 | 19 | 2.4 | 16 | 1.5 | 0.299 | ||
| C6 | 12 | 1.6 | 14 | 1.5 | 0.577 | ||
dB: decibel; Hz: Hertz; KHz: Kilohertz; SEM: Standard Error of the Mean; Sign: Significant; Prev.: Prevalence.
Table 2. Patients with a positive effect of therapy of C3 and C4 on their tinnitus at 7 weeks were compared with non-responders.
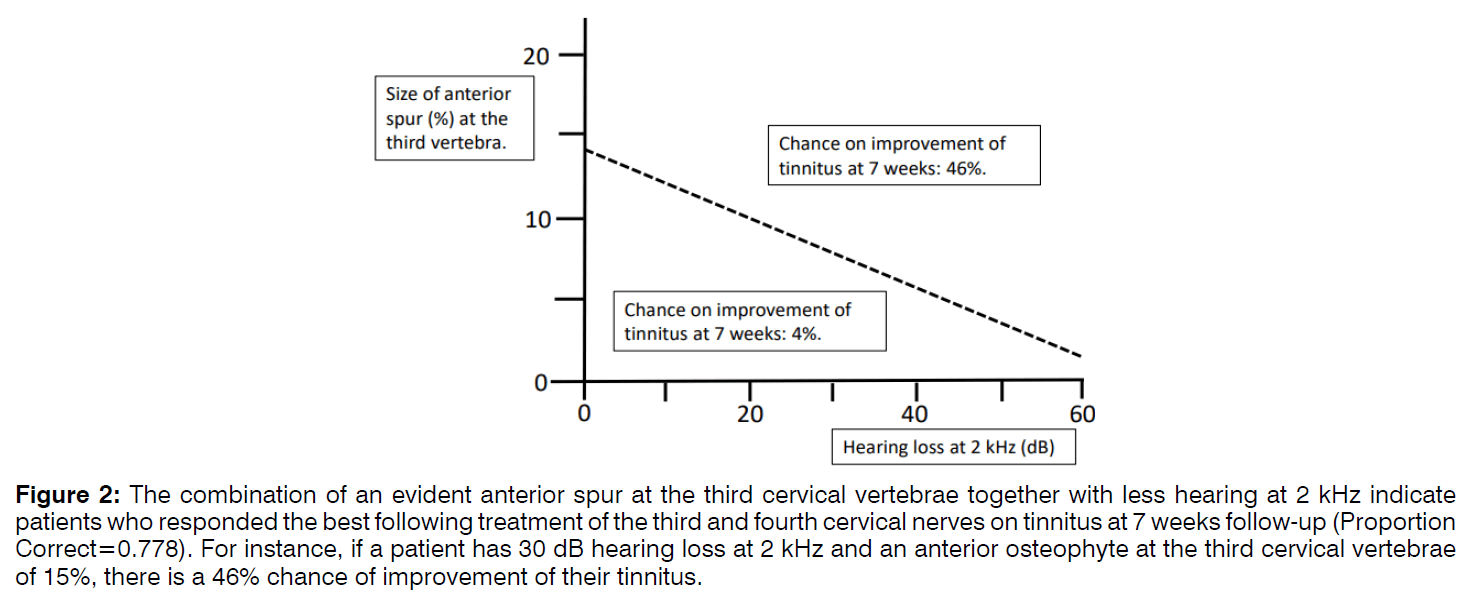
Multivariate statistical analysis pointed out that the combination of less hearing at 2 kHz and the magnitude of the anterior spur at the third vertebrae predicted a good result of the infiltration of C3 and C4 on tinnitus at 7 weeks. With discriminant analysis, patients with more chance for a successful infiltration of C3 and C4 were identified (Figure 2). Of these patients, 46% had less tinnitus at 7 weeks postoperative. The specifications used in Figure 2 have a sensitivity of 86% and a specificity of 76% in foretelling a good response to infiltration of the C3 and C4 in tinnitus patients. The positive and negative predictive values were 86% and 96% respectively.
Figure 2: The combination of an evident anterior spur at the third cervical vertebrae together with less hearing at 2 kHz indicate patients who responded the best following treatment of the third and fourth cervical nerves on tinnitus at 7 weeks follow-up (Proportion Correct=0.778). For instance, if a patient has 30 dB hearing loss at 2 kHz and an anterior osteophyte at the third cervical vertebrae of 15%, there is a 46% chance of improvement of their tinnitus.
Discussion
In a group of tinnitus patients, 19% of the patients reported less tinnitus after therapy of C3 and C4. Most of the patients had a moderate reduction of 25% to 50%. At 3.8 months, 50% of the successfully treated patients still had a positive effect. No adverse effects of the procedure were observed.
Somatic disorders of the cervical spine can be related to tinnitus and these forms of tinnitus are known as "somatosensory tinnitus"2. The somatosensory nervous system is a source of non-auditory inputs to auditory nuclei6. Different cervical nerves can induce tinnitus and it is difficult to find out which specific cervical nerve is responsible for the tinnitus in each patient4. In our study, therapy of the C3 and C4 in a group of tinnitus patients indicates that only a remote part (19%) reacted with a moderate downgrading of their tinnitus for a short period.
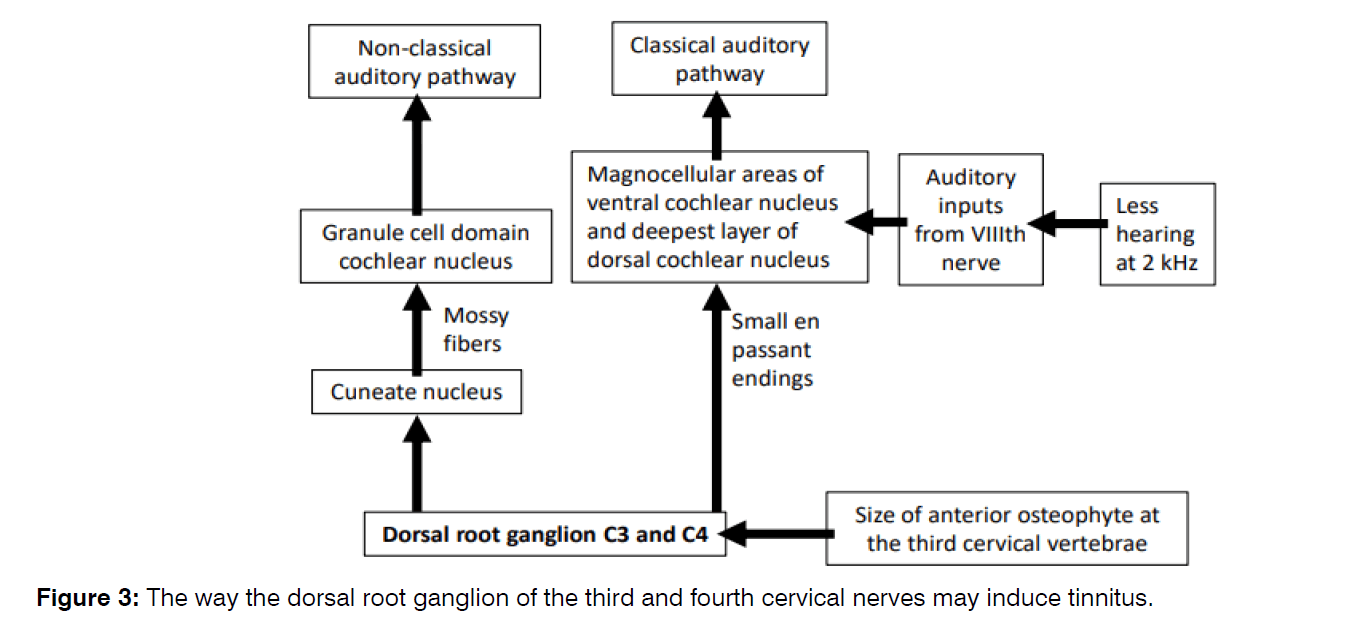
Auditory-somatosensory bimodal integration is present in the auditory nuclei. A disbalance between auditory and somatosensory inputs can provoke tinnitus [6]. Somatosensory input to the Cochlear Nucleus (CN) may modulate excitability in central auditory pathways and also auditory nerve denervation can enhance the somatosensory impact on the auditory system6. In our study, the combination of an evident anterior spur at the third cervical vertebrae together with less hearing at 2 kHz indicate patients who responded the best following infiltration of the C3 and C4.
There are two separate somatosensory tracts from the Dorsal Root Ganglia (DRG) to the CN (Figure 3) [2-6]. A slow direct pathway characterized by small bouton endings and a wide distribution in the CN, and a fast indirect pathway to the cuneate nucleus and then by mossy fibres to the granule cell area of the CN. The granule cell area is regarded as part of the extralemniscal system [2]. Heavy projections to the cuneate nucleus originated from the C2, C7, and C8 DRG, whereas those from the other cervical DRG are less extensive [7]. The projections to the cuneate nucleus from the different DRG appeared to overlap. It is unknown whether information of the DRG of C3 and C4 is preferentially transmitted by the direct or indirect somatosensory pathways to the CN.
Secondary tinnitus may develop owing to altered geometry, functional disorders, or morphological disorders of the cervical spine [8, 9]. In our study, tinnitus patients who responded to therapy of C3 and C4 had more degeneration at disc C3-C4 and larger anterior spur at the third cervical vertebrae, although it was not statistically significant. These degenerative changes are capable to stimulate C3 and C4. However, whether these degenerative changes can also because tinnitus depends of the presence of auditory deprivation.
An elevation of the somatosensory impact on auditory neurons is observed when the auditory input is hampered [2]. Damage to outer hair cells could preferentially affect those fusiform cells in the dorsal CN that indirectly receive somatosensory input via the granule cell/parallel fibre system10. Thus, tinnitus may be induced by a group of neurons, who become more reactive to somatosensory input following cochlear damage6. In our study, the disbalance of input from the auditory and somatosensory nervous system was associated to less hearing at 2 kHz. Further studies are needed to find out which conditions of auditory deprivation affect bimodal integration at the cochlear nucleus.
The findings of our study are limited due to its retrospective design, and the number of patients. A prospective study is needed with more patients included.
Conclusion
Treating cervical spine disorders can reduce tinnitus. In a group of tinnitus patients, 19% of the patients had less tinnitus after therapy of the C3 and C4. Screening of tinnitus patients is needed for the proper selection of the ones who could benefit from a somatic approach. In our study, the combination of an evident anterior spur at the third cervical vertebrae together with less hearing at 2 kHz indicate patients who responded the best following therapy of the C3 and C4.
Conflict of Interest
The authors declare no potential conflict of interest on publishing this paper.
References
- Roberts LE, Eggermont JJ, Caspary DM, Shore SE, Melcher JR, Kaltenbach JA. Ringing Ears: The Neuroscience of Tinnitus. J Neurosci. 2010;30:4972-9.
- Dehmel S, Cui YL, Shore SE. Cross-modal interactions of auditory and somatic inputs in the brainstem and midbrain and their imbalance in tinnitus and deafness. Am J Audiol. 2008;17:193-209.
- Koning HM, Dyrbye BA, van Hemert FJ. Percutaneous radiofrequency lesion of the superior cervical sympathetic ganglion in patients with tinnitus. Pain Practice. 2016;16:994-1000.
- Koning HM, Ter Meulen BC. Pulsed radiofrequency of C2 dorsal root ganglion in patients with tinnitus. Int. Tinnitus J. 2019;23:91-6.
- Koning HM, Koning MV, Koning NJ, Ter Meulen BC. Anterior Cervical Osteophytes and Sympathetic Hyperactivity in Patients with Tinnitus: Size Matters. Int. Tinnitus J. 2018;22:97-102.
- Shore SE. Plasticity of somatosensory inputs to the cochlear nucleus--implications for tinnitus. Hear Res. 2011;281:38-46.
- Arvidsson J, Pfaller K. Central projections of C4-C8 dorsal root ganglia in the rat studied by anterograde transport of WGA-HRP. J Comp Neurol. 1990;292:349-63.
- Montazem A. Secondary tinnitus as a symptom of instability of the upper cervical spine: operative management. Int Tinnitus J. 2000;6:130-3.
- Hölzl M, Behrmann R, Biesinger E, van Heymann W, Hülse R, Goessler UR, et al. Selected ENT symptoms in functional disorders of the upper cervical spine and temporomandibular joints. HNO. 2019;67:1-9.
- Shore SE, Koehler S, Oldakowski M, Hughes LF, Syed S. Dorsal cochlear nucleus responses to somatosensory stimulation are enhanced after noise-induced hearing loss. Eur J Neurosci. 2008;27:155-68.